Patients have a growing number of choices when it comes to presbyopia treatment, and clear communication is key to making sure they understand the pros and cons of each option.
MONOVISION LASIK
Monovision using laser correction is one of the most established means of correcting presbyopia. It also is the easiest and cheapest surgical method that patients have available to them. To review, this treatment induces anisometropia or a difference in vision between the two eyes. The consequence can be a reduction in binocular acuity and stereopsis. The dominant eye is corrected for distance vision, and the nondominant eye is corrected for near vision.
It is important to communicate to patients that the vision in the near eye will be purposely blurry at distance. The near vision is commonly corrected in the vicinity of -1.25 to -2.00 D. It is best to trial frame the correction for a patient or to perform a contact lens trial prior to the laser vision correction. This treatment is easy to perform with existing technology and provides immediate results.
AT A GLANCE
- LASIK monovision and corneal inlays are effective for treating presbyopia.
- LASIK monovision is quick and fairly inexpensive, but it decreases stereopsis and will not help patients once they develop cataracts. Inlays preserve stereopsis and should provide near vision even after cataract surgery.
- It important to explain to patients what they can expect immediately and how their vision will change over time.
Patients should be aware of the downsides as well. The treatment is permanent, even if their near vision needs change as they age. Surgery diminishes stereopsis and binocularity, and it only provides near vision in the treated eye. Finally, it makes later cataract surgery calculations more difficult and does not continue to work after that procedure.
Corneal Inlays
Corneal inlays for the treatment of presbyopia only recently became available in the United States. The FDA approved the Kamra (AcuFocus) in 2015 and the Raindrop Near Vision Inlay (ReVision Optics) in 2016.
Kamra
The surgeon makes a deep corneal pocket with a femtosecond laser. The inlay, which has a 1.6-mm central aperture and is made of polyvinylidene fluoride, increases depth of field by using the pinhole effect to improve near and intermediate vision without significantly affecting distance vision. In a pivotal trial, almost 90% of eyes treated with the Kamra saw 20/40 or better 36 months after implantation.1
The inlay is placed within the corneal pocket and then centered over the optical axis with the help of an AcuTarget HD Analyzer (Visiometrics) mounted on the operating microscope. FDA-approved candidates are patients 45 to 60 years of age with a spherical equivalent correction of +0.50 to -0.75 D with up to 0.75 D of astigmatism who need reading glasses.1
The Kamra inlay is only indicated for use in the nondominant eye of the patient. Vision can take 1 to 3 months to stabilize. Contrast sensitivity may be compromised in the treated eye, particularly at nighttime or in dim light.1
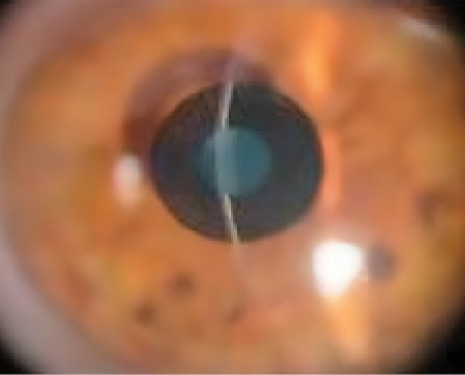
Figure 1. Kamra inlay.
Raindrop
The Raindrop Near Vision Inlay is a transparent hydrogel implant that is 2 mm in diameter and 30 μm thick. The water content of the inlay is similar to that of the cornea itself. The device is placed under a LASIK flap that is 30% central corneal depth. The surgeon lifts the LASIK flap and places the inlay over the light-constricted pupil. No special instrumentation is needed to place or center the inlay, because exact centration is not critical to the increased depth of focus created by the steepening of the central cornea.
The Raindrop inlay provides an average gain of 5 lines in near vision and 3 lines in intermediate vision. Distance vision remains good, with an average of 1 line of BCVA lost. Immediate improvement in near vision is noted after the procedure, with stabilization of vision within 1 month. There is little effect on contrast sensitivity.2
When discussing these technologies with patients, it is important to explain what to expect immediately and how their vision will change and improve over time. If off-label treatment for ametropia is considered along with the inlay, the pros and cons need to be discussed as well. Review medication protocols with an emphasis on follow-up to watch out for any untoward reactions.
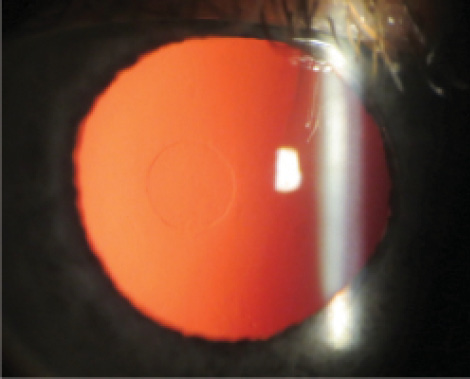
Figure 2. Raindrop inlay retro image.
Candidates
All inlays require that the eye be free of disease and that the cornea be healthy enough for LASIK surgery. Thickness of the cornea must be suitable for the pocket or flap required as well. Postoperatively, patients must comply with strict medical drop regimens to avoid inflammatory fibrosis, which could compromise vision and/or necessitate the removal of the device.
Advantages
The implantation of corneal inlays is a straightforward procedure using a femtosecond laser. They give a continuous range of vision (near, intermediate, and distance) in the treated eye without diminished stereopsis or diminished binocularity. They should continue to work after cataract surgery is performed, and they are removable.
Disadvantages
A centration device and pocket software are needed for Kamra insertion, and the patient may experience decreased contrast sensitivity in the treated eye. Both inlays require approximately 3 months of steroid drops, and inflammatory fibrosis can necessitate removal of the device. Neither one is approved for concomitant LASIK to correct ametropias or astigmatism in the treated eye.
WATCH IT NOW
Howard Gimbel, MD, shares an edited-down version of the Kamra inlay (AcuFocus) procedure.
CONCLUSION
LASIK monovision and corneal inlays are both effective alternatives for treating presbyopia, but clear communication is key to success with either strategy. By explaining the pros and cons of the chosen modality and discussing setting realistic expectations for the immediate and long term, surgeons can maximize patients’ satisfaction.
1. AcuFocus. Kamra inlay professional use information. http://www.accessdata.fda.gov/cdrh_docs/pdf12/P120023d.pdf. Accessed December 8, 2016.
2. Whitman J, Dougherty PJ, Parkhurst, GD, et al. Treatment of presbyopia in emmetropes using a shape-changing corneal inlay: one-year clinical outcomes. Ophthalmology. 2016;123:466-475.