There is more than one “right” way to manage astigmatism. After reviewing each patient’s history, eye metrics, needs, and expectations, I may offer surgical correction or not. With the former, my goal is to eliminate the element of “surprise” when it comes to postoperative outcomes, so I pay close attention to the details during the preoperative stage.
FACTORS FOR CONSIDERATION
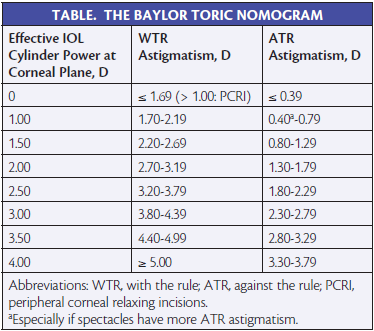
My process of choosing the form of astigmatic correction always keeps the posterior cornea in mind, and I consider both the total corneal astigmatism value from the Cassini (i-Optics) as well as a relaxed version of the Baylor toric nomogram (Table). The basic premise is that about 84% of people have a steep with-the-rule (WTR) posterior corneal curvature, which effectively adds to the total against-the-rule (ATR) corneal astigmatism.1 When I factor in my “wiggle room” for the posterior corneal factor, however, the application of this rule may result in a miscalculation of the toric correction for some patients undergoing surgical treatment. Additionally, this approach does not address eyes with obliquely oriented anterior corneal astigmatism.
The personal nomogram I developed has substantially reduced postoperative surprises in my patients. My method factors in the patient’s age, an important indicator of the drift in anterior corneal astigmatism. For my patients 65 years of age and younger, I aim for a +0.25 D WTR astigmatic target in order to account for the natural anterior corneal drift that occurs over time (on average, 0.34 D from WTR to ATR cylinder).2 In my older patients, my goal is to neutralize the astigmatism fully rather than leave WTR cylinder, because the anterior cornea changes less in this age group in my experience.
Posterior corneal astigmatism is approximately 0.30 to 0.40 D WTR in most patients with anterior WTR astigmatism and approximately 0.20 D WTR in most patients with anterior ATR astigmatism.3 Owing to my concern about flipping the axis in my WTR patients due to posterior corneal astigmatism, I have often undercorrected their astigmatism. I attribute this phenomenon to the following:
1. The actual amount of the posterior corneal astigmatism is unclear, and the patient could also be part of the 16% minority who have ATR or obliquely oriented posterior corneal astigmatism to begin with,1 thus increasing the amount of total WTR astigmatism.
2. The residual WTR astigmatism of approximately 0.20 to 0.30 D I intentionally leave to account for the natural anterior corneal drift.
3. Even minute malrotation of the IOL can further reduce my intended astigmatic correction.
Although not a definitive science, I factor in the contribution of the effective lens position. I will choose a lower toric power for short eyes (< 22 mm) in which the IOL tends to sits more anteriorly, often resulting in a stronger toric correction. In eyes that have a long axial length (> 26 mm), especially if the amount of astigmatism present is between two toric powers, I will choose the higher correction.
A final consideration is that corneas with high amounts of anterior WTR astigmatism also have large amounts of posterior WTR astigmatism. This results in even less total refractive WTR astigmatism. I further reduce the toricity of the IOL by at least 0.50 D in eyes with greater than 3.00 D of anterior corneal WTR astigmatism.
DIAGNOSTICS
The combined result of the subtleties I have described can make selecting the correct toric IOL difficult. I use several diagnostic tools to minimize unexpected surprises. To determine the power of astigmatic correction, I begin with at least two similar anterior corneal keratometry readings obtained by Placido-based topography, total corneal astigmatism value from the Cassini, and optical biometry. I confirm consistency in readings between the Lenstar LS900 (Haag-Streit) and the corneal topography values to account for the posterior corneal astigmatism and decide how to change my astigmatic correction accordingly. Next, I review the cylindrical magnitude and axis in the patient’s spectacles and then factor in the patient’s age and axial length. I also find it important to evaluate and review the postoperative refractive outcome of cataract surgery on the patient’s first eye, because the second eye will likely behave similarly in terms of astigmatic and spherical equivalent results.
CONCLUSION
I look forward to the development of new software and devices specifically engineered to more accurately measure total corneal astigmatism. I believe that future iterations of intraoperative aberrometry, especially when integrated with other devices and preoperative data, will be the best tool for astigmatic correction, because this technology will be able to factor in the refractive magnitude of the astigmatism, the proper axis for alignment, the axial length, and the effective lens position. Until that time, the meticulous analysis of each case can yield excellent outcomes, and my patients have been very happy after the implantation of Tecnis Toric IOLs (Abbott Medical Optics).
1. Koch DD, Ali SF, Weikert MP, et al. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38(12):2080-2087.
2. Hayashi K, Hirata A, Manabe S, Hayashi H. Long-term change in corneal astigmatism after sutureless cataract surgery. Am J Ophthalmol. 2011;151(5):858-865.
3. Koch DD, Ali SF, Weikert MP, et al. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38(12):2080-2087.
By Christopher R. Zieker, MD
It is estimated that one in three people in the United States has a cornea that is not perfectly round, causing blurry vision that may be worsened by myopia or hyperopia.1 With such a high prevalence of astigmatism, it is not surprising that surgeons have developed a variety of approaches to correcting it.
Most patients have a minimum goal of clear uncorrected distance vision. Although I do not promise my patients 20/20 UCVA, my objective is to choose the correct lens power and manage astigmatism to get them within a couple of lines of the bottom of the eye chart. Doing so will allow them to drive during the day and at night legally, watch television, and generally function without distance glasses. If the lens power is correct, 0.75 D or more of residual astigmatism can transform the outcome from sharp 20/25 to blurry 20/40 UCVA. Although some patients have worn glasses for astigmatism their whole life and do not mind continuing to use them, a higher quality of vision is very important to others.
Laser arcuate incisions and limbal relaxing incisions (LRIs) can correct approximately 1.00 to 1.25 D of cylinder or less very well. Toric IOLs and LRIs are both acceptable choices to address higher amounts of astigmatism. For each patient, the best treatment takes into account risk, benefit, and cost. Because I can successfully correct up to 4.00 D of astigmatism with an LRI at a significantly lower cost than for a toric IOL, many of my patients choose the former treatment option. The predictability of LRIs decreases from the usual 95% to approximately 80% to 85% when treating astigmatism ranging from 3.00 to 4.00 D. It is important to inform patients of this difference when they cannot afford a toric IOL.
When patients want to be rid of their bifocal glasses after cataract surgery, I find that performing an LRI to correct astigmatism allows me also to implant a multifocal IOL such as the Tecnis Multifocal (Abbott Medical Optics). In my experience, this lens provides patients with clear UCVA at distance and near. I do not think it is reasonable to tell patients that they cannot have the desired multifocal lens simply because they have 2.00 to 3.00 D of astigmatism.
Toric lenses are typically better than an LRI or laser arcuate incision for patients who have irregular astigmatism or are at risk of being somewhere on the keratoconus spectrum. Even patients with forme fruste keratoconus are at increased risk of ectasia if LRIs or laser arcuate incisions are used. Moreover, some patients simply prefer to receive a toric IOL, and when properly placed, these lenses make patients very happy. n
1. Vitale S, Ellwein L, Cotch MF, et al. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126:1111-1119.
Elizabeth Yeu, MD
• assistant professor of ophthalmology, Eastern Virginia Medical School, Ghent, Virginia
• partner specializing in cornea, cataract, and refractive surgery at Virginia Eye Consultants, Norfolk, Virginia
• (757) 622-2200; eyeu@vec2020.com
• financial disclosure: consultant to Abbott Medical Optics, Alcon, and i-Optics
Christopher R. Zieker, MD
• cataract and refractive surgeon in Wilton, New York
• recipient of America’s Most Compassionate Doctors award in 2011, 2012, and 2013
• (518) 450-1080; czieker@ziekereye.com; www.ziekereye.com
• financial disclosure: none acknowledged


