
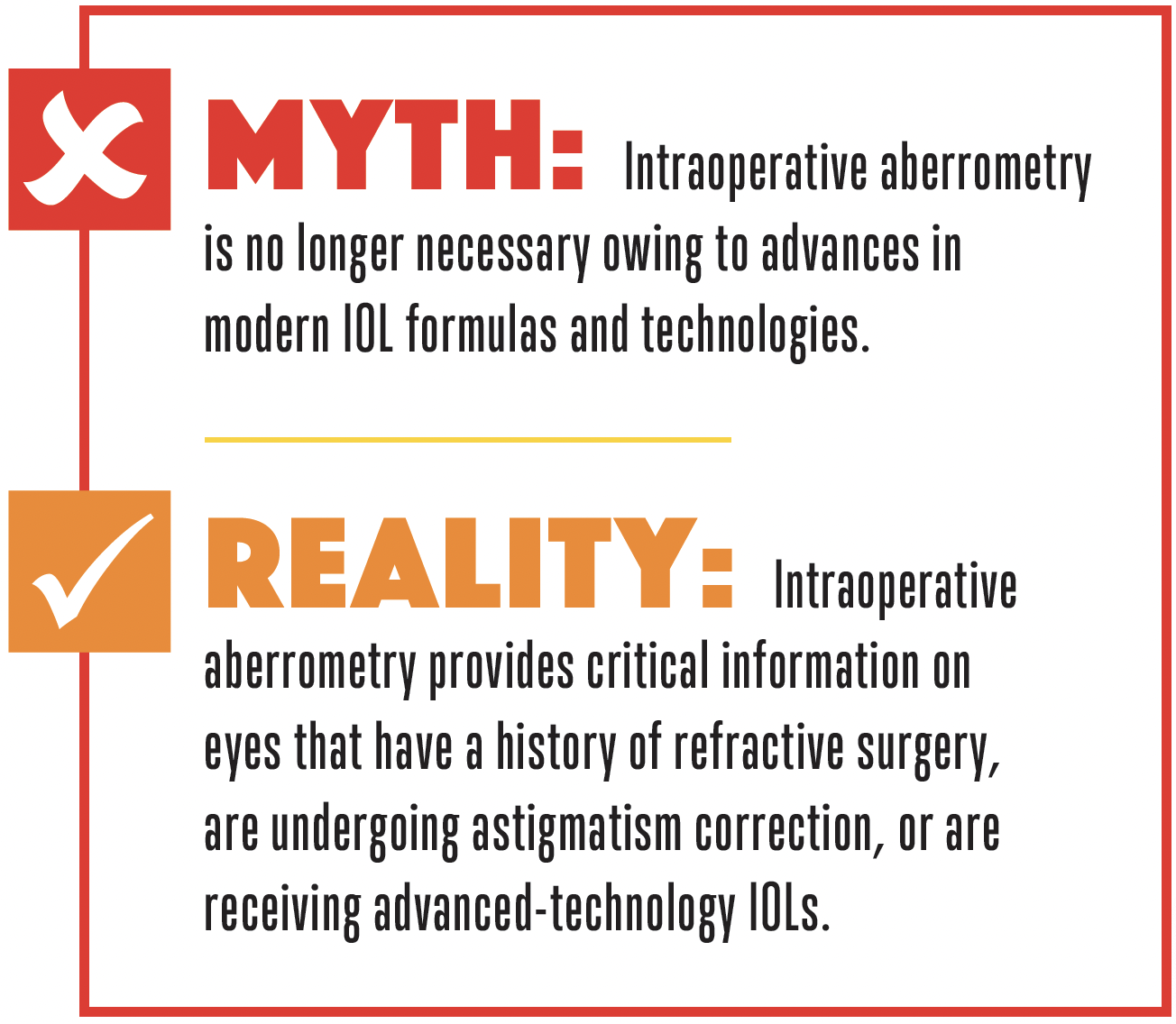
There is a growing belief that intraoperative aberrometry (IA) has lost its relevance in the age of advanced IOL formulas and improved refractive technologies. This misconception deserves correction. Although modern advances have undoubtedly improved outcomes, IA remains extremely valuable.
AREAS WHERE IA SHINES
IOL Power Calculations
Contemporary IOL power formulas such as the Barrett Universal II have revolutionized cataract surgery by enhancing refractive accuracy. These formulas reduce the need for intraoperative IA in many straightforward cases. To say that this makes IA obsolete, however, is incorrect. Particularly in complex cases, IA offers benefits that modern formulas cannot replace.
One of the most valuable uses of IA is in eyes that have a history of refractive surgery. In these cases, measuring true corneal power is a challenge that post–refractive surgery formulas attempt to address. None of them, however, is perfect. In contrast, IA directly assesses the total corneal refractive power, which can greatly improve refractive accuracy.
The introduction of the Light Adjustable Lens (LAL; RxSight) led some practitioners to conclude that IA is no longer necessary. The power of the LAL can be adjusted postoperatively, which might seem to negate the need for precise preoperative measurements. IA, however, helps optimize the initial power, especially when the target is slight hyperopia to induce spherical aberration and improve depth of focus. This lays the foundation for maximizing the LAL’s potential once postoperative adjustments are made.
Astigmatism Management
Current methods for estimating the amount of anterior and posterior astigmatism are imprecise. IA measures the amount and axis of astigmatism after cataract incisions are made, allowing for a more accurate determination of the impact of surgically induced astigmatism and improving refractive outcomes with toric IOLs.
IA REMAINS A VALUABLE TOOL
The belief that IA no longer holds value is a myth. Although the latest IOL formulas and technologies such as the LAL have reduced the need for IA in routine cases, its importance in complex situations remains undeniable. Eyes with astigmatism or a history of refractive surgery are just two situations where IA can be highly beneficial. This technology provides critical information for IOL decision-making that other tools struggle to match, helping cataract surgeons deliver the best possible outcomes to their patients.




