By all measures, Center For Sight, my practice in Sarasota, Florida, has been incredibly successful. Prior to the COVID-19 pandemic, we were in a routine—a good routine but a routine nonetheless. We were practicing high-quality refractive surgery and refractive laser cataract surgery, and we were improving people’s lives. Why change anything?
In March, during the unprecedented worldwide COVID-19 pandemic, an executive order from the governor stopped all elective procedures in Florida, effectively shutting us down. We suddenly had a lot of time to think about changes that would be required to reopen. We knew that our patients would be at substantial risk without a vaccine or effective treatment for some time. It was clear that we would have to do a lot of things differently, possibly forever.
So we started to look critically at and question everything. We asked ourselves, “What could be better?” We looked at consultation times, which sometimes kept patients in our office for 2 hours, from signing in to tech examinations, testing, biometry, the doctor’s examination, waiting rooms, and dilating rooms to patient education, consents, and so on.
Then we started to get excited about how we could make changes to keep our patients safer, improve flow through the office, save patients valuable time, and ultimately allow us to see more patients more efficiently. This article describes some of the changes we have made as a result of our review, the reasons for the changes, and the effects we expect these changes to have on our patients and our practice.
SAFETY
It became clear that, to reopen, we would need to restructure the clinic so that we could keep our patients safe. Most, based on age alone, are in the highest-risk group for COVID-19–related complications. It is our responsibility to provide for their safety while they are in our offices.
Social distancing meant an end to many of the protocols we used to take for granted. We transitioned to greeting people at the door with the screening questions promulgated by the Centers for Disease Control and Prevention, and we did away with waiting rooms and reception areas. Our entire team and all patients are required to wear masks at all times. Face shields on slit lamps have become de rigueur.
We installed thermal imaging systems to monitor everyone’s temperature (Figure 1) discreetly. The system has a programmable temperature that triggers an alarm. It is capable of tracking multiple targets simultaneously and is similar to the systems used in airports.
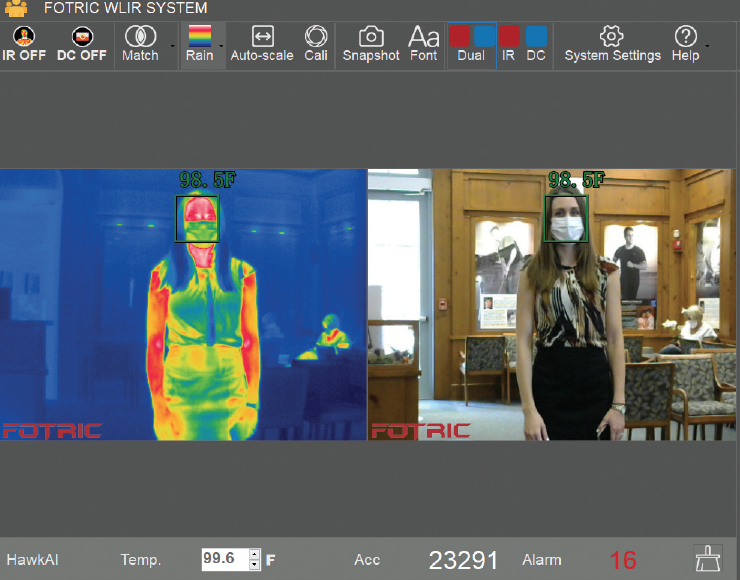
Figure 1. The thermal imaging system is capable of tracking multiple targets discreetly and simultaneously.
Companions and family members are now discouraged from entering the building, except when a patient requires assistance. Although this could make counseling more difficult, we realize that we could do the counseling remotely via telephone or Zoom videoconferencing in order to include spouses or other family representatives.
ZERO-CONTACT INTAKE
With only a few chairs left in our reception area, we needed a technology to allow patients to wait in their cars until the technician was ready to bring them back to a room. For this, we use Phreesia, a software-as-a-service app, designed to facilitate an efficient, no-contact patient intake system.
The system allows preregistration by patients so that when they arrive there are no forms to fill out (eg, insurance, HIPAA, consent)—these have all been completed electronically before arrival, including demographic data (Figure 2). The system populates this information directly into our Nextech/MDI electronic medical record system.
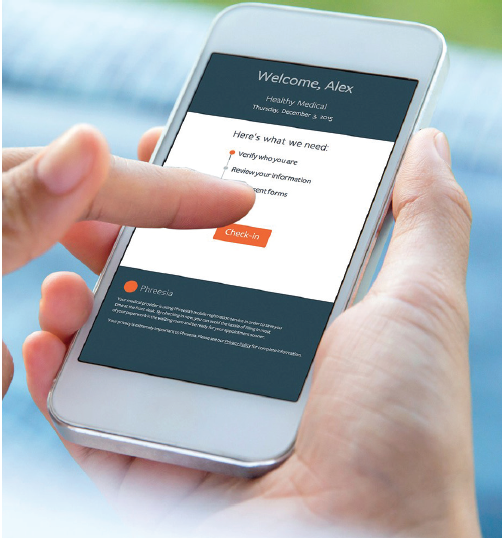
Figure 2. Phreesia is used by patients to complete paperwork and check in for their appointment.
Finally gone are the days when patients would take up to 20 minutes completing paperwork upon arrival, all the while touching pens and papers, potentially surrounded by strangers. This created problems with efficiency, limited our ability to stay on schedule, and involved multiple touchpoints.
Our adoption of Phreesia has the dual benefit of increasing patient safety and improving our efficiency. I believe that this system will ultimately allow us to schedule more patients more efficiently and waste less of their valuable time.
The system registers when patients arrive in the parking lot, allowing us to two-way text them to acknowledge their arrival, and it reminds them to wait in their vehicle until a tech is ready for them. On the back end, Phreesia is also capable of handling payment and merchant processing, consents, and even surveys, all with zero contact and paperless. We are still in the process of integrating this system, but we are impressed with it so far.
MINIMAL CONTACT Examinations
Once the system notifies patients that a technician is waiting, they come in, respond to screening questionnaires and thermography, and are brought straight back to their own dedicated exam lane. Patients bypass the reception room and other common areas. They leave their dedicated room only when the technician whisks them to the testing area where topography, OCT, and other tests are done. They then return quickly back to their lane.
When the technician completes the workup, I am notified immediately via the Slack communicator app, which allows WiFi-based messaging across all phone platforms. I see patients in the same room with the same technician, who now functions as a scribe and then as a procedure counselor after I leave.
Patients are then taken directly to the door to exit the practice. All surgical counseling is done remotely via telephone or videoconferencing. Billing and payments can be done automatically with Phreesia or via telephone after the visit, again with the aims of expediting the encounter and reducing contact.
We used to have patients worked up initially in one room, then moved to a waiting area for testing, then wait again to be worked up further in another exam lane, then wait in the dilating room, then finally be brought back to one of my exam lanes where I would see them with a scribe. Now, we have fewer people in contact with each patient and no handoffs. By eliminating handoffs, we achieve a definite improvement in efficiency. By eliminating waiting rooms and common areas, we give the patient the comfort and security of a private lane.
Watch It Now
Dr. Lahners outlines his practice’s cautious approach to reopening and shares the practice’s new operational protocols to ensure patient safety.
NONCONTACT IMAGING
Sitting in a dilating room requires a handoff and more inefficiency. It also requires social distancing, dramatically reducing the number of chairs available. Plus, indirect ophthalmoscopy requires prolonged face-to-face time and contact with the patient’s lids and face. How would we deal with this?
We invested in optomap ultrawide-field retinal imaging (Optos), a noncontact, nonmydriatic posterior pole imaging system. Although we cannot eliminate pupillary dilation for all patients, some patients on the surgical consultant’s schedule have options. For example, if a patient has recently been seen by one of our optometrists and has a well-documented normal retinal examination and no new vitreoretinal symptoms, we now offer a mini-dilation with 2.5% phenylephrine (no tropicamide) combined with optomap imaging. This quickly gives the patient a big enough pupil for evaluation in most cases.
Most patients I see are surgical referrals from one of our optometrists, and most times they had a thorough retinal examination in recent days or weeks. The optomap has been an excellent tool for these patients; it offers a streamlined examination process, avoids the side effects associated with cycloplegia, and eliminates time spent in the dilating room. Pupils dilate only partially with phenylephrine, so patients do not become as light-sensitive as with full dilation, do not lose their reading capability, and recover faster after the eye examination.
We cannot offer this option to new patients or those with pseudoexfoliation, a history of trauma, or zonular loss, for example, because full dilation is necessary in these cases for a proper surgical evaluation. The optomap is a nice option, however, for routine patients.
In many cases, the view with this device is as good as or better than what we can see with an indirect ophthalmoscope due to problems with patient cooperation, photophobia, or other factors. It also offers different imaging options. One of my favorites is the red-free image, which is great for evaluating retinal vascular disorders such as diabetes.
Eliminating an extended close face-to-face indirect ophthalmologic examination and avoiding touching the patient’s eyes and lids can help lessen the risk of transmitting contagions in the rare case of an asymptomatic, afebrile doctor or patient.
The optomap images are loaded seamlessly into our electronic medical record system, allowing me to peek at the patient’s retina before even entering the exam lane. This review may call attention to a potential problem, which triggers a full dilation and possibly a retinal consultation. The images provide a high-definition record of the retina for documentation of everything from the nerve to the macula and even the peripheral retina. It has been a nice addition to our practice and has greatly helped increase efficiency and decrease contact.
CONCLUSION
We are getting better all the time and are constantly learning from our colleagues how to navigate this new landscape. By questioning every step in our process, we have achieved our goals of increased patient and staff safety, increased efficiency, and an overall improvement in patient care, ultimately allowing us to increase our productivity.
We are happy to be back in operation now (Figure 3). We are taking everything one day at a time and nothing for granted and enjoying Center For Sight 2.0.

Figure 3. Dr. Lahners performs surgery with heightened safety protocols.