The best way to get started with toric IOLs is to set yourself up for early success. As with all aspects of refractive cataract surgery, there are many nuances with toric lenses that can be overwhelming initially. By becoming comfortable with the basics of these IOLs, you can gain the confidence needed to tackle increasingly challenging cases. Every toric lens case requires the same basic steps: patient selection, lens selection, marking of the axis, and lens implantation and orientation. Using the guidelines presented in this article is a great way to get started and hopefully help ensure early success for you and your patients.
PATIENT SELECTION
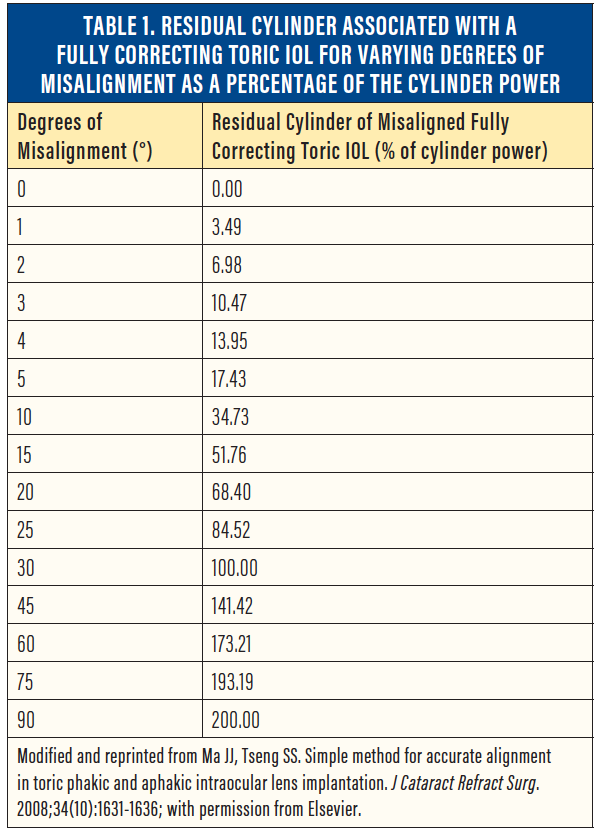
Initially, you should select patients with lower amounts of astigmatism. Think: “Aim small, miss small.” Roughly 3% of astigmatic correction is lost for every 1° of toric misalignment (Table 1).1 Take, for example, a patient with 4.50 D of cylinder. If the alignment of a fully correcting toric IOL for this patient is off by 10°, the IOL would lose 33% of its effect, leaving the patient with 1.50 D of visually significant astigmatism. If a fully correcting toric IOL is off by the same 10° in a patient with a total of only 1.25 D of astigmatism, the IOL would still lose 33% of its effect; however, it would leave this patient with only 0.41 D of residual astigmatism.
When you begin to incorporate toric IOLs into your practice, it is best to start in patients with regular astigmatism and normal baseline topography. Toric IOLs should be thought of as premium lenses, and they are best suited for premium eyes—those that are healthy from the cornea to the fovea.
Irregular astigmatism due to factors such as ocular surface disease, corneal scars, pterygia, and Salzmann nodules, to name a few, will compromise the efficacy of the toric IOL. In such patients, the corneal irregularity can often be improved medically or surgically. Then, after testing is repeated and the patient’s visual status is shown to be stable, the patient may be considered a reasonable candidate for toric IOLs.
LENS SELECTION
In general, you should choose the toric IOL power with the aim of minimizing residual astigmatism. Do not be afraid to flip the axis to with-the-rule (WTR) cylinder in the process (Figure). Traditionally, it was thought that one should never flip a patient’s astigmatic axis, regardless of the orientation. However, leaving a patient with a small amount of WTR astigmatism not only gives the patient a slightly increased depth of focus,2 but it also helps to neutralize the natural against-the-rule (ATR) cylinder drift that occurs with age.3,4 Consequently, many providers treat lower levels of ATR astigmatism and flip the patient’s axis to WTR as a result.
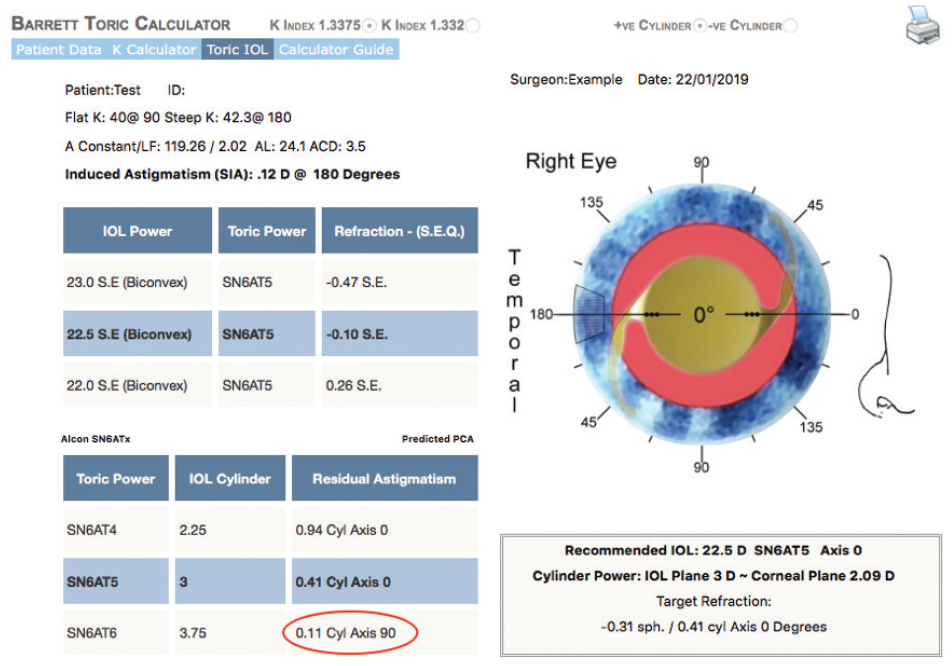
Figure. Measurement from ascrs.org/barrett-toric-calculator: The default lens selection is for a T5 toric, which would leave the patient with 0.41 D of ATR astigmatism at 0°. We would recommend instead using a T6 toric, which would minimize the residual astigmatism to 0.11 D and flip the axis to WTR.
To calculate your toric IOL model, power, and axis, we recommend using the Barrett Toric Calculator. There are many options available for toric IOL calculation; however, numerous studies have shown superior astigmatic outcomes with this calculator.5,6 Further, the Barrett Toric Calculator can easily be used with any standard IOL, it can be accessed for free from the ASCRS website, and it can be added on as software on certain optical biometry devices to allow automatic, integrated toric IOL calculation.
To get started with toric IOLs, we recommend using monofocal torics. This is advisable because toric multifocal (TMF) IOLs are more sensitive to residual astigmatism than are monofocal lenses, and patients experience a greater loss of visual acuity for a given amount of toric misalignment with a TMF.7 The surgeon can be put in a difficult position when a patient is unhappy with his or her vision with residual astigmatism after TMF implantation. It is challenging in this situation to determine whether such a patient is best suited for further astigmatism correction or for IOL exchange with a monofocal IOL. Therefore, because it is arguably more crucial that astigmatism be fully corrected in a TMF patient, it is recommended to start with monofocal toric IOLs until you become comfortable with the basics of torics.
Toric IOL Myths Busted
Getting started with toric IOLs can be daunting, but separating fact from fiction can encourage a closer look.
By John P. Berdahl, MD

Roughly speaking, about one-third of all patients will benefit from astigmatic correction, making toric IOLs a valuable tool for the cataract surgeon. These lenses have been available in the United States since the late 1990s, yet many surgeons are still reluctant to use them today. Let’s look at the three top myths that prevent adoption.
Myth No. 1: Toric IOLs require a lot of extra equipment. Perhaps the most common myth associated with the incorporation of toric IOLs into a cataract surgery practice is that one must have access to every piece of technology available to do a good job.
Fact: Although some supplementary technologies can aid in the precision of toric IOL implantation, they are not all mandatory. The only two mandatory pieces of equipment are a topographer and an optical biometer. Each and every patient who is scheduled for toric IOL implantation should undergo topographic evaluation to identify any corneal irregularities, to confirm that the astigmatism is regular, and to verify the axis and magnitude of corneal astigmatism determined by the optical biometer.
Myth No. 2: Patients in my region aren’t willing to pay extra for cataract surgery. It is no myth that toric IOLs are associated with an out-of-pocket cost to patients, but you won’t know if patients are willing to pay unless you ask them.
Fact: We have an obligation to provide patients with all of the available options, including toric and presbyopia-correcting IOLs. Before they come in the door, one-third of patients know that they don’t want and are not interested in anything extra, one-third know that they are interested in gaining more from their vision, and one-third don’t even know their options. In our practice, about 35% to 40% of patients want to be less dependent on glasses after cataract surgery. Sometimes that requires a toric lens, sometimes a presbyopic lens.
Talking with patients about cost can be uncomfortable, but, with practice, the conversation gets easier and the surgeon gets more comfortable navigating the dialogue. The bottom line is that you shouldn’t sell patients on the service—you should help them understand their options.
Myth No. 3: Residual astigmatism will lead to unhappy patients. Untreated residual astigmatism will lead to unhappy patients, but, most of the time, fixes for residual astigmatism are readily available.
Fact: It is true that some patients are still going to have astigmatism after a toric lens is implanted, but with proper preoperative counseling, adequate planning, and readily available solutions, they don’t have to be unhappy. Fixes for residual astigmatism include prescription glasses, IOL rotation, IOL exchange, and excimer laser enhancement. No matter how good a surgeon you are, some patients will indeed end up with residual astigmatism.
One key to early success is that, when you are just learning to use toric IOLs, you should select patients who have a meaningful amount of regular astigmatism and an easygoing personality. The ideal amount of astigmatism in early cases is between 1.50 and 3.00 D because with that degree of cylinder you can reliably determine the axes.
CONCLUSION
Adding toric IOL implantation to your practice can be daunting, but today it is a wonderful option for correcting astigmatism. These lenses can help to boost postoperative uncorrected visual outcomes and patient happiness. With minimal equipment and the right strategy for educating patients and talking about out-of-pocket costs, any surgeon can enjoy success with toric IOLs.
AXIS MARKING
There are many methods of marking the axis on the eye.8 The cheapest and easiest way is the manual reference marker method. With this method, a fine-tip surgical marker is used to mark the 3 and 9 clock positions on the limbus while the patient is sitting and looking straight ahead. This takes into account the variable degree of cyclotorsion that occurs when patients assume the supine position for surgery.
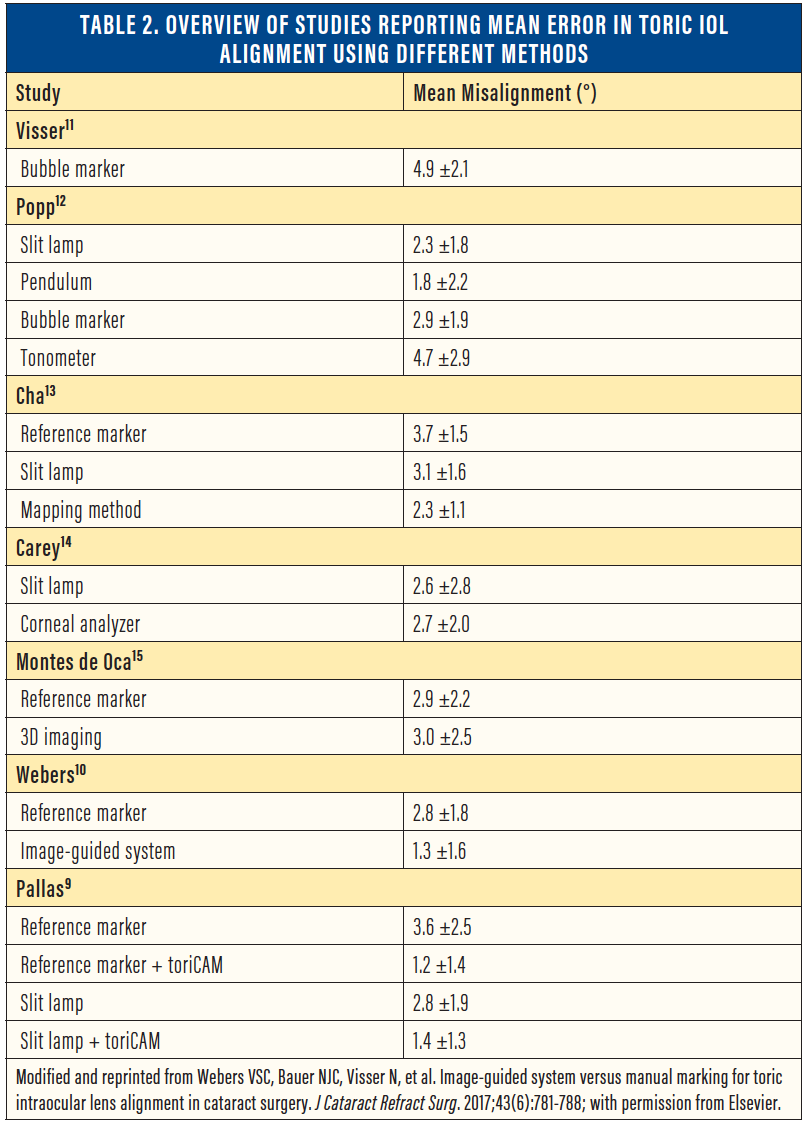
Once the patient is positioned for surgery, the surgeon can use a corneal meridian marker to mark the desired target axis. Many modifications of this technique exist, including marking at the slit lamp or using toric markers with built-in bubbles, pendulum markers, or smartphone applications such as toriCAM, developed by Graham D. Barrett, MD.9 Another approach is to use preoperative imaging with intraoperative iris and limbal landmark registration to provide an image overlay of the toric axis in the surgeon’s microscope.
Although image-guided10 and smartphone marking techniques9 have been shown to lead to slightly lower degrees of misalignment (Table 2), this has not correlated with better visual acuity results or lower residual astigmatism.10 Consequently, we recommend experimenting with different marking techniques until you find what works best for you and your practice.9-15
LENS IMPLANTATION AND ORIENTATION
Initial implantation of a toric IOL should be done in the same fashion the surgeon is accustomed to with a nontoric IOL. However, as the haptics are unfolding, we recommend positioning the IOL axis marks 5° to 10° counterclockwise from the final desired axis. This will compensate for lens shift during removal of OVD, during which the lens often rotates by several degrees independently. Once all of the OVD has been removed, the IOL can then be rotated clockwise into the final position using a blunt second instrument through the paracentesis incision.
Given the standard haptic configuration and angle of most IOLs, it is never recommended to rotate more than a few degrees counterclockwise, as this can put unwanted stress on the capsular bag and increase the risk of a capsular tear. We also recommend aspirating the OVD from behind the toric IOL in order to minimize the risk of rotation postoperatively, which can occur due to residual OVD between the IOL and capsular bag. Finally, caution should be used in high axial myopes, in whom the risk of toric IOL rotation after implantation is greater.
PATIENT COUNSELING
As is the case with any premium surgery, patient counseling is paramount. The expectation for both the patient and surgeon should be to maximally reduce, but not necessarily eliminate, the patient’s astigmatism. Given the limited range of toric lens powers, imperfect keratometry measurements, and variability of the posterior cornea, even with the best surgical technique it is impossible to completely eliminate every patient’s astigmatism. Always inform patients preoperatively that, occasionally, a patient will require a second procedure to optimize the correction of astigmatism; this advance discussion can be extremely helpful when addressing an error during the postoperative period.
For patients with an unexpectedly large amount of residual astigmatism after toric IOL implantation, the website astigmatismfix.com can be of tremendous help in determining the best course of action, be it rotating the IOL, exchanging the IOL, or performing laser vision correction.
CONCLUSION
The best way to get started with toric lenses is by implanting monofocal toric IOLs in patients with low amounts of regular astigmatism, using the Barrett Toric Calculator, performing reliable axis marking, and engaging in adequate and proper patient counseling.
1. Ma JJ, Tseng SS. Simple method for accurate alignment in toric phakic and aphakic intraocular lens implantation. J Cataract Refract Surg. 2008;34(10):1631-1636.
2. Leube A, Ohlendorf A, Wahl S. The influence of induced astigmatism on the depth of focus. Optom Vis Sci. 2016;93(10):1228-1234.
3. Ueno Y, Hiraoka T, Beheregaray S, Miyazaki M, Ito M, Oshika T. Age-related changes in anterior, posterior, and total corneal astigmatism. J Refract Surg. 2014;30(3):192-197.
4. Ho JD, Liou SW, Tsai RJ, Tsai CY. Effects of aging on anterior and posterior corneal astigmatism. Cornea. 2010;29(6):632-637.
5. Abulafia A, Barrett GD, Kleinmann G, et al. Prediction of refractive outcomes with toric intraocular lens implantation. J Cataract Refract Surg. 2015;41(5):936-944.
6. Kern C, Kortüm K, Müller M, Kampik A, Priglinger S, Mayer WJ. Comparison of two toric IOL calculation methods. J Ophthalmol. 2018;2018:2840246.
7. Garzón N, Poyales F, de Zárate BO, Ruiz-García JL, Quiroga JA. Evaluation of rotation and visual outcomes after implantation of monofocal and multifocal toric intraocular lenses. J Refract Surg. 2015;31(2):90-97.
8. Kaur M, Shaikh F, Falera R, Titiyal JS. Optimizing outcomes with toric intraocular lenses. Indian J Ophthalmol. 2017;65:1301-1313.
9. Pallas A, Yeo TK, Trevenen M, Barrett G. Evaluation of the accuracy of two marking methods and the novel toriCAM application for toric intraocular lens alignment. J Refract Surg. 2018;34(3):150-155.
10. Webers VSC, Bauer NJC, Visser N, Berendschot TTJM, van den Biggelaar FJHM, Nuijts RMMA. Image-guided system versus manual marking for toric intraocular lens alignment in cataract surgery. J Cataract Refract Surg. 2017;43(6):781-788.
11. Visser N, Berendschot TTJM, Bauer NJC, Jurich J, Kersting O, Nuijts RMMA. Accuracy of toric intraocular lens implantation in cataract and refractive surgery. J Cataract Refract Surg. 2011;37:1394-1402.
12. Popp N, Hirnschall N, Maedel S, Findl O. Evaluation of 4 corneal astigmatic marking methods. J Cataract Refract Surg. 2012;38:2094-2099.
13. Cha D, Kang SY, Kim S-H, Song J-S, Kim H-M. New axis-marking method for a toric intraocular lens: mapping method. J Refract Surg. 2011;27:375-379.
14. Carey PJ, Leccisotti A, McGilligan VE, Goodall EA, Moore CBT. Assessment of toric intraocular lens alignment by a refractive power/corneal analyzer system and slitlamp observation. J Cataract Refract Surg. 2010;36:222-229.
15. Montes de Oca I, Kim EJ, Wang L, et al. Accuracy of toric intraocular lens axis alignment using a 3-dimensional computer-guided visualization system. J Cataract Refract Surg. 2016;42:550-555.