
This is an important topic for me and for my career. I’ve been involved in developing, testing, and using multifocal IOLs for more than 20 years in the United States and in Central America. My experience in routine clinical use and in sponsored research has allowed me to carefully evaluate the past and present of multifocal IOLs and to glimpse the future of and alternatives to these lenses. I should admit at the outset of this article that I am biased toward the Johnson & Johnson Vision series of multifocals—in part because I helped to develop and test them and thus know them very well. However, I have helped to develop other IOLs that are excellent options for correcting presbyopia, and I have relevant clinical and research experience with the large variety of multifocal IOLs available in Central America. I will share my experience and observations with as little bias as possible.
THE EYES OF A 19-YEAR-OLD
Many authorities suggest that the teenage years of a person’s life offer the best quality of vision. In books about sailing on the high seas in centuries past, it was usually a teenage boy sitting in the crow’s nest of a privateer ship as the lookout because it was learned by hard experience that a teenage boy likely had the best vision for the task. It is therefore worth reviewing the distance, unaccommodated, and near accommodated wavefronts of the eyes of a high-functioning 19-year-old who subsequently does very well in college and medical school without glasses (Figures 1 and 2). Presumably, this patient’s eyes are a great example of what an optimal set of wavefronts should look like.
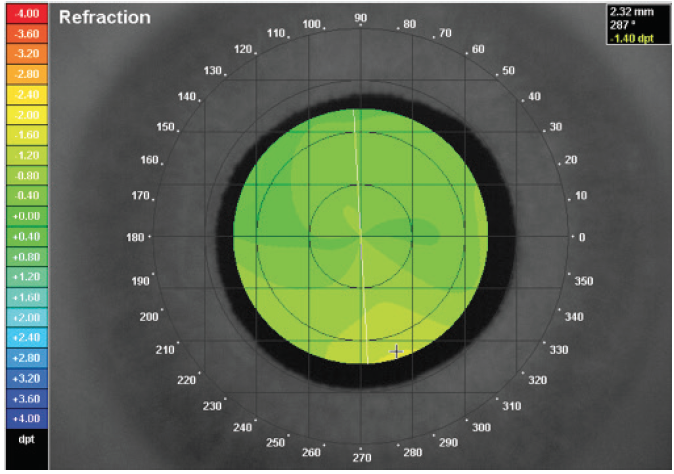
Figure 1. A high-quality, whole-eye wavefront of a 19-year-old with excellent eyesight and excellent studying habits who graduated from medical school a few years later. On the scale on the left-hand side, green represents no deviation of the wavefront. There are minimal higher-order aberrations, and the system forms a high-contrast image of the distance vision on the macula.
Refractive cataract surgeons are familiar with the unaccommodated distance wavefront of a normal adult and typically make decisions relative to this mental construct. The distance wavefront is usually almost uniformly green with minimal higher-order aberrations (HOAs). Figure 1 confirms that the 19-year-old has an excellent quality and quantity of distance vision; this is the kind of image surgeons strive for when they perform laser vision correction.
On the other hand, refractive cataract surgeons rarely evaluate the wavefronts of accommodating eyes, so they are less familiar with the expected findings of a near wavefront. What happens when the same 19-year-old reads his textbooks in preparation for college and medical school courses? When a person with a normal visual system views objects at near, the objects are at different distances. In this situation, multifocality helps him to focus on the images simultaneously. This idea can be illustrated by a dinner date: A person will want to see his or her companion’s face, the food, and the drinking glasses, but those objects will be at different distances. The normal human visual system usually becomes multifocal at near to allow better visualization of these kinds of near objects (Figure 2). I will touch on an important exception to this rule later in this article.
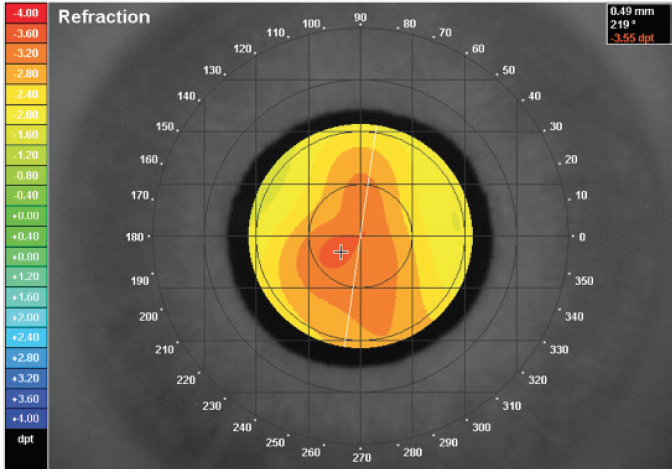
Figure 2. The same eye as pictured in Figure 1. This wavefront is composed of multiple warm colors consistent with varying degrees of myopia induced from the accommodative effort. When viewing a near target with a 5.00 D accommodative demand, the eye develops a multifocal imaging system. The eye must be presumed to see well because the patient does well in college and medical school with no glasses.
MULTIFOCALS MUST STRIKE A BALANCE
Human eyes most often demonstrate flat, green wavefronts at distance in an unaccommodated state, but multifocal wavefronts at near in an accommodated state. This means a multifocal IOL designer must strike a balance to minimize the compromise between various vision goals. (A typical multifocal IOL patient needs as little multifocality at distance as possible and as much multifocality at intermediate and near as possible. This is a tall order for an IOL with a fixed shape.)
While eye care providers eagerly await an accommodating IOL that will effectively change shape like the natural crystalline lens, the AcrySof ReStor series of IOLs (Alcon) attempts this very compromise by minimizing the amount of multifocality at distance to a central diffractive zone of 3.6 mm. Therefore, when the pupil dilates larger than 3.6 mm, the portion of the pupil not in the central diffractive zone is in a monofocal zone. This design is a clever way to minimize multifocality at distance and maximize it at near when the pupil is more likely to be smaller.
INTEGRATING NEW TECHNOLOGY AND LESSONS LEARNED
In ophthalmology, it often takes 30 years or more to fully integrate new technology into the mainstream. For instance, IOLs were first implanted in the early 1950s but were not commonly used until the ‘80s. Phacoemulsification was described in the mid-60s but became commonplace in the mid-90s. Multifocal IOLs were first studied in the ‘80s (3M diffractive IOL, 3M; no longer available) and were first approved by the FDA in the late ‘90s (Array zonal refractive lens, Advanced Medical Optics; no longer available). As with other cycles of ophthalmic innovation, it is no surprise that multifocal IOLs are still used in a minority of cataract surgery cases.
That is not the case, however, if the percentage of refractive lens exchange patients who receive multifocal IOLs is taken into account. If extended depth of focus IOLs are included here, then some form of presbyopia-correcting IOL accounts for the clear majority of refractive lens exchange cases. It can safely be assumed that the reason for the lens surgery and the associated cost of the surgery have a big impact on IOL choice.
This observation raises a crucial point regarding multifocal IOL use, which is always to consider why a patient is having the surgery. If a patient’s primary goal is to remove the blur from his or her vision and not the glasses from his or her nose, then a standard monofocal IOL is a great choice. On the other hand, if the patient does want to remove the glasses from his or her nose, then a multifocal IOL is a great choice. The latter patient is more likely to accept the increased cost and the decreased contrast sensitivity of a multifocal IOL as a trade-off for freedom from glasses (Figure 3).
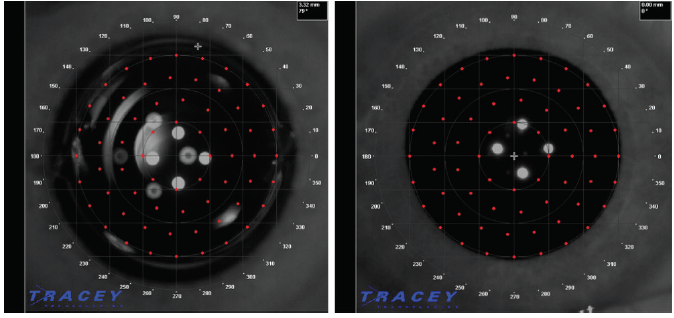
Figure 3. Right eye of a 46-year-old man with a distance UCVA (UDVA) of 20/10- and multiple reflections from a zonal refractive multifocal IOL (pictured left). Right eye of a 13-year-old boy with 20/16 UDVA, no history of eye surgery, and no significant internal reflections from his phakic lens (pictured right). The difference in the images demonstrates that there is more to patients’ subjective experiences than UDVA alone. Trading a normal phakic crystalline lens for an IOL of any kind will add unwanted reflections from the IOL to optical system.
Whatever the motivation for cataract surgery, patients’ primary concern is typically safety. In other words, they want a minimal risk of complications or secondary surgery. Although the final refractive outcome is important, wearing a pair of glasses to achieve that final refractive goal is not a big negative to some patients.
My emphasis on patient motivation derives from my experience with the Array multifocal IOL in the early 2000s. I was implanting the Array in about 40% of patients, and my goal was to minimize their postoperative need for glasses. My patients did not always share that goal, however, and often returned to the office a year or 2 after surgery wearing glasses. Their reasons varied, but they all indicated to me that they had undergone surgery to decrease blur, not to free themselves from glasses. I came to realize that I was not asking the best questions preoperatively.
At that time, we did not charge a premium for multifocal IOLs. Interestingly, this group of patients rarely complained much about postoperative glare and halos, and I virtually never performed an IOL exchange or laser vision correction enhancement to correct residual refractive error.
In contrast, I also implanted the Array IOL in a subset of hyperopic patients who presented for refractive surgery. This group complained more often about glare and halos and regularly required refractive enhancements—either an IOL exchange or laser vision correction. They sent me a loud message regarding the importance of the motivation for IOL surgery.
With the introduction in 2005 of a way to charge a premium for presbyopia-correcting IOLs, surgeons’ interest in providing multifocal IOLs to patients increased. At that time, I began to charge patients an out-of-pocket charge for the extra work involved in the surgery. Thereafter, surgeons began to hear more about unmet patient needs, including residual refractive errors, enhancement procedures, and concerns about quality of vision such as loss of contrast sensitivity, glare, and halos.
LESSONS LEARNED
With today’s options for high-quality, diffractive multifocal IOLs, surgeons and patients have an abundance of choices from several manufacturers. In my experience, all of them work, but each has one limitation or another. The biggest lesson that I have learned is that, in order to succeed in refractive cataract surgery, surgeons must understand themselves, their IOL preferences, and their patients. Here I have distilled more than 2 decades of working with multifocal IOLs into four criteria for meeting patients’ needs in every single case.
Lesson No. 1: Not all patients are good candidates for multifocal IOLs. One of the most important questions to ask prospective IOL patients is: “Do you take off your glasses to read?” If they do, they are telling you that they strongly prefer to see at near the flat, green, high-quality wavefront a young eye usually sees at distance. This patient is a poor candidate for a multifocal IOL and will likely be better served by some degree of postoperative myopia.
Lesson No. 2: Surgeons should precisely understand their own outcomes. This requires regularly and reliably tracking outcomes. Otherwise, accurately predicting results is impossible. This past year, I delivered lectures on the topic of improving results with presbyopia-correcting IOLs at two industry-sponsored dinner meetings. Of the approximately 40 surgeons at each dinner, not a single one admitted to tracking his or her results.
Lesson No. 3: Surgeons should know their patients. Ophthalmologists should talk to all patients preoperatively in order to understand their desires and fears. This process includes developing a realistic plan to accomplish a patient’s specific goals and, sometimes, telling a patient “no” when what he or she wants is not yet possible. I told some of my happiest patients “no” the first time I met them. After reevaluation a year or 2 later, I was able to provide them with the results and outcomes they desired. Sometimes, the best recommendation is to await further innovation.
Lesson No. 4: Surgeons should know all their preferred and nonpreferred IOLs. Sometimes an ophthalmologist’s preferred IOL is not the best choice for a particular patient. Surgeons must know the alternative multifocal IOLs and be able to knowledgably choose among them when advisable.
CONCLUSION
More widespread adoption of multifocal and presbyopia-correcting IOLs is imminent. This is fantastic news because it means that more patients will be given the opportunity to achieve their visual goals after cataract surgery.
It is important for surgeons to keep in mind, however, that not all patients have cataract surgery to achieve the same goals. Not every patient desires spectacle independence, and not every patient is a suitable candidate for a multifocal IOL. Nor is one multifocal IOL the optimal choice for every patient receiving this form of presbyopic correction. Successful refractive cataract surgery requires ophthalmologists to know themselves; to understand their patients; and to know all IOL options, including those they prefer and alternative choices. Armed with this knowledge, success with refractive cataract surgery is achievable.




