CASE PRESENTATION
A 62-year-old woman presents with significant nuclear sclerosis. Thirty years ago, the patient underwent bilateral centripetal radial keratotomy (RK), developed and popularized in Russia, with a small optical zone.
Her current refraction is +6.00 +1.50 x 170º OD and +6.50 +1.25 x 030º OS. She has a history of successful contact lens wear. Recently, however, she developed contact lens intolerance, and her BCVA decreased to 20/40 OD (20/60 with glare) and 20/50 OS (20/80 with glare).
A slit-lamp examination of each eye finds a 3-mm optical zone and eight RK incisions that extend to the limbus. Both eyes have 2+ nuclear sclerosis, 1+ cortical changes, and a trace posterior subcapsular cataract.
Mild dry eye disease in both eyes has responded to topical therapy with cyclosporine ophthalmic emulsion 0.05% (Restasis, Allergan/AbbVie), low-level light therapy, and occlusion of the lower puncta. The patient nevertheless continues to experience marked vision fluctuation from morning to evening. CXL was proposed to treat the patient’s fluctuating vision, but she declined the offer.
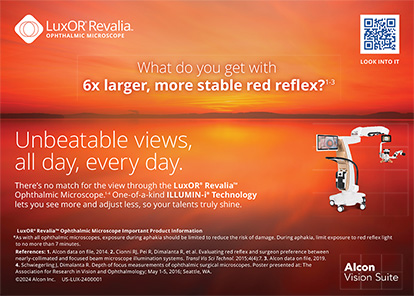
Diagnostic testing finds higher-order corneal aberrations of 0.448 OD and 0.701 OS and corneal asphericity values of +3.13 OD and +4.12 OS. Corneal astigmatism measures +1.28 D @ 170º OD and +2.19 D @ 012º OS. From morning to evening, the average corneal power fluctuates 0.75 D and 0.50 D in the right and left eyes, respectively (Figures 1–3). The average IOL powers are greater than 30.00 D with the ASCRS formula for prior RK.
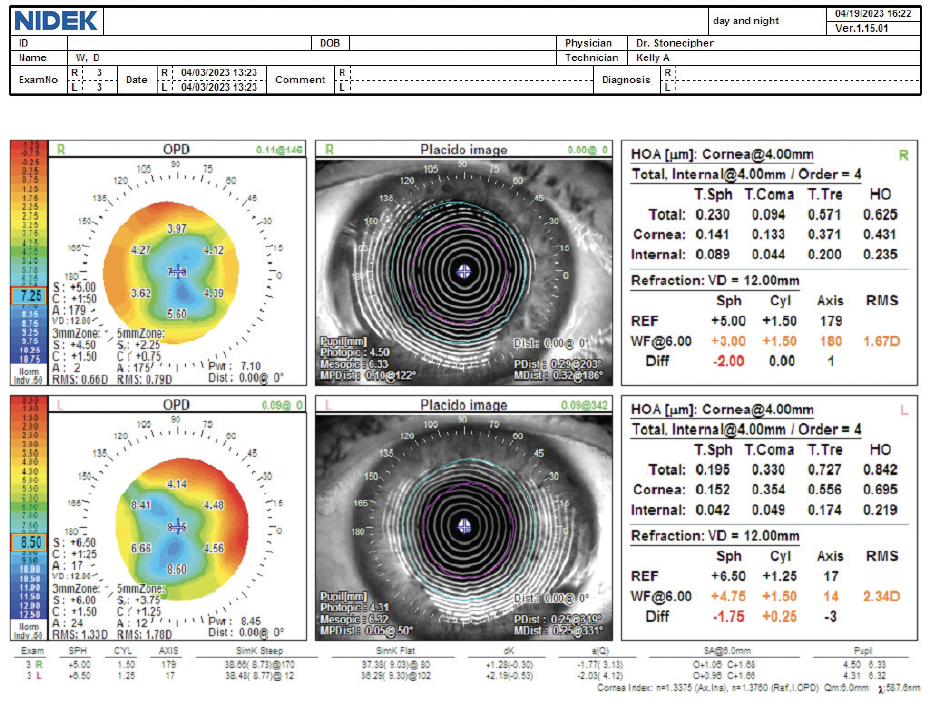
Figure 1. Day and night refractions of both eyes with the OPD-Scan III.
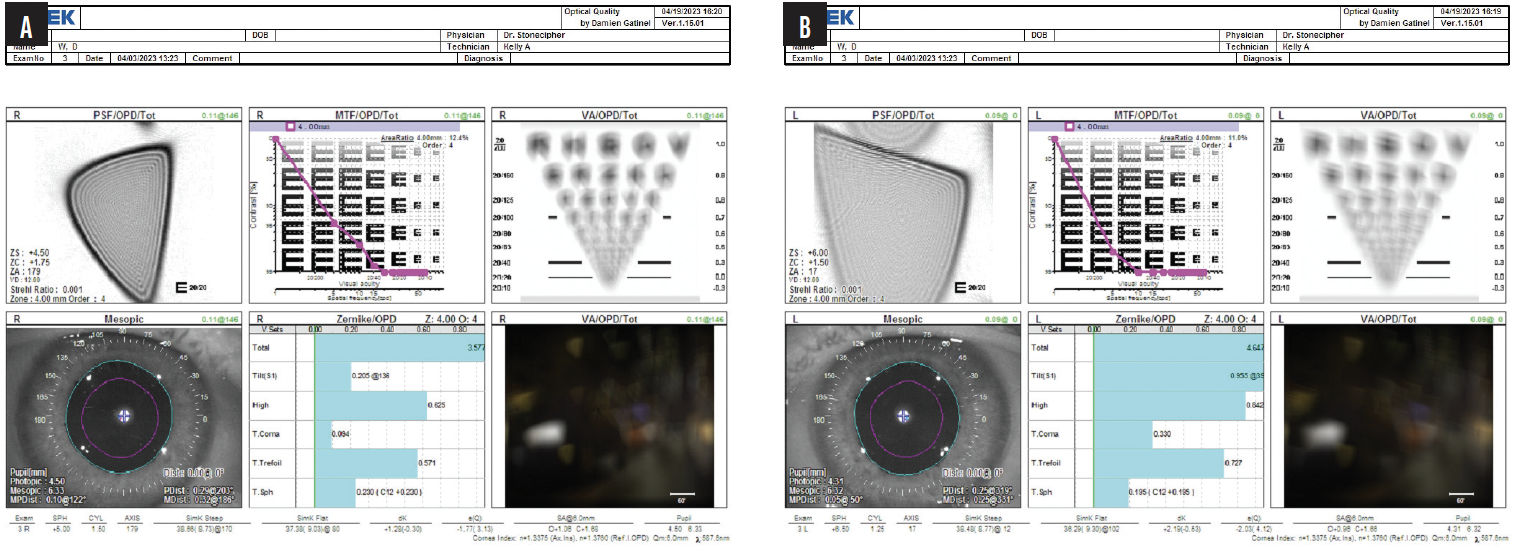
Figure 2. Optical quality by Damien Gatinel, MD, PhD, for the right (A) and left (B) eyes.
Figure 3. Overview with the OPD-Scan III for the right (A) and left (B) eyes.
The patient asks what her surgical options are. How would you proceed?
—Case prepared by Karl G. Stonecipher, MD

BLAKE K. WILLIAMSON, MD, MPH, MS
This is an extremely challenging case. Lengthy informed consent is the first step. The goal here is maximal function, not perfection. It is important the patient understand that, no matter the surgical intervention, she will likely continue to experience fluctuating vision. If she is truly contact lens intolerant, even with a perfectly fitting scleral lens, she will need to wear spectacles for optimal vision.
I would not perform PRK. I would evaluate tomography and her previous refractions for ectasia and perform CXL if indicated before proceeding to cataract surgery. If CXL is not an option, my first choice would be bilateral implantation of an IC-8 Apthera (Bausch + Lomb). I typically place this IOL in patients’ nondominant eye and avoid bilateral implantation because doing so can dim vision. Patients like this one, however, are sometimes willing to accept dimming in exchange for the improvement in vision achieved with pinhole optics.
This patient requires a higher-powered IC-8 than is currently available. She must therefore be willing to wear spectacles or scleral lenses after surgery. That said, I have been pleasantly surprised at how forgiving the IC-8 can be. Some of my patients with complex corneas whom I expected to have a high residual refractive error after IC-8 implantation ended up with little ametropia.

JEFFREY WHITMAN, MD
Central keratometry values such as average pupil power with the OPD-Scan III (Nidek) or effective refracting power with the Holladay IOL Consultant (Holladay Consulting) would be obtained. This information, topographic keratometry readings, and axial length would be entered into the Holladay 2 formula, which I have found to be highly accurate in patients who have a history of RK.
In my experience, CXL has not been effective at achieving refractive stability in post-RK eyes, so I would not perform the procedure here.
I would choose the maximum available power (30.00 D) of either a Light Adjustable Lens (LAL; RxSight) or IC-8 Apthera lens. Power could be increased an additional 3.00 D with light treatment of the LAL, which should give the patient functional vision. Either a piggyback lens could be implanted in the sulcus or an EVO ICL (STAAR Surgical) could be placed over the LAL after the lock-in treatment to fine-tune her vision further if necessary. Alternatively, implantation of a 30.00 D IC-8 would likely reduce vision fluctuation. Even if the -0.75 D refractive target is missed with the IOL in an irregular eye, the small-aperture optics often yield satisfactory vision. Placement of a piggyback lens over the IC-8 could be considered as well.

WHAT I DID: KARL G. STONECIPHER, MD
The patient and I thoroughly discussed her options. Preoperative biometry indicated that 31.00 and 32.00 D IC-8 Apthera IOLs would achieve an emmetropic result in the right and left eyes, respectively. Although this IOL is not currently available in powers higher than 30.00 D, we decided it was the best option for reducing the aberrations caused by the RK procedures. As mentioned earlier, the patient was not interested in undergoing CXL.
Near-clear corneal incisions were created with a 3-mm metal blade to avoid intersection with the RK incisions because a 3-mm incision is required for insertion of an IC-8 lens. A blue sleeve was used on the Centurion Vision System (Alcon) to guard against wound leakage.
Four weeks after surgery, the patient’s UCVA was 20/32 OU, 20/50 OD, and 20/32 OS. Her uncorrected near visual acuity was 20/40 OU. The plan is to wait until refractive stability is achieved before determining how best to address her residual refractive error. At the time of this writing, the patient is happy with her outcome and has decided not to obtain a pair of temporary glasses.