I am grateful and humbled to be part of arguably one of the greatest eye care centers in the country. Our surgical practice includes five anterior segment surgeons, two retina surgeons, and one oculoplastics surgeon. In 2018, we performed more than 14,000 surgeries, and, of those, 7,319 were cataract procedures.
As a former Army officer, I cannot emphasize enough the role of teamwork in an organization. The staff at Center for Sight is the epitome of teamwork, and we work together like a well-oiled machine. This makes my surgery days feel less like work and more like fun.
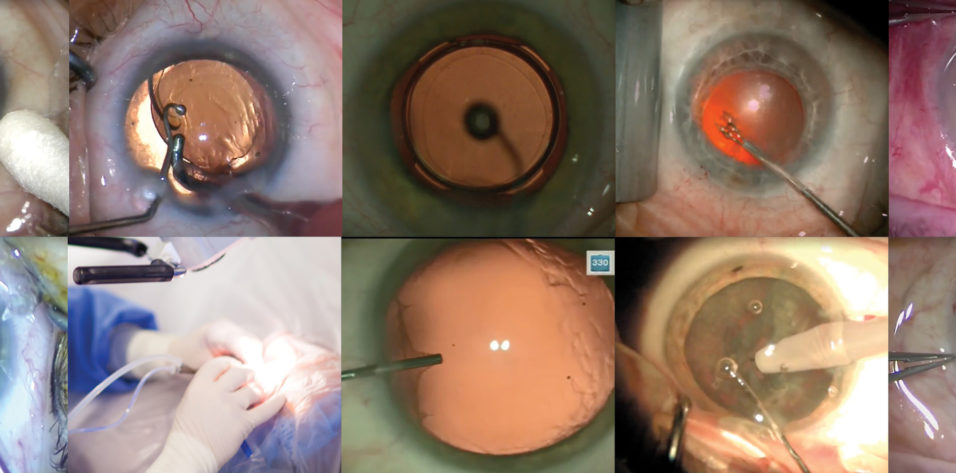
We were early adopters of the femtosecond laser, and I have performed more than 30,000 cases with the Lensar Laser System (Lensar). I have a unique role in my practice in that I run the Lensar three mornings per week, from 7 to 9 am, and see patients in the clinic for the remainder of the day. On the fourth day, I run the Lensar in the morning and also perform Nd:YAG capsulotomies. In the afternoon, I perform all of my own cases (Figure 1).

Figure 1. Dr. Soscia performs cataract surgery.
ALL-DAY SURGERY DAYS
My typical all-day surgery day includes approximately 30 femtosecond laser procedures and 15 Nd:YAG capsulotomies in the morning. In the afternoon I typically perform 25 more cataract surgeries, and 10 to 15 of these are laser cataract surgery procedures. I use the Lensar in conjunction with the Compact Intuitiv System (Johnson & Johnson Vision) for phacoemulsification.
On an all-surgery day, I use two rooms in our ambulatory surgery center and one separate room where I perform the femtosecond laser portion of the case. I typically schedule my femtosecond cases first, which enhances our efficiency because it enables me to perform most of the laser procedures before entering the OR.
BREAKDOWN OF A TYPICAL CASE
For a typical case with the femtosecond laser, I program a 5.25-mm capsulorhexis. This size, which is optimal for my technique, also ensures an appropriate 360º overlap of the anterior capsule on the anterior surface of the IOL. If I am implanting a toric IOL, I rely on the Intelliflap feature of the Lensar system to mark the axis of astigmatism directly on the capsulotomy. I also use the laser to make a small intrastromal corneal mark that serves two purposes. First, it can be used in conjunction with the Intelliflap mark to help align a toric IOL. Second, the mark can be used to center limbal relaxing incisions (LRIs) in situations in which we choose to use a manual LRI instead of the laser system’s astigmatic keratotomy function.
In the OR, if I am making a manual paracentesis and corneal wound, I use a Fine-Thornton Fixation Ring (Katena) to stabilize the eye. If I am performing LRIs, I do so at the beginning of the case with the Mastel President (Mastel), set at 550 µm, after injecting a small amount of lidocaine with epinephrine. If the corneal wound is done manually, I use the Mastel 2.8-mm diamond keratome. My typical approach is a temporal clear corneal incision.
I then proceed to fill the eye with my OVD of choice, Amvisc Plus (Bausch + Lomb), which has an excellent balance of cohesive and dispersive properties. I then either verify that the capsulotomy is free-floating or, if I perform the capsulorhexis manually, use the Mackool-Inamura Capsulorhexis Forceps (Duckworth & Kent) to complete the capsulorhexis. Hydrodissection and hydrodelineation are then performed with balanced saline solution using a 27-gauge Chang Hydrodissection Cannula (Katena).
If I am facing a very dense cataract, a shallow anterior chamber, or an eye with a low endothelial cell count, I place a small amount of Healon EndoCoat (Johnson & Johnson Vision) in the anterior chamber for added corneal protection during phacoemulsification. EndoCoat is an excellent dispersive OVD that coats the endothelium throughout the duration of the case. My phaco tip of choice is a 20-gauge bent tip with a 30º bevel. With my phaco settings, this type of tip provides the best phacodynamics.
When the Lensar is used to fragment the lens, the laser’s software performs an automatic analysis of the density of the cataract so that the surgeon can match each density with a predetermined chop, dice, or combination fragmentation pattern. Each of our five surgeons has unique fragmentation patterns set to each cataract density, based on factors such as primary phacoemulsification technique. Our surgeons choose their techniques based on the hardness of the cataract, the endothelial cell count, and the second instrument of choice.
I prefer a supracapsular technique for soft cataracts with deep anterior chambers. In harder cataracts, I prefer a stop-and-chop or vertical chopping technique. My second instrument is the dual-ended Nagahara Fine Chopper and Nichamin Quick Chopper (MicroSurgical Technology). One end is perfect for a horizontal chop, and the quick-chop end is perfect for dense cataracts with a vertical chopping technique. In laser cataract surgery, I choose the fragmentation pattern that is symbiotic with my particular technique and the characteristics of the cataract.
After phacoemulsification is complete, I perform irrigation and aspiration with a curved tip, making subincisional cortex easy to aspirate. The capsular bag is then filled with OVD and the IOL inserted.
IOL SELECTION
For premium lens patients, we always customize the IOL based on patient needs. Perhaps our most popular option is to combine the Tecnis Symfony IOL (Johnson & Johnson Vision) with the Tecnis Multifocal (Johnson & Johnson Vision). We have found that this combination provides patients with the greatest level of spectacle independence and satisfaction.
For monofocal lens patients, we match the implant with the patient’s corneal Q value, determined using the Pentacam (Oculus), in order to obtain the highest quality of vision.
For all patients, we work hard preoperatively to obtain an optimal ocular surface. Many surgeons overlook this important step.
CONCLUSION
We have had the Lensar laser for more than 7 years, and we now have one of the largest databases of Lensar cases. Having the ability to perform iris registration with the laser is an invaluable tool for perfecting our astigmatic results. Perhaps more important, buried beneath the precise refractive results we achieve with this laser in our premium patients, is the benefit the laser affords in difficult cases.
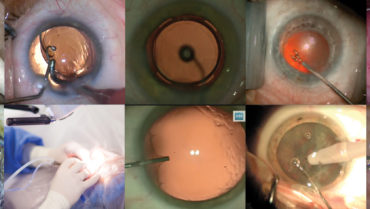
We perform free cataract surgery for indigent patients every summer in our annual Mission Cataract program, a 2-week event that is aided by the Center For Sight Foundation (Figure 2). Lensar has donated free certificates for all of these indigent patients. Through this program, we have documented the results of a series of almost 400 patients with extremely dense and difficult cataracts. We plan to present this data at the Kiawah Eye Meeting this year.

Figure 2. Dr. Soscia performing laser cataract surgery for an indigent patient as part of the practice’s Mission Cataract program.