CASE PRESENTATION
A 34-year-old engineer presents for LASIK. The patient wears glasses because he lives at high altitude and cannot tolerate contact lenses. He loves cycling and skiing and considers his glasses to be a limitation.
His eyeglass prescription is -3.50 -1.50 X 020º OD and -3.75 -1.50 X 150º OS. In the refracting lane, the patient’s manifest refraction is identical to his eyeglass prescription, correcting to 20/20 OU. The results of the slit-lamp examination are completely normal, and the patient’s general and ocular health are excellent. He takes no medications, has no significant family history, and does not smoke. Pachymetry readings are 555 µm OD and 565 µm OS.
The patient has done his research and politely asks specific questions regarding his suitability for LASIK based upon the images that were just taken of his eyes and the technology that you use. Additionally, you performed LASIK on his mother 15 years ago, and he is wondering how things have changed since then.
Like the first installment of this two-part series (bit.ly/coleman0118), this article breaks from the usual format of the Complex Case Management series. Instead of exploring the management of complications, both pieces provide insight into the complexity of the preoperative evaluation and discussion with a patient. This month’s article concentrates on the patient’s questions regarding the image of his left eye (Figure 1). Although the answers pertain specifically to the iDesign Advanced WaveScan Studio System and »Star S4 IR excimer laser (Johnson & Johnson Vision), the principles can be applied to any laser system.
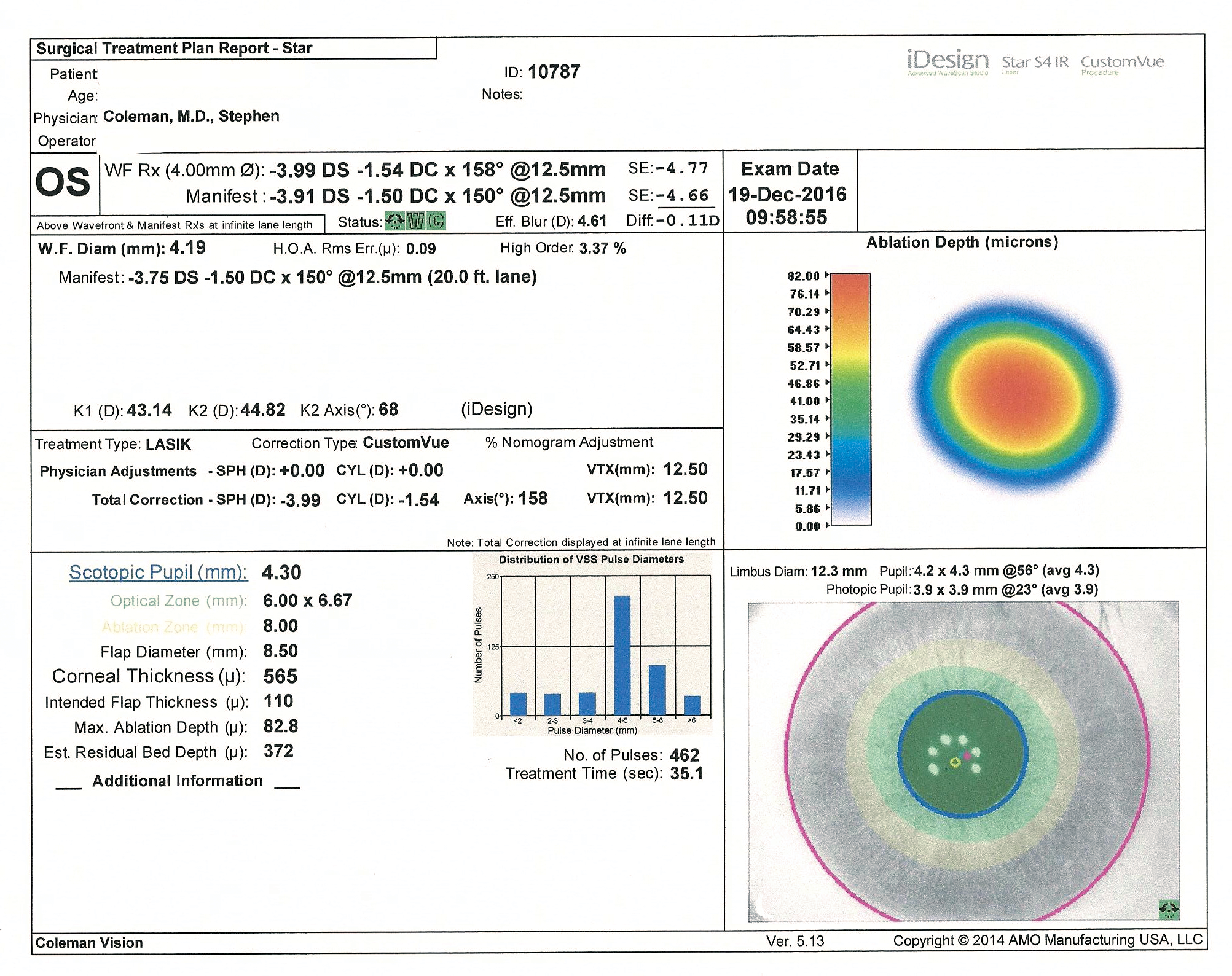
Figure 1. Measurements of the patient’s left eye with the iDesign Advanced WaveScan Studio.
Patient’s First Question
What is a % Nomogram Adjustment, which is noted in the middle box on the left?

Dr. Coleman: Great question. The percentage nomogram adjustment allows a surgeon to make a percentage adjustment to the entire iDesign system–designed ablation. A maximum of 10% is allowed. In other words, it can produce 10% more or less power to the overall prescription being treated, which includes all aspects of that particular prescription. This is a setting that surgeons alter infrequently, once they have established a benchmark based on their environmental conditions, surgical technique, and patient outcomes. This particular adjustment does not affect the overall calculated depth of the ablation, nor does it change the shape of the ablation pattern, which I am sure we will talk about in a minute.
Patient’s Second Question
Are the Physician Adjustments related?
Dr. Coleman: Yes, they allow the surgeon to alter the magnitude of the spherical component of the treatment by ±0.75 D. This is a much more dynamic adjustment and is typically based on the individual patient. For instance, because you are a 34-year-old engineer and we have discussed your visual goals, I might make a slight physician adjustment but leave the percentage nomogram adjustment alone.
Patient’s Third Question
Are you trying to create a specific treatment for me?
Dr. Coleman: That is correct. Laser technology in 2017—not just this particular system but all laser platforms in general—has become more advanced to allow surgeons to make treatments more specific to each individual eye.
Patient’s Fourth Question
What do the green boxes toward the top of the image mean?

Dr. Blanton: These are status bars. The first green square has two rotational arrows, one pointing clockwise and the other counterclockwise. They indicate that this particular map is eligible for iris registration. This tool allows the laser’s software to recognize anatomic landmarks on the iris, which enables it to compensate for any rotation of the eye. People’s eyes rotate when they move from sitting to lying down. After taking such great care to measure the aberrations in a patient’s optical system, it behooves the surgeon to ensure that this precision is translated when the eye rotates.
The second green box has a W in it, indicating that it has passed through a sophisticated algorithm that ensures the consistency and accuracy of the wavefront map.
The third green box has a C in it, indicating that the corneal topographic image is valid. This confirmation is important, because the imaging populates the keratometry values into the treatment. Keratometry values allow the laser treatment pattern to take into account the dome-shaped nature of the cornea.
All of this information helps to create a treatment pattern that is incredibly precise and thus provides better outcomes.
Patient’s Fifth Question
What does Scotopic Pupil (mm) in the lower left column mean?
Dr. Coleman: This is the size of your pupil in dim lighting, not necessarily completely dark but the low-light conditions that occur frequently in real life. Optical scientists and ophthalmologists have taken this information into account and have created laser profiles related to the size of the scotopic pupil, specifically something known as spherical aberration. This complex mathematical term describes what it means when a patient says, “I see a little ghosting or halos around lights at night.” The treatment of spherical aberration is a great step forward, and it is something that glasses and contact lenses do not correct.
We have learned that low-light conditions are quite complex, and we are always investigating ways to improve outcomes in this setting. We cannot adjust the rod-cone ratio in a patient’s eye, for example, but we are able to optimize the shape of the cornea with a laser and address the issue effectively. Does this make sense?
Patient’s Sixth Question
What does the Distribution of VSS Pulse Diameters graph to the right represent?
Dr. Blanton: After the surgeon selects and programs a map for treatment, the laser’s software uses a sophisticated form of calculus that draws on the genius of a well-known French mathematician named Fourier. The Fourier calculation is the best-known way to measure the optical system and then use that information to change the shape of the cornea by gently sculpting the tissue to create the so-called perfect eye.
Each excimer laser pulse removes 0.25 µm of corneal tissue. By comparing your eye to an eye with no aberrations (the perfect eye), the software can calculate how many pulses are needed, what the diameter of those pulses should be, and where they should be placed and overlap to achieve the optimal result. Large pulses efficiently remove tissue, whereas small pulses are necessary to treat subtle irregularities in the optical system that are called higher-order aberrations. This process is known as variable spot scanning, or VSS. The graph showing the distribution of the VSS pulse diameters tells the surgeon how many pulses of each of the various diameters will be used to treat the patient’s eye.
Patient’s Seventh Question
What does the information under the scotopic pupil listing mean?
Dr. Coleman: The optical zone describes the minimum area where your cornea will be treated with laser energy. This is really the specific change in the shape of your cornea that will address and, I hope, eliminate your prescription. I generally use an optical zone of 6.00 X 6.67 mm, but doctors can adjust these dimensions based on the thickness of the patient’s cornea and his or her prescription. In general, the larger the optical zone, the deeper the ablation. The ablation zone is similar to the optical zone and reflects the total diameter of the treatment.
Patient’s Eighth Question
From what I have read, the next few lines are a surgeon’s preference that varies from individual to individual.
Dr. Coleman: Exactly. For you, I would choose a flap diameter of 8.5 mm, which is a little larger than the planned treatment area. I would enter the thickness of your cornea, 565 µm, and I would use an intended flap thickness of 110 µm. In conjunction with a maximum ablation depth of 82.8 µm, the estimated residual bed depth is 372 µm.
Patient’s Ninth Question
What does all of that mean?
Dr. Coleman: What it really means is that, ideally, the diameter of a LASIK flap, for instance, will be larger than the treatment being delivered. There are many opinions regarding the estimated residual bed depth, which ranges from 200 to 350 µm. Most surgeons make this determination based on the patient sitting in front of them. You would be surprised at how much math is involved in surgical decisions and how closely your goal—seeing well—is aligned with your doctor’s goal.