I have a private clinic in Andorra. Even in routine cases, most of my patients opt for laser cataract surgery. I begin the interventions with the Lensar Laser System (Lensar), as you can see in my accompanying Eyetube video (bit.ly/hanneken0220). I use the laser to create the capsulotomy and to perform nucleus fragmentation; the video shows the grid pattern created in the nucleus by the femtosecond laser. I find it useful, especially in tricky situations, such as an eye with a shallow anterior chamber or hard nucleus, to use the femtosecond laser for these two steps.
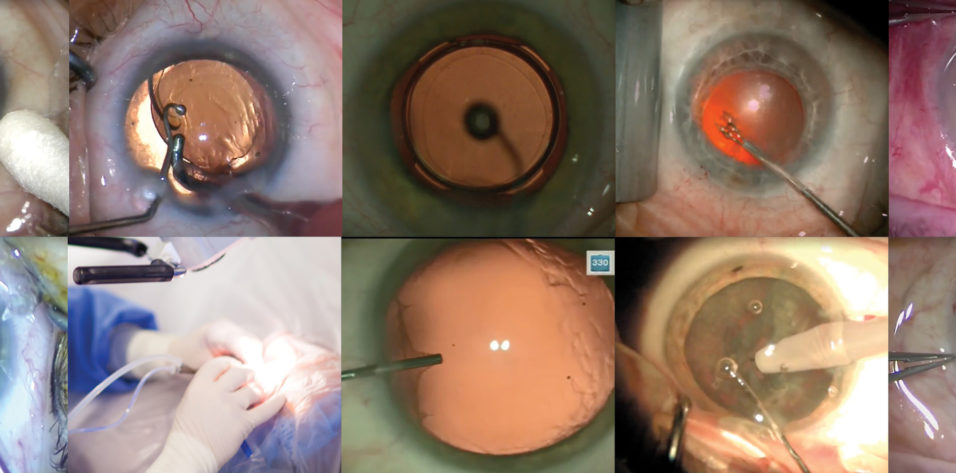
After the laser part of the surgery is complete, I use an angled 2.0/2.2-mm trapezoidal knife (SUB7601, Bausch + Lomb) to create the main incision, and I usually use the same knife also for my two paracenteses, which I make about 30° on either side of the main incision (Figure 1).
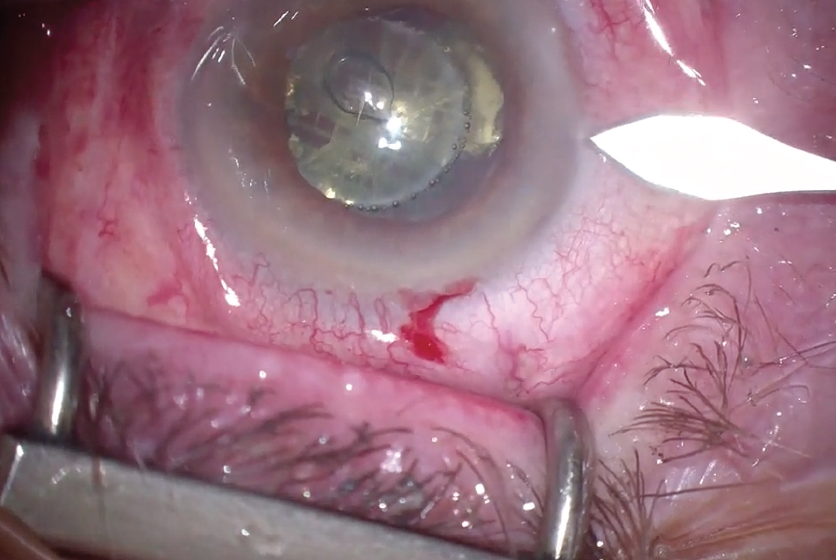
Figure 1. An angled 2.0/2.2-mm trapezoidal knife is used to create a paracentesis about 30° from the main incision. Note the laser fragmentation pattern in the nucleus.
In the case in my video, because the pupil is small, I inject additional epinephrine to get better dilation and guard against intraoperative floppy iris syndrome. I then inject a sodium hyaluronate OVD, usually Amvisc (Bausch + Lomb), followed by the completion of thorough hydrodissection of the nucleus.
The operating microscope I use is an older Leica model with which I'm still very happy. The phaco machine is a Stellaris Vision Enhancement System (Bausch + Lomb), which I have also been using for many years. This video was recorded with a 4K camera from Enciris Technologies, a French company.
CHOPPING TECHNIQUE
I use a chopping technique for nucleus division, relying on the Koch Chopper (Bausch + Lomb) as my second instrument. The fragmentation pattern achieved with the femtosecond laser makes chopping a lot easier. As you can see in the video, even with a small pupil, I can easily divide and aspirate the nucleus. Nearly all the nucleus can be aspirated without any additional phaco energy.
Prefragmenting the nucleus with the femtosecond laser frequently allows me to use only aspiration without moving the phaco handpiece in the eye very much (Figure 2). Sometimes to save time I use the phaco handpiece in I/A mode for aspiration of thick cortical masses, before switching over to bimanual irrigation and aspiration.
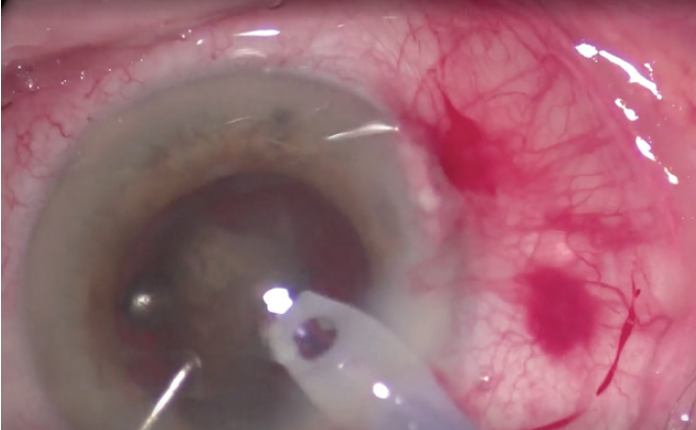
Figure 2. The nucleus can be aspirated with little use of phaco energy.
The separation of irrigation and aspiration into bimanual handpieces, to me, is a big advantage because it allows me to reach every part of the capsular bag (Figure 3). I can use the irrigation handpiece to lift the iris to allow access underneath. Even with a small pupil like this one, I can meticulously clean all of the cortex out of the eye.
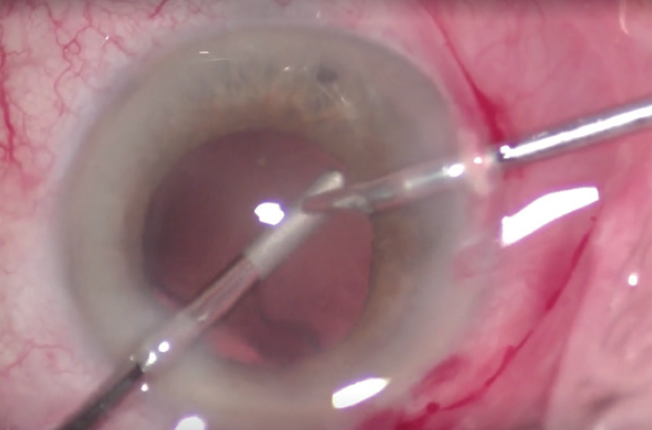
Figure 3. Separation of irrigation and aspiration can aid the surgeon in being able to reach every part of the capsular bag.
LENS INSERTION
With cortical removal complete, I fill the capsular bag with OVD, again normally Amvisc, to prepare for IOL insertion. I frequently use an extended depth of focus IOL as my routine lens. The Acunex Vario (Teleon Surgical; not available in the United States) is a hydrophobic IOL that features a 1.50 D add in an asymmetric near segment.
The lens folds and goes into the shooter smoothly and easily, and, after ejection from the shooter, it unfolds nicely in the capsule in a controlled manner.
The hydrophobic material is glistening-free, according to the manufacturer. The quality of vision is excellent, and patient satisfaction has also been excellent. I have been describing the lens to patients as a normal, routine lens with a small degree of multifocality (extended depth of focus) so that at least they can see well at an intermediate distance and, in combination with monovision, also at near. Patients hardly ever report any kind of optical phenomena.
FINISHING UP
After implantation I aspirate the OVD, again using the I/A handpieces. I aspirate thoroughly from behind the lens by putting the irrigation handpiece under the lens to wash out the OVD. The final steps are the closing of the paracenteses and the incision with wound hydration, followed by injection of cefuroxime.