Case Presentation
A 45-year-old man presented with a 1-year history of intermittent pain in his left eye on waking that has failed to respond to conservative measures. The patient has a long-standing scar in the cornea of his right eye that has left him with poor visual acuity (Figures 1–3). UCVA is 20/200 OD. Refraction produces minimal improvement, but pinhole visual acuity is 20/30. UCVA is 20/20 OS.
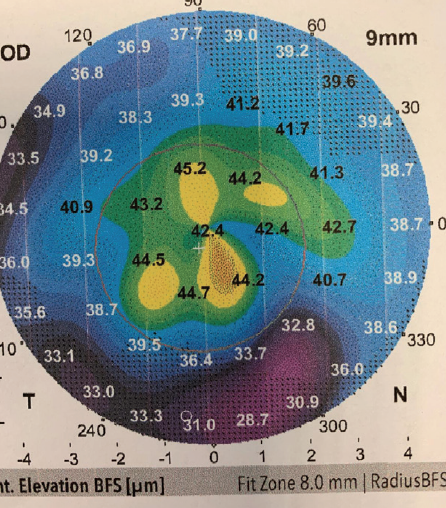
Figure 1. Topography of the right cornea.
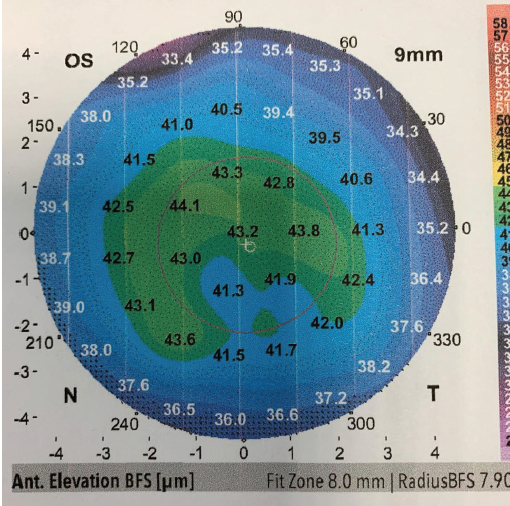
Figure 2. Topography of the left cornea.
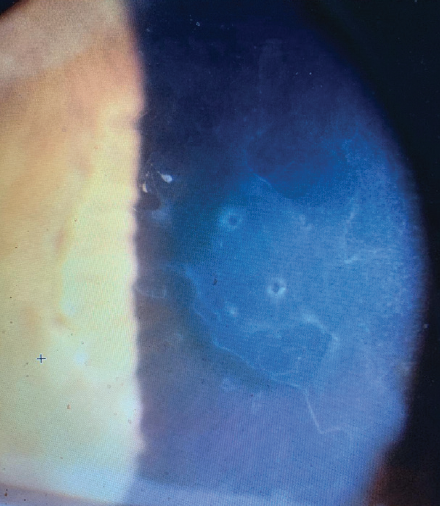
Figure 3. The cornea of the left eye.
How would you optimize vision in the patient’s right eye and treat the symptoms in the left eye?
—Case prepared by Allon Barsam, MD, FRCOphth
A. JOHN KANELLOPOULOS, MD

The intermittent pain upon waking is textbook recurrent erosion from map-dot-fingerprint dystrophy, also known as anterior epithelial basement membrane dystrophy and epithelial basement membrane dystrophy (EBMD), or a previous epithelial abrasion. The binocular nature establishes the former diagnosis, although EBMD is more common in female patients.
The Placido disc–based reflection topography provided shows several solitary and some confluent steep islands scattered centrally, more so in the right eye, which confirm the aforementioned diagnosis and represent areas of thickened or doubled dots of epithelium (Cogan cysts). In my experience, images obtained early in the day show more pronounced findings (anterior segment OCT epithelial mapping is fantastic for this) because the diurnal evaporation of corneal moisture can improve symptoms and imaging. The external photograph clearly illustrates Cogan cysts (the dot element) and map-like and fingerprint-like superficial epithelial findings in the left eye that match the topography. The whiter areas represent reduplication and/or poor attachment of the epithelium.
Phototherapeutic keratectomy (PTK) would be my treatment of choice for each eye. I would avoid transepithelial laser scraping, which would imprint the anterior surface irregularity onto the underlying stroma. Instead, I would thoroughly remove the epithelium manually; most of the epithelium should slough off easily, but remnants may require removal with a hockey-stick blade or an Epi Clear device (Orca Surgical), which is a favorite of mine. I would then ablate a mere 8 to 10 µm of Bowman membrane in the left eye. If the scarring in the right eye involves Bowman membrane and the superficial stroma, a deeper ablation may be required to create the scaffold for tight hemidesmosome adhesion during reepithelialization. Because the pathology is within the central 8 mm (the usual maximum optical zone for excimer lasers), this treatment may suffice. The unknown here is the actual underlying refraction that will be accurately established after PTK, so the quest for emmetropia may require a second round of surface ablation.
ALI MEARZA, MBBS, FRCOPHTH

The signs and symptoms are suggestive of EBMD in the left eye. The intermittent pain on waking is suggestive of recurrent erosion. Figure 3 shows a map-dot pattern of irregularity affecting the cornea and associated haze. Topography shows irregularity of the central cornea in keeping with this diagnosis.
No photograph of the anterior segment of the right eye and no further history are provided. UCVA is poor with minimal improvement on refraction. What is promising is that the pinhole acuity indicates good visual potential in this eye.
In terms of optimizing the vision in the right eye, it would be useful to know the history of the scar (eg, EBMD, herpetic or other infection). Corneal OCT imaging to look at the depth of the scar would help to determine the treatment options. As always, the treatment offered should start with the least invasive and end with the most. UCVA in the left eye is excellent, and the scar in the right eye is long-standing, indicating that this patient has been coping well to date. These circumstances suggest that one option is not to treat the right eye for the time being.
If the patient is keen for visual improvement, then the first step is a contact lens trial. Sometimes, a contact lens alone can counteract the effect of a corneal scar. If this form of treatment fails, surgical intervention is indicated, either PTK with adjunctive mitomycin C 0.02% or the more invasive deep anterior lamellar keratoplasty. The decision between the two procedures depends on the depth of the scar. The recovery period after deep anterior lamellar keratoplasty is long, and the patient must be counseled appropriately. If the scar is herpetic in origin, this complicates matters; it increases the chance of recurrence, and oral antivirals will be required as prophylaxis. The presence or absence of associated new vessel formation will also help steer the conversation in terms of prognosis and the likelihood of a good outcome.
Visual acuity in the left eye is excellent. Initial management should be noninvasive. I would advise the patient to administer preservative-free lubricating drops during the day and a lubricating ointment at night. Additional supportive measures such as punctal plugs and oral flaxseed oil can be considered if elements of dry eye disease are present. Treatment may reduce symptoms and keep the patient comfortable.
An issue here is that the left eye is the patient’s better-seeing eye, which must be borne in mind if one is considering surgical intervention. If lubricating drops and ointment do not help, then the next step is PTK as opposed to epithelial debridement on its own or anterior stromal puncture. PTK in this context is minimally invasive, very safe, and highly effective for managing the irregularities caused by EBMD and treating recurrent erosion. Given the presence of haze, I would combine the treatment with mitomycin C 0.02%.
Epithelial mapping for both eyes would be useful for diagnostic purposes and could provide useful information for surgical planning.
WHAT I DID: ALLON BARSAM, MD, FRCOPHTH

I performed excimer laser PTK on the patient’s left eye with the Amaris 1050RS laser (Schwind eye-tech-solutions) to treat the symptoms of recurrent corneal erosion syndrome, which had not responded to conservative therapy alone. I performed alcohol debridement followed by a 7-µm PTK ablation. After healing had been confirmed in the left eye, I addressed the poor visual acuity in the right, which was irregular from old scarring that was deep and extended into the stroma. The epithelium was clinically normal in the right eye, so I performed topography-guided transepithelial PRK, again using the Amaris 1050RS laser.
Six weeks after surgery, UCVA in the left eye had returned to preoperative levels, and symptoms had resolved. UCVA was 20/40 OD, which improved to 20/30 with refraction.




