Cataract surgery in patients with vitreoretinal disease poses challenges for both anterior segment and retinal specialists. Level 1 evidence regarding the optimal perioperative management of these patients—including those with age-related macular degeneration (AMD), diabetic macular edema (DME), and uveitis—is unavailable to guide best practices. Recent studies report that favorable outcomes can be achieved, however, and this research emphasizes the preoperative control of cystoid macular edema and inflammation in particular.
UVEITIS
No randomized controlled studies exist to determine the optimal perioperative treatment regimen for cataract surgery on patients with uveitis. Reflecting this gap, the American Academy of Ophthalmology Preferred Practice Patterns guidelines state that treatment must be individualized, given each patient’s comorbid systemic disease, the expected duration of therapy, and his or her preferences.1
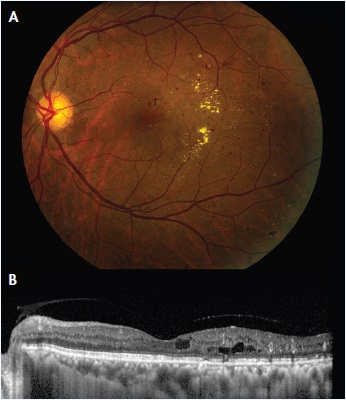
Figure 1. Fundus photograph (A) and enhanced depth imaging optical coherence tomography (OCT) scan (B) of a 59-year-old patient with DME. A report by the DRCR.net found that prior treatment for DME or preoperative DME increases the risk of center-involving DME postoperatively.7
The key to successful outcomes in patients with uveitis remains strict preoperative control of inflammation. In general, uveitis specialists maintain that inflammation must be quiet for at least 3 months prior to cataract extraction, an approach that has support in the literature.2 Favorable outcomes can be achieved in this population. A recent meta-analysis of 89 studies by Mehta et al found that a visual acuity of 20/40 or better was achieved in 68% of uveitic patients undergoing phacoemulsification when inflammation was “quiet or mostly quiet” at the time of surgery.3
The choice of IOL for adults with uveitis remains a matter of debate. Leung et al found insufficient evidence to recommend a particular IOL for patients with uveitis in a 2014 Cochrane Review.4 Mehta et al, however, reported poorer outcomes with silicone IOLs, suggesting that other materials may be preferable.3
Counseling is mandatory for patients with uveitis, because postoperative complications such as glaucoma, posterior capsular opacification, and cystoid macular edema are common.5,6 Comanagement with a uveitis specialist is advisable.
DIABETIC MACULAR EDEMA
The prevention of postoperative DME is imperative for achieving favorable outcomes after cataract surgery in diabetic patients. In a recent report by the DRCR.net,7 Baker et al found that 11% of patients with DME not involving the center on OCT developed center-involving DME 16 weeks after cataract surgery (Figure 1). Prior treatment for DME was associated with an increased risk of postoperative center-involving DME (P < .001).
Level 1 evidence regarding the optimal treatment for DME prior to and after cataract surgery is unavailable. In patients with persistent disease despite consistent antivascular endothelial growth factor (anti-VEGF) or focal laser therapy, no data exist to suggest that cataract surgery must be deferred until the complete resolution of DME. In our practice, patients with center-involving DME are treated until the level of edema is deemed stable, based upon OCT findings, clinical examination, and visual acuity. Once stable, patients are then treated 1 to 2 weeks prior to cataract extraction and are reevaluated 4 weeks after the last anti-VEGF treatment. Given the data from the DRCR.net, patients without center-involving DME are evaluated 1 month after cataract extraction and no later than 16 weeks after cataract surgery to assess them for DME occurrence.
Numerous studies have reported a statistically significant reduction in postoperative macular edema, stabilization of central macular thickness, and better BCVA8-10 when anti-VEGF treatment is used prior to or at the time of cataract surgery in diabetic patients with or without baseline DME. Confirmatory data and future research on efficacy, patient selection, and the ideal timing of preoperative treatment will be of particular interest. Given the available evidence, however, the “prophylactic” anti-VEGF treatment of patients without center-involving DME cannot be recommended and may result in overtreatment.
AGE-RELATED MACULAR DEGENERATION
Data from large, prospective AMD trials have demonstrated good visual acuity results in patients with AMD undergoing cataract surgery without increased progression to neovascular AMD. The Age-Related Eye Disease (AREDS) 2 study found that visual acuity improved in all AMD disease severity groups (P < .0001) 5 years after cataract surgery in 1,232 eyes of 793 patients with mild, moderate, severe, noncentral geographic atrophy, or advanced AMD.11 Similarly, work by the AREDS study group found no increased risk of progression to neovascular AMD after cataract extraction at 5 years.12
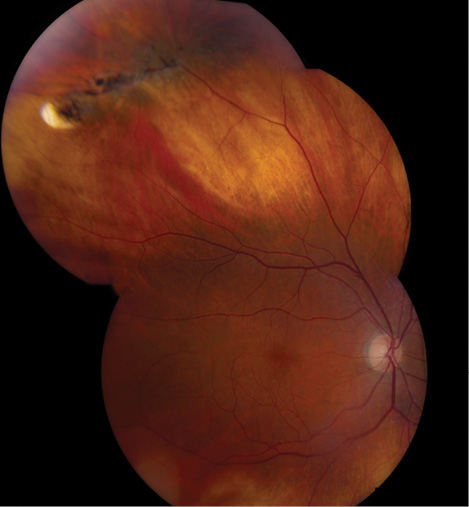
Figure 2. Lattice degeneration without associated retinal breaks in a 62-year-old patient. No level 1 evidence exists regarding the necessity of prophylactic laser retinopexy or cyrotherapy prior to cataract extraction for these lesions, and treatment should be individualized.
Also encouraging, recent retrospective studies have not shown an increased anti-VEGF treatment burden after cataract extraction.13,14 Such data are useful for counseling patients regarding the risk of neovascular complications after cataract surgery. Prospective studies are needed to determine the optimal timing and level of exudative control required to maximize cataract surgery outcomes in patients with neovascular disease.
POSTERIOR VITREOUS DETACHMENT AND RETINAL DETACHMENT
The evolution of posterior vitreous detachment has been implicated in pseudophakic rhegmatogenous retinal detachment.15,16 Described risk factors include a history of retinal detachment in the fellow eye, a long axial length, lattice degeneration, posterior capsular rupture, male gender, and younger age.17,18
Level 1 data regarding the prophylactic treatment of peripheral retinal pathology, including lattice degeneration and atrophic retinal holes, prior to cataract surgery or after an Nd:YAG laser capsulotomy are unavailable (Figure 2). We mostly consider prophylactic laser retinopexy of peripheral retinal pathology for patients with a history of a retinal tear or detachment in the fellow eye, but treatment is determined on a case-by-case basis. Further data from a prospective study would be of interest to cataract and retinal physicians alike.
ENDOPHTHALMITIS
There is currently no consensus on the use of intracameral antibiotics for the prophylaxis of endophthalmitis after cataract extraction,19 but recent reports in the United States and Japan have been promising. Storestein et al found a 22-fold decrease in the endophthalmitis rate with the use of intracameral antibiotics,20 whereas Matsuura et al reported a threefold reduction.21 Further study of the use of intracameral antibiotics will be of interest, particularly in patients with posterior capsular rupture who may be at elevated risk of postcataract endophthalmitis.
CONCLUSION
Cataract surgery on patients with coexisting retinal disease can be completed safely with favorable visual outcomes. Prospective data will help to clarify the timing, nature, and necessity of perioperative treatments. n
1. Uveitis and Cataract Surgery - 2013 - American Academy of Ophthalmology. http://one.aao.org/clinical-questions/uveitis-cataract-surgery. Accessed April 9, 2015.
2. Bélair M-L, Kim SJ, Thorne JE, et al. Incidence of cystoid macular edema after cataract surgery in patients with and without uveitis using optical coherence tomography. Am J Ophthalmol. 2009;148(1):128-135.e2.
3. Mehta S, Linton MM, Kempen JH. Outcomes of cataract surgery in patients with uveitis: a systematic review and meta-analysis. Am J Ophthalmol. 2014;158(4):676-692.e7.
4. Leung TG, Lindsley K, Kuo IC. Types of intraocular lenses for cataract surgery in eyes with uveitis. Cochrane Database Syst Rev. 2014;3:CD007284.
5. Rahman I, Jones NP. Long-term results of cataract extraction with intraocular lens implantation in patients with uveitis. Eye Lond Engl. 2005;19(2):191-197.
6. Ram J, Gupta A, Kumar S, et al. Phacoemulsification with intraocular lens implantation in patients with uveitis. J Cataract Refract Surg. 2010;36(8):1283-1288.
7. Diabetic Retinopathy Clinical Research Network Authors/Writing Committee, Baker CW, Almukhtar T, et al. Macular edema after cataract surgery in eyes without preoperative central-involved diabetic macular edema. JAMA Ophthalmol. 2013;131(7):870-879.
8. Chae JB, Joe SG, Yang SJ, et al. Effect of combined cataract surgery and ranibizumab injection in postoperative macular edema in nonproliferative diabetic retinopathy. Retina. 2014;34(1):149-156.
9. Lanzagorta-Aresti A, Palacios-Pozo E, Menezo Rozalen JL, Navea-Tejerina A. Prevention of vision loss after cataract surgery in diabetic macular edema with intravitreal bevacizumab: a pilot study. Retina. 2009;29(4):530-535.
10. Takamura Y, Kubo E, Akagi Y. Analysis of the effect of intravitreal bevacizumab injection on diabetic macular edema after cataract surgery. Ophthalmology. 2009;116(6):1151-1157.
11. Age-Related Eye Disease Study 2 Research Group, Huynh N, Nicholson BP, et al. Visual acuity after cataract surgery in patients with age-related macular degeneration: Age-Related Eye Disease Study 2 report number 5. Ophthalmology. 2014;121(6):1229-1236.
12. Chew EY, Sperduto RD, Milton RC, et al. Risk of advanced age-related macular degeneration after cataract surgery in the Age-Related Eye Disease Study: AREDS report 25. Ophthalmology. 2009;116(2):297-303.
13. Tabandeh H, Chaudhry NA, Boyer DS, et al. Outcomes of cataract surgery in patients with neovascular age-related macular degeneration in the era of anti-vascular endothelial growth factor therapy. J Cataract Refract Surg. 2012;38(4):677-682.
14. Grixti A, Papavasileiou E, Cortis D, et al. Phacoemulsification surgery in eyes with neovascular age-related macular degeneration. ISRN Ophthalmol. 2014;2014:417603.
15. Ripandelli G, Coppé AM, Parisi V, et al. Posterior vitreous detachment and retinal detachment after cataract surgery. Ophthalmology. 2007;114(4):692-697.
16. Hilford D, Hilford M, Mathew A, Polkinghorne PJ. Posterior vitreous detachment following cataract surgery. Eye Lond Engl. 2009;23(6):1388-1392.
17. Tielsch JM, Legro MW, Cassard SD, et al. Risk factors for retinal detachment after cataract surgery. A population-based case-control study. Ophthalmology. 1996;103(10):1537-1545.
18. Bhagwandien ACE, Cheng YYY, Wolfs RCW, et al. Relationship between retinal detachment and biometry in 4262 cataractous eyes. Ophthalmology. 2006;113(4):643-649.
19. Schimel AM, Alfonso EC, Flynn HW. Endophthalmitis prophylaxis for cataract surgery: are intracameral antibiotics necessary? JAMA Ophthalmol. 2014;132(11):1269-1270.
20. Shorstein NH, Winthrop KL, Herrinton LJ. Decreased postoperative endophthalmitis rate after institution of intracameral antibiotics in a Northern California eye department. J Cataract Refract Surg. 2013;39(1):8-14.
21. Matsuura K, Miyoshi T, Suto C, et al. Efficacy and safety of prophylactic intracameral moxifloxacin injection in Japan. J Cataract Refract Surg. 2013;39(11):1702-1706.
Allen C. Ho, MD
• director of retina research, Wills Eye Hospital, Philadelphia
• professor of ophthalmology, Thomas Jefferson University, Philadelphia
• (215) 928-3300; acho@att.net
M. Ali Khan, MD
• vitreoretinal surgery fellow, Retina Service, Wills Eye Hospital, Philadelphia
Keegan Skidmore, BA
• medical student, Warren Alpert Medical School of Brown University, Providence, Rhode Island