Case Presentation
A 49-year-old man presents for a cataract surgery consultation. The patient reports decreased visual acuity in each eye. He received a Verisyse phakic IOL (Johnson & Johnson Vision) through a superior incision in each eye 15 years ago.
Upon examination, BCVA is 20/25 with a manifest refraction of -1.75 +0.50 x 005º OD, and glare testing reduces visual acuity to 20/100 OD. In the left eye, BCVA is 20/30 with a manifest refraction of -3.50 +0.75 x 175º, and glare testing reduces visual acuity to 20/200.
A slit-lamp examination reveals a clear cornea and a well-centered phakic IOL in each eye (Figure). The right eye has a 1+ nuclear sclerotic cataract and a 1+ posterior subcapsular cataract. The left eye exhibits mild anterior capsular changes and has a 1+ nuclear sclerotic cataract and a 3+ posterior subcapsular cataract. A dilated fundus examination shows mild myopic degeneration but no holes, breaks, or tears. The endothelial cell count is 2,400 cells/mm2 in the right eye and 2,000 cells/mm2 in the left. An OCT scan of the retina is normal in each eye.
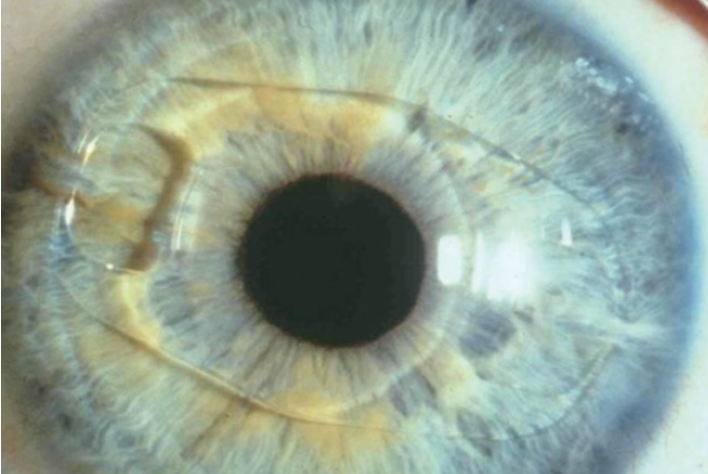
Figure. A Verisyse phakic IOL in situ in the left eye.
The patient is concerned about seeing glare at night. He expresses a desire for good midrange vision. He does not want monovision but would instead like the visual acuity in his left eye to be similar to that in his right.
How would you proceed? Would you offer laser cataract surgery? Where would you place the cataract incision, and which IOL would you offer to this patient? Are you concerned about the endothelial cell count?
—Case prepared by Audrey R. Talley Rostov, MD
RUPERT MENAPACE, MD, FEBO

Iris-fixated phakic IOLs are an effective and safe option for correcting myopia. Implantation of a nonfoldable PMMA Verisyse lens with a 5-mm optic requires a large incision that can induce significant astigmatism, particularly when the incision is created in clear cornea. I recommend against using a femtosecond laser for surgery in this case because the gas that accumulates between the IOL and the crystalline lens could cause a radial anterior capsular tear.
I would explant the phakic IOL through a superior frown incision and then perform cataract surgery using a temporal approach under topical and intracameral anesthesia. To begin the explantation, after asking the patient to look down, I would create a superior fornix-based conjunctival flap and a 4.5-mm scleral frown incision located as posteriorly as possible. Next, I would dissect a 5.5-mm sclerocorneal tunnel and create a 2.2-mm central corneal lip. After exchanging the aqueous for a cohesive OVD, I would use a pair of Artiflex implantation forceps (Ophtec, not available in the United States) to grasp the haptic base and disenclavate the iris with a needle passed through paracenteses at the 10 and 2 clock positions. After enlargement of the corneal lip to 5.5 mm, the IOL would be rotated vertically and explanted while the endothelium was protected with a spatula.
Standard temporal-access 2.2-mm posterior-limbal cataract surgery would follow with a related use of a dispersive OVD during phacoemulsification.
The choice of replacement IOL depends on the quality of the patient’s preoperative corneal topography. Asymmetric bow tie astigmatism resulting from the implantation of a Verisyse lens through a superior corneal incision would decrease the optical performance of multifocal and extended depth of focus IOLs. The planned posteriorly positioned 5.5-mm frown incision would avoid inducing additional astigmatism during explantation of the phakic IOL. A toric trifocal lens could be considered. An excimer laser enhancement might be required to optimize the refractive result but should not be performed before 6 months have elapsed in case the cataract incision sags and induces a change in astigmatism.1
SIMONETTA MORSELLI, MD

I would counsel this patient on his low endothelial cell counts and his possible future need for an endothelial cell transplant. I would offer to perform cataract surgery and implant a monofocal IOL. When performing the IOL power calculation, I would target -2.00 D to obtain the same postoperative refraction as the right eye.
The pupil would not be dilated before surgery. After the conjunctiva had been opened from the 11 to the 2 clock position, a 4.5-mm scleral frown incision would be created at the 12 clock position, and a 2.2-mm temporal corneal sideport incision would be created. Under a cohesive OVD, the phakic IOL would be disenclavated with special forceps and a manipulator. After explantation of the IOL, the scleral incision would be closed with a 10-0 nylon suture, and the conjunctiva would be closed with an 8-0 polyglactin suture (Vicryl, Ethicon).
A mydriatic solution would be administered through the 2.2-mm temporal clear corneal incision created for disenclavation of the phakic IOL. Cataract surgery would be performed through this same incision under a cohesive OVD. I would perform phacoemulsification according to my usual technique and insert a monofocal IOL into the capsular bag. I would not suture the incision at the conclusion of surgery.
MAJID MOSHIRFAR, MD; AND MARGARET H. SHMUNES, BS

This patient appears to have been highly myopic (> -15.50 D) given that this appears to be a 5.0-mm Verisyse model 206 phakic lens. I (M.M.) would proceed with conventional cataract surgery because laser cataract surgery could pose several risks in this case. For example, the endothelial cell count is already lower than normal; the average range for a man this age, according to the literature,2 is 2,200 to 3,500 cells/mm2. The docking of a femtosecond laser could contribute to endothelial contusion in the periphery because of the close proximity of the phakic lens to the iris.
Moreover, I (M.M.) want to create a concentric capsulorhexis. Because of the enclavation site of the phakic lens along the horizontal meridian, the pupil probably will not dilate uniformly along that meridian. This could limit the geometric centration of a laser capsulotomy.
I (M.M.) would initially make a 5-mm self-sealing scleral frown incision superiorly through which I would disenclavate, rotate, and remove the phakic lens, but I recommend proceeding with the cataract extraction through a temporal 2.4-mm clear corneal incision. (A similar case may be viewed at bit.ly/0920CRSTCSCase.)
I (M.M.) would avoid choosing a multifocal lens for this patient because he has expressed concern about glare. I would use the axial length adjustment recommended by Douglas D. Koch, MD, and the SRK/T formula. The patient desires midrange vision, so a standard one-piece monofocal IOL would be a reasonable choice. If the white-to-white corneal diameter is larger than 12.7 mm or the anterior chamber is large, I (M.M.) would prefer to implant a three-piece Sensar IOL (model AR40, Johnson & Johnson Vision).
To protect the endothelium, a generous amount of a dispersive OVD would be instilled after each step of the cataract procedure. The preoperative discussion with the patient should cover the risk of further endothelial cell loss,3 his potential need for an endothelial transplant, and the cumulative risk of a retinal detachment.4
SHERI ROWEN, MD, FACS

In challenging cases such as this one, it is clear that a 6-mm incision will be required just to extract the phakic IOL. This patient obviously has a clinically significant cataract that requires removal. I would want to know the keratometry readings from before and after phakic IOL surgery in order to determine the effect of the earlier 6-mm incision. The current amount of refractive cylinder is acceptable after a large superior 6-mm incision, but it is important to determine the change over time. I would also like to see the current topographic maps in order to assess the regularity of the cornea.
This patient’s endothelial cell count is lower than normal. I would try to use a Ziemer Femto LDV femtosecond laser to perform the capsulotomy and fragment the cataractous lens because I believe this will be less traumatic to the endothelial cells than a manual approach. All the laser energy would be under the Verisyse phakic IOL and the energy fragmenting the lens would be contained within the lens as the last part of the procedure with this laser is the capsulotomy. I would create the corneal and scleral incisions manually unless arcuate incisions are needed to treat astigmatism. I would prefer to avoid arcuate incisions, however, because a large incision has already been made in this eye and, if another is added, this could destabilize the cornea over time.
I would enter the eye temporally to avoid weakening the prior incision located superiorly and to facilitate access to the phakic lens for disenclavation. I would create two sideport incisions followed by a 6-mm incision to avoid or minimize the induction of astigmatism. My preference would be a limbal-scleral approach (as for small-incision cataract surgery) in order to have the least direct effect on corneal tissue. The phakic lens would then be disenclavated and removed through the temporal incision. The edges of the incision would be sutured, leaving only sub–3-mm access for phacoemulsification and IOL implantation.
This patient with high myopia has enjoyed excellent vision with a phakic IOL. He wants to retain the best possible night vision and intermediate vision. Two IOLs can probably meet these demands: the AcrySof IQ Vivity (Alcon) and the Crystalens AO (Bausch + Lomb). The AcrySof IQ Vivity lens is an extended range of vision IOL designed to provide intermediate vision with a profile similar to that of a monofocal lens. The Vivity is not diffractive and has no rings, but by shifting and stretching the intermediate zone of vision it can offer this range without some of the issues encountered with other multifocal IOLs. This lens was recently approved by the FDA. The Crystalens (lowest available power, 4.00 D) will most likely provide the intermediate visual acuity this patient desires as well as good distance visual acuity while minimizing glare at night. If the axial length is greater than 26 mm, I would use the Wang-Koch formula adjustment and the Holladay 1 formula.
I would expect this patient to do very well.
WHAT I DID: AUDREY R. TALLEY ROSTOV, MD

I decided to perform laser cataract surgery using the Lensar Laser System (Lensar) in an effort to minimize endothelial cell loss. The laser capsulotomy and phacofragmentation were executed without complication. I then created a 6-mm temporal incision, injected a dispersive OVD (Viscoat, Johnson & Johnson Vision), disenclavated the Verisyse lens with an enclavation needle, and explanted the IOL.
After hydrodelineation and hydrodissection of the fragmented cataract, the pieces were easily removed with irrigation as part of a modified technique of small-incision cataract surgery. Two sutures were placed in the temporal incision, and the cortex was removed with bimanual irrigation and aspiration using a low infusion pressure. A three-piece SofPort lens (model LI61AO, Bausch + Lomb) was implanted; the targeted postoperative refraction was -1.50 D. The patient was pleased with the outcome.
Watch it Now
1. Menapace R, Vass C, Hirsch U, Strenn K. A simple, safe and stable alternative to the frown incision for implantation of PMMA intraocular lenses with a large optic diameter. Spektrum Augenheilkd. 1996;10:237-240.
2. Galgauskas S, Norvydaite D, Krasauskaite D, Stech S, Stanislovas Ašoklis R. Age-related changes in corneal thickness and endothelial characteristics. Clin Interv Aging. 2013;8:1445-1450.
3. Moshirfar M, Imbornoni LM, Ostler EM, Valliammai M. Incidence rate and occurrence of visually significant cataract formation and corneal decompensation after implantation of Verisyse/Artisan phakic intraocular lens. Clin Ophthalmol. 2014;8:711-716.
4. Ohno-Matsui K, Kawasaki R, Jonas JB, et al; META-analysis for Pathologic Myopia (META-PM) Study Group. International photographic classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015;159(5):877-883.e7.




