CASE PRESENTATION
A 21-year-old woman presents for a laser vision correction evaluation. The patient states that she sees well with her soft contact lenses but does not like wearing glasses because of their heaviness and peripheral distortion. She reports no contact lens intolerance, eye rubbing, or dry eye.
By report, her refraction has been stable for the past 3 years. The manifest refraction is plano -5.75 x 180º OU. BCVA is 20/15 OD and 20/30 OS. The patient reports that the poor BCVA in her left eye is due to long-standing amblyopia from an untreated “lazy eye.”
On both autokeratometry and topography, the steepest keratometry reading is just above 50.00 D in each eye. IOP is normal. The optic nerves are symmetrically cupped (0.4 OU), and the rims appear to be healthy. The patient reports no family history of glaucoma or corneal ectasia. The rest of the examination is unremarkable (Figures 1–3).
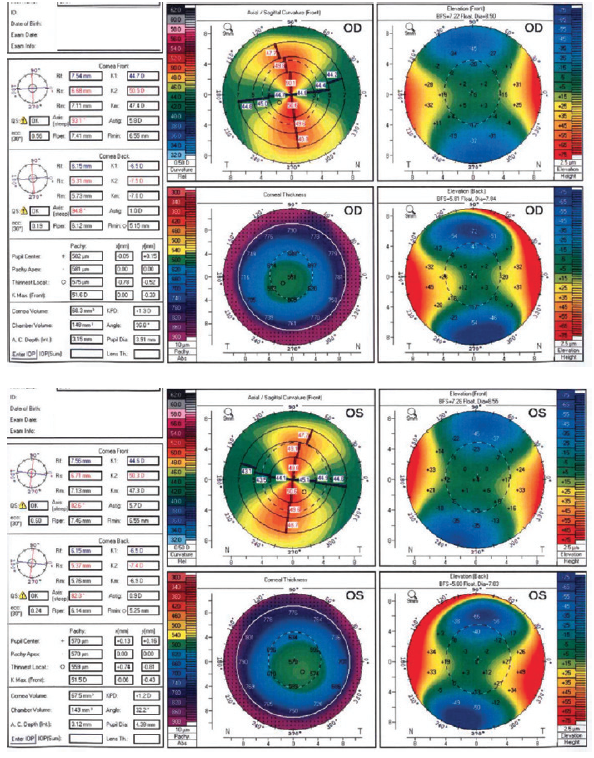
Figure 1. Analysis with the Orbscan IIz (Bausch + Lomb).
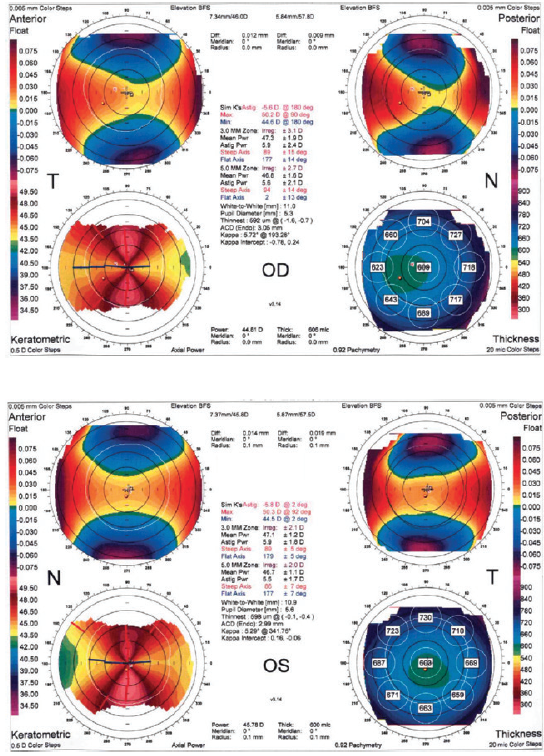
Figure 2. Findings with the Pentacam.
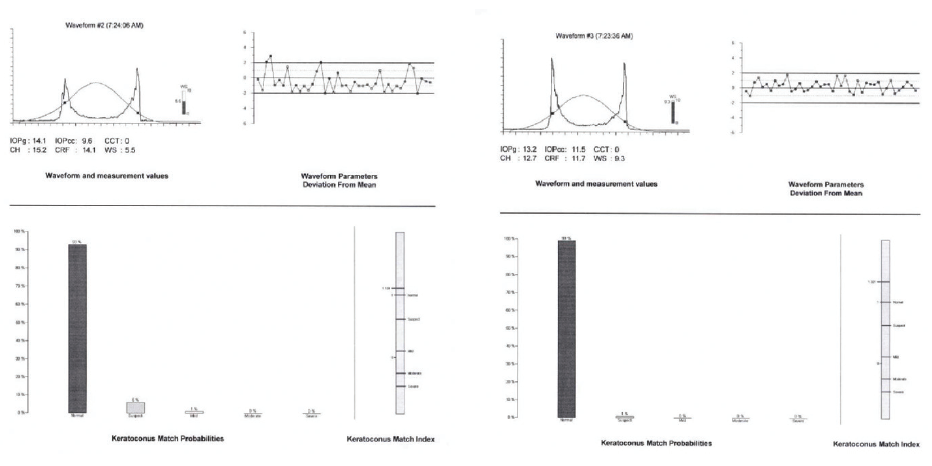
Figure 3. Keratoconus Match Index on the Ocular Response Analyzer (Reichert).
—Case prepared by Christopher E. Starr, MD

MARGUERITE B. MCDONALD, MD, FACS
If refractive stability is clearly established, there are several factors in this case that contraindicate laser vision correction of any kind. First, the patient is young and has steep keratometry readings, and she could develop keratoconus. Second, she has amblyopia in the left eye. Third, the FDA-approved excimer laser systems do not correct her amount of astigmatism. Using two key cards in an off-label fashion would run the risk of inducing higher-order aberrations from a high cylinder correction. Moreover, this level of correction increases the possibility that an enhancement will be required.
I also would not perform intraocular surgery—either a refractive lens exchange or placement of a phakic IOL—in a 21-year-old who can tolerate contact lenses. Instead, I would recommend that this patient remain in her contact lenses for now.


RAPHAEL PENATTI, MD; AND GEORGE O. WARING IV, MD, FACS
This patient has high, bilateral, radially symmetric, with-the-rule astigmatism. The anterior and posterior elevation maps are within normal limits and consistent with high regular astigmatism.
First, we would look carefully for risk factors for developing keratoconus such as atopy or a history of excessive eye rubbing. We would attempt to obtain historic manifest refractions and topographies to look objectively for progression of astigmatism. We would evaluate advanced corneal tomography analysis such as the Belin/Ambrósio Enhanced Ectasia Display, and we would pay particular attention to the maximum Ambrósio relational thickness index (Pentacam, Oculus Optikgeräte). Additionally, we would assess the corneal biomechanics with a noncontact tonometer such as the Corvis ST (Oculus Optikgeräte). The Corvis Biomechanical Index and Tomographic Biomechanical Index have been shown to be accurate indices for evaluating the risk of corneal ectasia.1 Further, we would evaluate a model of ocular mechanical behavior that uses the finite element method (SpecifEye, OptoQuest) with pre- and postoperative strain comparison maps as well as the ectasia match percentage.
If all of these indices appeared to be favorable, we would perform LASIK on both eyes.
Before treatment, we would counsel the patient on her increased risk of ectasia and possible need for CXL in the future. Because of her history of amblyopia, we would review and document her BCVA and UCVA and take the guarded prognosis for her left eye into consideration. We would inform the patient that treatment might be staged in order to treat the full amount of refractive astigmatism, and we would emphasize that an enhancement cannot be performed if ectasia is suspected.

WHAT I DID: CHRISTOPHER E. STARR, MD
Their opposing treatment recommendations notwithstanding, I largely agree with both of the viewpoints presented by the panelists. Despite the patient’s remarkably high but regular astigmatism, the steep keratometry reading (> 50.00 D), and her youth, there were no other significant red flags for corneal ectasia. Readings with the Belin/Ambrósio Enhanced Ectasia Display were normal, and results with the Keratoconus Match Index on the Ocular Response Analyzer confirmed normal corneal biomechanics.
The patient was highly motivated to undergo surgery to reduce her astigmatism, even if not completely. After a thorough discussion of all of the options and their inherent risks, she opted to undergo bilateral conventional PRK with adjunctive mitomycin C because of her increased risk of haze and with the understanding that there would be approximately 2.00 D of residual astigmatism. We agreed that her corneal stability would be closely monitored for at least 1 year after surgery before considering a second PRK procedure or corneal relaxing incisions to treat the residual astigmatism. Then the COVID-19 pandemic struck New York City, where I practice, and all elective surgery was halted. We hope to schedule surgery in the near future.
1. Ambrósio R Jr, Lopes BT, Faria-Correia F, et al. Integration of Scheimpflug-based corneal tomography and biomechanical assessments for enhancing ectasia detection. J Refract Surg. 2017;33(7):434-443.




