CASE PRESENTATION
A 56-year-old White man presents with a desire for vision correction. The patient’s manifest refraction is +7.50 -6.75 x 102º = 20/16 OD and +5.75 -2.00 x 83º = 20/12 OS. The optical media are clear. The corneas, retinas, and optic nerves are unremarkable. There are no significant findings in his general or ocular history.
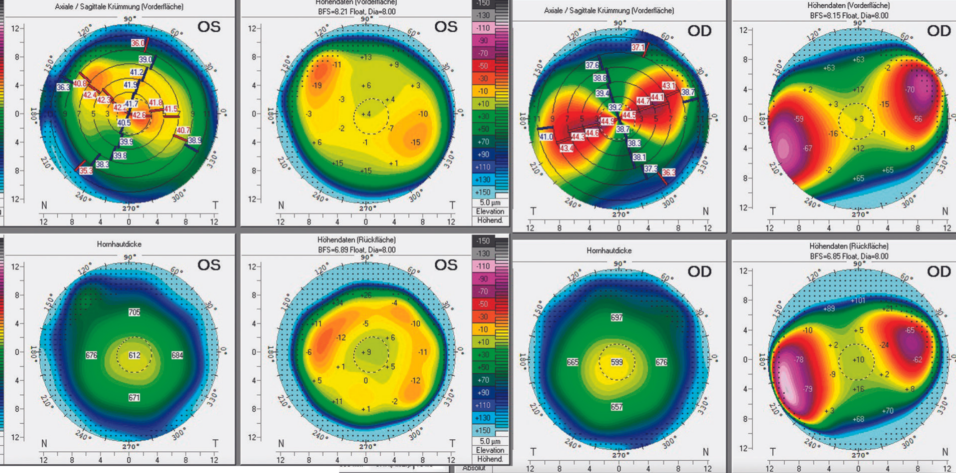
Imaging with the Pentacam (Oculus Optikgeräte; Figure) shows 5.70 D of regular corneal astigmatism with a maximum keratometry value of 44.70 D OD and 1.30 D of regular corneal astigmatism with a maximum keratometry value of 42.40 D OS. The anterior chambers are shallow, and the angles are narrow.
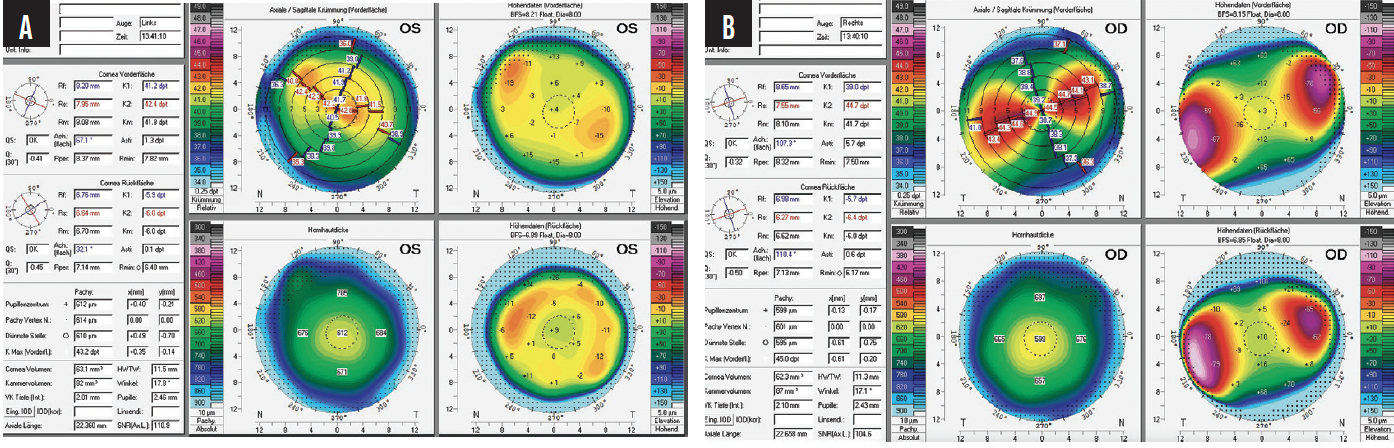
Figure. Scheimpflug imaging of the left (A) and right (B) eyes. The anterior chambers are shallow, and the angles are narrow.
How would you proceed?
—Case prepared by Suphi Taneri, MD, FEBOS-CR

AYLIN KILIÇ, MD
Based on the patient’s age and refraction, I would recommend an intraocular approach. Amblyopia is evident in the right eye; the spherical target would be -1.50 D to provide near vision. Emmetropia would be targeted in the left eye. A monofocal toric IOL would be a reasonable choice. Because of the high corneal astigmatism, however, a bioptics approach would be my preference. Residual astigmatism could be corrected 6 months after the implantation of a monofocal toric IOL.
Preoperative counseling would be important because a period of neural adaptation to monovision may be required after surgery. The shallow anterior chamber and narrow angles would receive careful evaluation because they could increase the risk of endothelial damage during surgery.

THEO G. SEILER, MD, FEBO
To my mind, the patient is a candidate for clear lens exchange. The high amount of hyperopic astigmatism to be corrected and his age are contraindications for a primary corneal refractive procedure, and the shallow anterior chambers make the implantation of a phakic IOL impossible. The question is what sort of toric lens to implant—monofocal, extended depth of focus (EDOF), or trifocal?
Assuming postoperative IOL rotation of 3º and a 3% reduction of the astigmatic correction per degree, the predicted postoperative manifest astigmatism is greater than 0.50 D. I would therefore avoid a diffractive toric trifocal or diffractive EDOF IOL in favor of either a toric monofocal or toric nondiffractive EDOF IOL with or without monovision. A contact lens trial would be performed. Thorough counseling to set reasonable patient expectations would be required before the choice of IOL is finalized.

PAVEL STODULKA, MD, PHD
The concept of laser lenticule rotation as a variation on SMILE may be attributed to Jesper Hjortdal, MD, PhD.1 My colleagues and I published the world’s first clinical cases.2 During laser lenticule rotation, an intrastromal SMILE lenticule with half the astigmatism power is created with a femtosecond laser. The lenticule is not extracted, as in classic SMILE surgery, but rotated 90º in the stromal pocket and left in place. The strategy can correct astigmatism and produce a myopic shift. Based on my clinical experience, there is a good chance that the patient in this case can achieve emmetropia or very low residual ametropia. Lenticule rotation is a challenging new surgery that can correct high amounts of astigmatism without removing ocular tissue.
The second option for the patient is refractive lens exchange with toric IOL implantation. My preference would be a trifocal toric IOL, which would give the patient a high likelihood of postoperative spectacle independence. Some degree of dysphotopsia due to the diffractive technology would be expected. I achieved successful clinical results with the world’s first implantations of the hydrophobic FineVision HP Toric (BVI Medical) in patients who had up to 8.00 D of cylinder. The IOL has demonstrated reliable rotational stability and delivered high patient satisfaction thus far.
I would avoid LASIK for such a high amount of hyperopic astigmatism because postoperative refractive stability and optical quality are typically suboptimal.

WHAT I DID: SUPHI TANERI, MD, FEBOS-CR
Because of the patient’s immense ametropia, staged surgery was planned. First, femtosecond LASIK was performed with the VisuMax 500 (Carl Zeiss Meditec) and Technolas Teneo 317 Model 2 (Bausch + Lomb) to correct most of the corneal astigmatism and half of the hyperopia.
The targeted refraction was +4.00 -4.75 x 100º OD and +3.75 -2.00 x 80º OS. Following treatment, the patient was able to wear glasses more comfortably (+4.00 -3.00 x 110º OD and +3.00 -1.00 x 75º OS). After refractive stability was documented, he underwent refractive lens exchange with a toric IOL (Ankoris, PhysIOL) in the right eye and an aspheric IOL (Akreos Adapt AO, Bausch + Lomb) in the left eye.
Three months postoperatively, the patient’s UCVA was 0.8 OD, 1.0 OS, and 1.33 OU. His BCVA was 1.0 OU with a manifest refraction of -0.25 -0.50 x 160º OD and +0.25 -0.75 x 50º OS. At the slit lamp, early posterior capsular fibrosis was visible, but immediate treatment was not deemed necessary.
1. Damgaard IB, Ivarsen A, Hjortdal J. Intrastromal lenticule rotation for treatment of astigmatism up to 10.00 diopters ex vivo in human corneas. J Refract Surg. 2019;35(7):451-458.
2. Stodulka P, Hjortdal J, Slovak M. Intrastromal lenticule rotation for the treatment of astigmatism. J Refract Surg. 2020;36(6):415-418.