


Corneal mapping is an important part of the initial consultation for patients who are interested in laser vision correction. There are three main technologies that are part of the corneal mapping process: Placido-disc topography, tomography, and epithelial mapping with OCT or the »ArcScan Insight 100. Most clinicians in the United States have either topography or tomography, but a growing number of centers have added technologies that can perform epithelial mapping, a relatively new technology that can help clinicians understand more about a patient’s corneal status than was previously possible.
AT A GLANCE
- A question that often arises is whether patients who have been diagnosed with keratoconus and have had CXL can become candidates for refractive surgery in the future. Patients with high levels of refractive error may be candidates for a phakic IOL. Patients with mild to early moderate keratoconus who have mild to moderate refractive errors may be able to have PRK in the future.
- Although PRK can potentially be considered in some patients in the first year after CXL, waiting can allow the corneal shape to improve further and potentially provide improved outcomes.
The results of these diagnostic tests help clinicians to determine whether patients are suitable candidates for both PRK and LASIK, for PRK alone, or for neither. The patient’s refractive error and corneal thickness are also key measurements that are used to determine candidacy for corneal refractive surgery.
EXPLORING OPTIONS
A small percentage of patients who are evaluated for refractive surgery will be diagnosed with keratoconus and be informed that they are not candidates for PRK or LASIK as a primary procedure. Instead, they will be directed toward CXL, which strengthens the cornea and prevents keratoconus from progressing. CXL often also improves corneal shape and vision.
One question that often arises is whether patients who have been diagnosed with keratoconus and have undergone CXL can then become candidates for refractive surgery in the future. There are several options. Patients with high levels of refractive error may be candidates for a phakic IOL such as the »Visian ICL (STAAR Surgical). Patients with mild to moderate keratoconus who have low to moderate refractive errors may be able to have PRK in the future.
CASE STUDY
A 21-year-old patient presented in 2012 for CXL (Figure 1). She had moderate myopia in both eyes with BCVA of 20/50 OD and 20/40 OS. She underwent epithelium-on CXL in January 2012 as part of the CXLUSA study. Following the procedure, she experienced significant improvement in corneal shape and vision. She returned in the summer of 2016, at the age of 26, and expressed a strong interest in reducing her need for contact lenses and glasses. On examination, her BCVA had improved to 20/25 OU, and she had experienced significant improvement in corneal shape in both of her eyes (Figure 2).
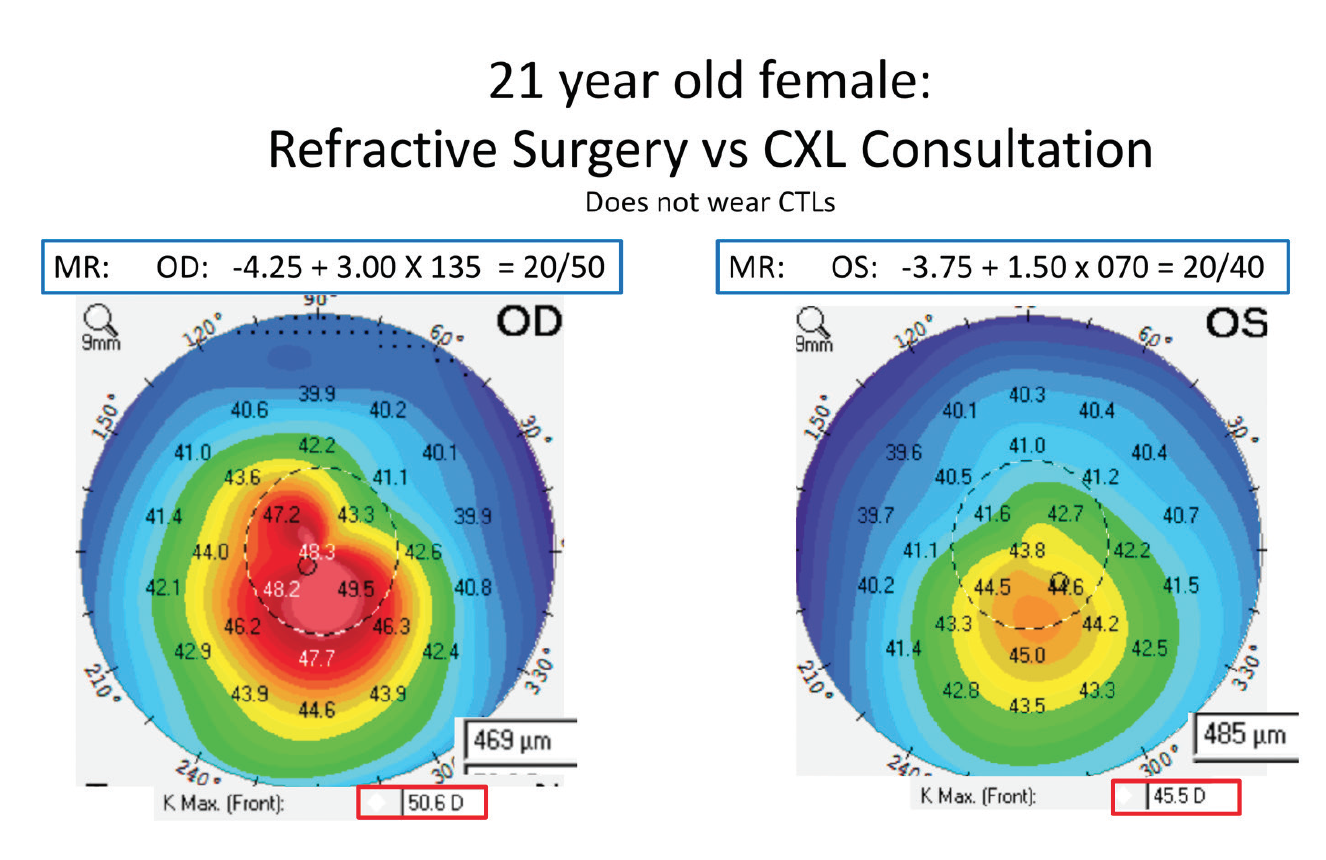
Figure 1. A patient with a history of CXL sought refractive surgery to improve her vision.
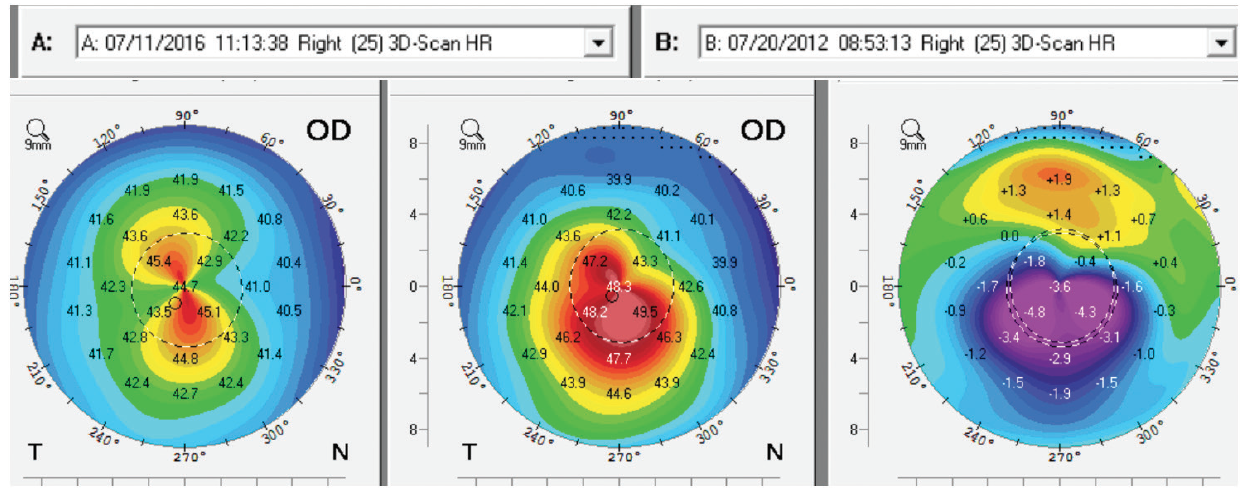
Figure 2. Improvement in corneal shape in the patient’s right eye following CXL.
We spent a lot of time discussing her options. If she lived outside the United States, she might have been a candidate for the »EVO Visian ICL Toric (STAAR Surgical), and we discussed this option in great detail. She was, however, most interested in corneal refractive surgery. She was informed that she would need to continue to return for follow-up visits on an annual basis, and that if she developed signs of a recurrence of keratoconus, she would have to have a repeat CXL procedure.
The patient underwent PRK in both eyes in November 2016 with the »Visx Star S4 IR excimer laser system (Johnson & Johnson Vision). To prepare the cornea, we used the EBK epithelial debridement device (Orca Surgical) and applied mitomycin C 0.02%.
The patient’s right eye was treated with a conventional ablation at a depth of 38 µm; her left eye received a Visx CustomVue wavefront-guided ablation treatment at a depth of 69 µm.
The patient returned 1 year later and reported that she was pleased with her visual outcome. Although she has some mild residual refractive error, she is overall happy with her reduced need for glasses.
CONCLUSION
In general, patients with keratoconus can benefit from undergoing CXL and can experience improvement in their corneal shape and vision. Some patients can then become candidates for refractive surgery. As in this case, patients can experience improvement of their corneal shape over years. So although PRK can potentially be considered in some patients in the first year after CXL, being forbearing can allow the corneal shape to improve further and potentially provide improved outcomes.
Technologies for PRK such as topography-guided Contoura Vision (Alcon) and the wavefront-guided iDesign system (Johnson & Johnson Vision) may provide improved outcomes compared with conventional ablation profiles. Of course, the patient needs to be informed that there is always a risk of recurrence of keratoconus, so continued follow-up with corneal mapping is important.




