CASE PRESENTATION
A 27-year-old woman is referred for cataract surgery. The patient reports increased light sensitivity, glare, and a slight reduction in her visual acuity.
Her BSCVA is +0.25 -0.75 x 115º = 0.8 OD and +0.50 -1.50 x 85º = 0.5 OS. A clinical evaluation finds normal corneas, retinas, and optic nerves. A slit-lamp examination in mydriasis shows nuclear lens opacification that is greater in the left eye (Figure 1). OCT imaging (ACE, Bausch + Lomb) confirms the presence of a nuclear cataract (Figure 2). Imaging with the Pentacam AXL (Oculus; Figure 3) shows a regular cornea with 0.50 and 1.00 D of corneal total astigmatism in the right and left eyes, respectively.
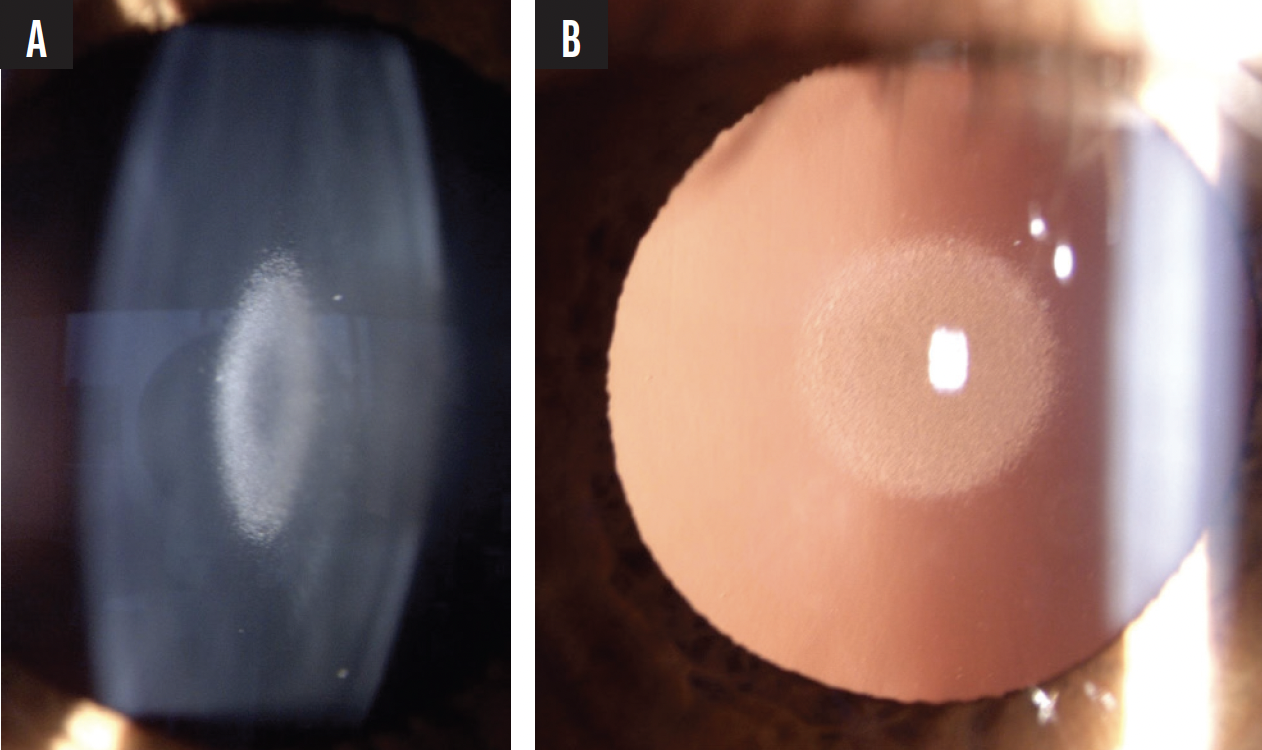
Figure 1. Nuclear cataract in the right eye viewed at the slit lamp (A) and with retroillumination (B).
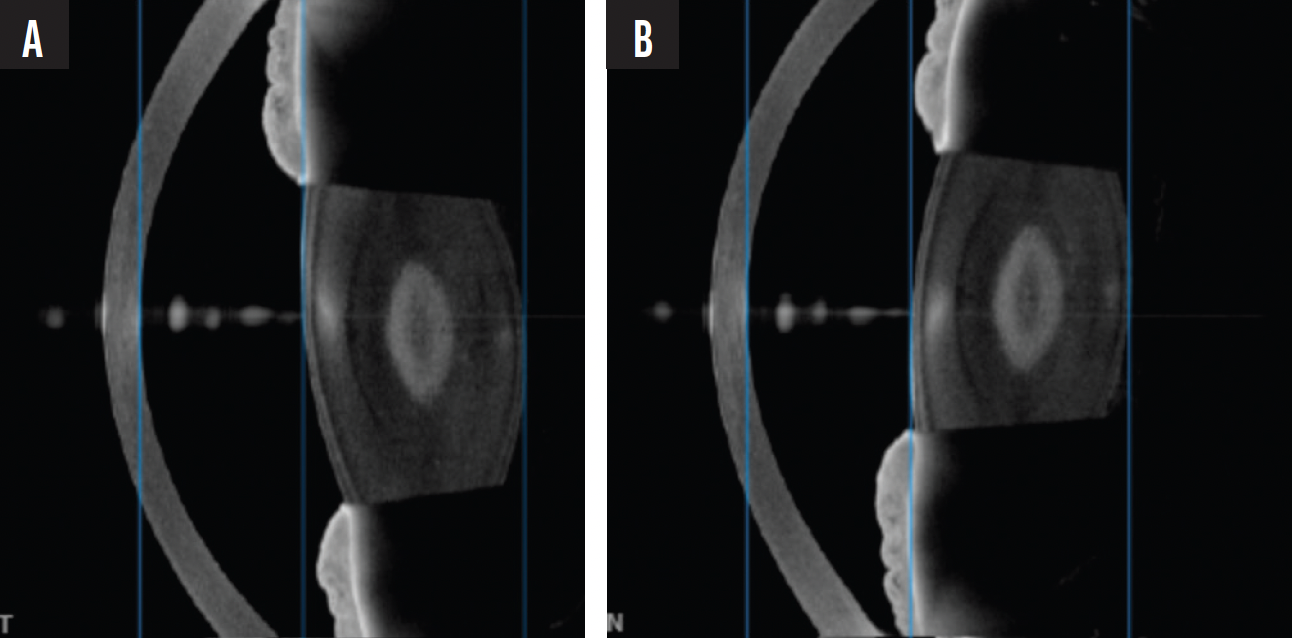
Figure 2. OCT imaging confirms the presence of a nuclear cataract.

Figure 3. Tomography shows a regular cornea and a grade of 1 in each eye using the Pentacam Nucleus Staging Module.
The patient’s daily activities include horseback riding, driving, working at a computer for 4 hours, and reading. She desires maximum spectacle independence.
How would you proceed?
—Case prepared by Suphi Taneri, MD, FEBOS-CR


BASAK BOSTANCI, MD, FEBO, AND SEFIK CAN IPEK, MD, FEBO
When counseling a young patient with bilateral cataracts, it is essential to consider that the condition may be congenital, which could predispose them to amblyopia. The cataract shown in Figure 1 resembles a central pulverulent cataract, a term that refers to powdery disc-like opacities involving the embryonal and fetal nucleus. It is well known that amblyopic eyes perform poorly in low-contrast environments, so the reduction in contrast sensitivity associated with the implantation of a multifocal IOL could be problematic. The large angle kappa shown on Pentacam imaging would make us even more hesitant to implant a multifocal lens. Additionally, based on the increased posterior corneal densitometry measurements with the Pentacam, we would order a specular microscopy exam to evaluate the endothelium.
A review of the patient’s daily activities indicates that, apart from reading, she spends most of her time on activities that require distance and intermediate vision. Based on this and the aforementioned factors, our preference would be to implant an extended depth of focus (EDOF) IOL in each eye with a target of emmetropia. Surgery would be performed on the left eye first, and the patient’s visual acuity and accommodative capacity with both eyes working together would be evaluated before operating on the right eye. Care would be taken to avoid fixation switch diplopia, which can occur in patients who have a history of amblyopia; a change in refractive status causes the amblyopic eye to become the fixating dominant eye.
Because the situation has a genetic etiology, it might be beneficial to examine the patient’s family members.

WILLIAM F. WILEY, MD
This presentation is unusual but not unheard of in a 27-year-old patient. The unique appearance of the cataract has been beautifully captured with OCT imaging and at the slit lamp. The opacity may be a lamellar cataract affecting the fetal nucleus and thus could be a form of congenital cataract that has progressed to clinical significance. If so, it may have a genetic etiology, likely with an autosomal dominant inheritance pattern.
Given the patient’s age and lifestyle demands, a careful approach is essential to ensuring optimal visual outcomes and her satisfaction. A detailed discussion with the patient is necessary to identify her visual priorities and emphasize the importance of balancing her distance, intermediate, and near visual acuity against potential optical side effects.
The main decision in this case is which premium IOL to use. A high-quality EDOF lens would offer some depth of focus with minimal photic phenomena, whereas a multifocal IOL would provide a full range of vision but carries a higher risk of nighttime halos and glare.
Delayed sequential bilateral cataract surgery would be my preference, and I would consider implanting a different type of lens in each eye. For instance, placing a full-range trifocal IOL in the first eye would allow the patient to experience its benefits. If she is satisfied with the lens in all environments, the same approach would be employed in the second eye. If, however, the patient is bothered by glare or halos, an EDOF lens would be implanted in the second eye. This strategy could be reversed, with an EDOF IOL placed in the first eye and, if she desires more near vision, a trifocal IOL placed in the second eye. The decision on which lens type to implant and which eye to operate on first depends on her ocular dominance and primary desire (depth of focus vs avoidance of dysphotopsias).
Regarding astigmatism correction, a toric lens is warranted in the left eye. For an accurate determination of total corneal astigmatism, advanced technologies and techniques such as the IOLMaster 700 with Total Keratometry (Carl Zeiss Meditec), a Pentacam assessment of corneal power, use of the Barrett toric calculator, and/or intraoperative aberrometry would be employed. A postoperative evaluation of the residual astigmatism in the patient’s left eye would guide my decision on whether her right eye also requires a toric IOL. Given the borderline amount of astigmatism and her age, I lean toward recommending toric IOLs for both eyes. This approach would be prudent because she is likely to develop against-the-rule astigmatism as she ages, which would flip the axis slightly and potentially render residual with-the-rule astigmatism beneficial in the long run.

WHAT I DID: SUPHI TANERI, MD, FEBOS-CR
The young age of the patient made planning cataract surgery tricky. Not intervening was not an option, however, because increasing glare and light sensitivity were greatly affecting her life. Her history allowed me to rule out amblyopia; both eyes had seen equally well without any dysphotopsias until recently.
Given the patient’s life expectancy, a hydrophobic lens material was my preference to avoid the possibilities of glistenings and opacification in the long term. During our discussions of different IOL designs, I explained to the patient that a monofocal lens would provide her with the best image quality but that she would become dependent on near glasses after surgery. In my experience, this dependence generally frustrates individuals her age who are used to excellent uncorrected near visual acuity. I also noted that multifocal IOLs are associated with reduced vision quality and contrast sensitivity. Further, I explained that a toric model would be required in at least one of her eyes and that complications could arise if the lens rotated after implantation.
The patient elected to receive two IOLs per eye, a primary monofocal lens (RayOne Aspheric IOL, Rayner) placed in the capsular bag and a secondary multifocal lens (Sulcoflex Aspheric Pseudophakic Supplementary IOL, Rayner) implanted in the sulcus during the same session. The refractive target for the monofocal IOL in each eye was emmetropia. The multifocal IOLs had add powers of +1.75 D and +3.50 D to enhance her intermediate and near visual acuity, respectively (Figure 4). An EDOF model of the Sulcoflex lens with a +1.75 D add is also available. In situations like this one, however, I have found that patients dearly miss their crisp uncorrected near visual acuity.
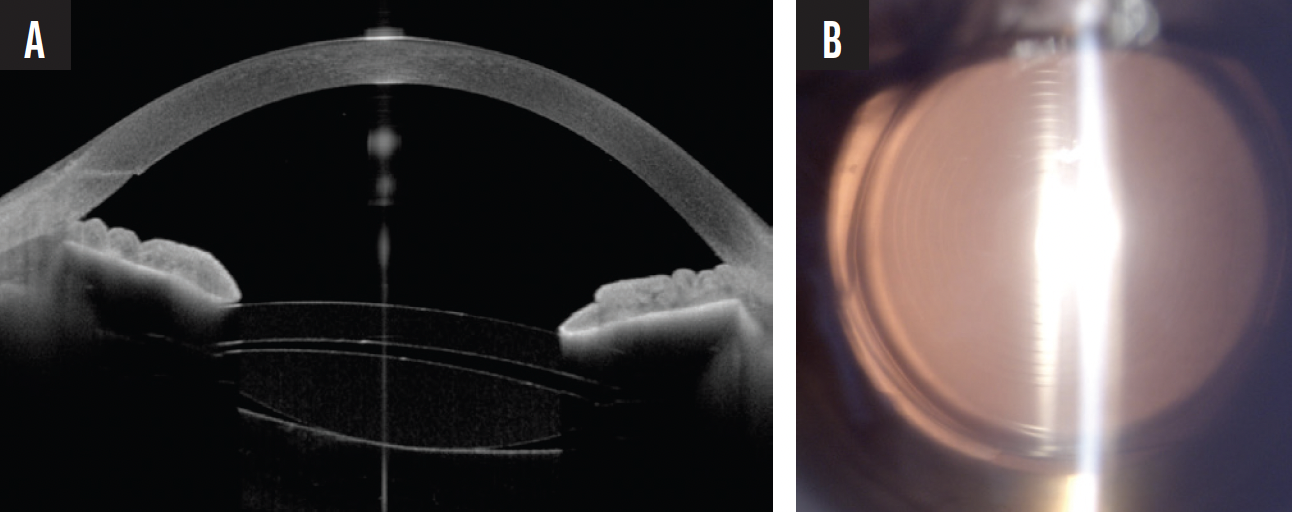
Figure 4. An OCT scan of the lens system—a monofocal IOL in the capsular bag and a multifocal IOL in the sulcus—obtained 3 months after surgery (A). Retroillumination of the multifocal IOL on the day of surgery (B).
The advantage of the dual lens system is that the sulcus-fixated IOL can be removed with relative ease and minimal risk if the patient cannot adapt to the multifocal optic. In my experience, the same is true—even decades after cataract surgery—if their refraction or visual needs change or they develop macular disease.
A few days after surgery, the patient was happy with the outcome. Changes in her refraction are to be expected over the course of her lifetime. These could be addressed by replacing the sulcus-fixated lens because this model is available with a spherical base power of -3.00 to +3.00 D and up to several diopters of toricity.




