CASE PRESENTATION
A 43-year-old man presents for a cataract evaluation. The patient’s right eye was injured by a dart gun when he was 9 years old. He states that vision in the eye has decreased during the past 5 years. His UCVA is 20/400 OD, and he has a manifest refraction of -4.00 +8.00 x 105º = 20/100 OD. The patient’s BCVA is 20/20 OS with a manifest refraction of -1.75 D.
An examination of the right eye finds a curvilinear corneal scar from the 11 to 3 clock positions and peripheral synechiae from the 1:30 to 3 clock positions (Figures 1 and 2). A 2+ to 3+ anterior subcapsular cataract that is densest nasally is encroaching on the visual axis. There is also a mild nuclear sclerotic cataract and a 1+ posterior subcapsular cataract (Figure 3).
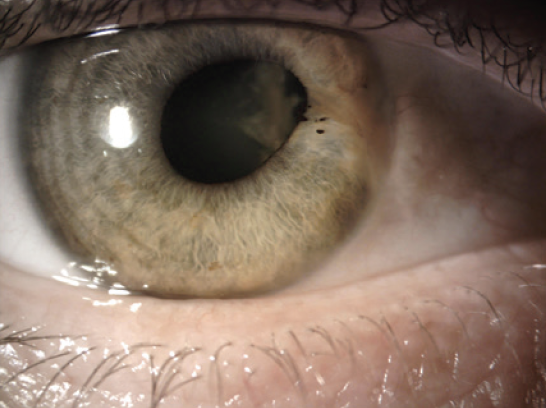
Figure 1. An area of synechiae and zonular dialysis.
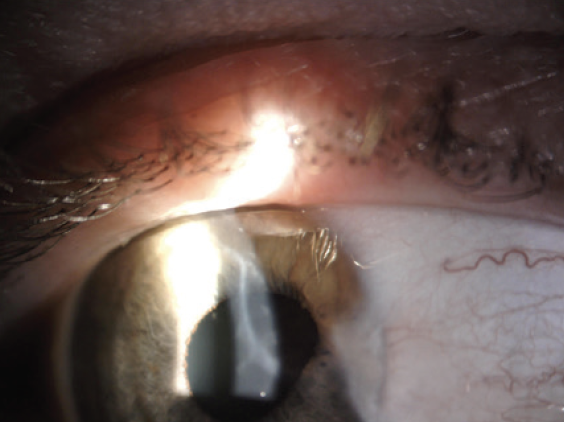
Figure 2. A corneal scar.
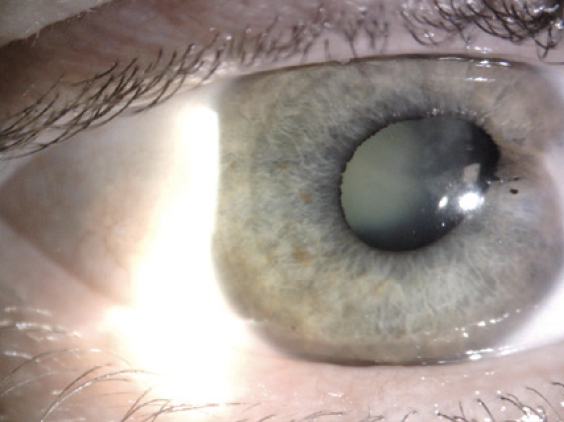
Figure 3. A traumatic cataract.
An evaluation with the Pentacam (Oculus Optikgeräte; Figure 4) finds mostly regular astigmatism with an axis of 106º. The findings of a dilated funduscopic examination are normal. The IOP is 15 mm Hg OD. IOP-lowering medication has not been prescribed.
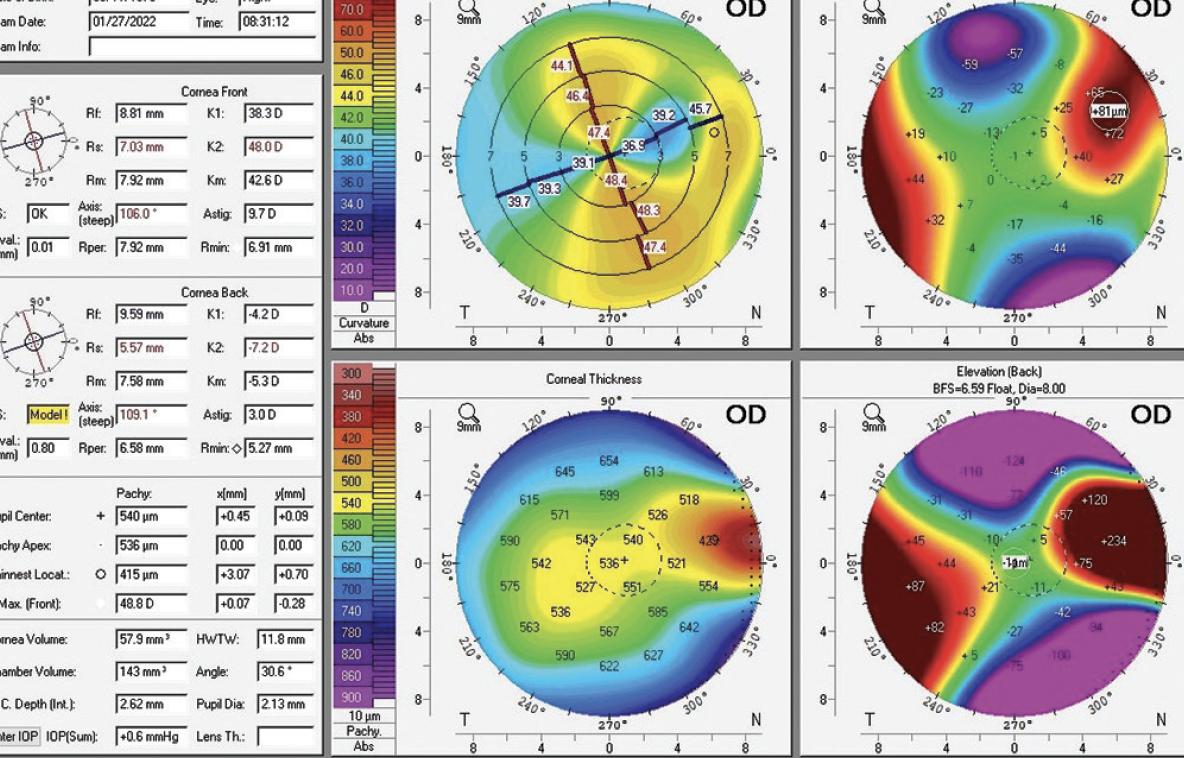
Figure 4. Scheimpflug tomography of the cornea shows astigmatism.
The patient desires the best distance visual acuity possible. How would you proceed? Would you consider a toric IOL? How else might you address the astigmatism? What options would you offer to the patient?
—Case prepared by Audrey R. Talley Rostov, MD

SUMITRA S. KHANDELWAL, MD
I typically would not recommend a toric monofocal IOL for a patient with a corneal scar. The patient’s topography, however, shows regular astigmatism except in the far periphery. I would like more information on his history of glasses wear. Did he have better vision with spectacles in the past? If so, offering to correct some of his astigmatism makes sense. Otherwise, I would consider performing a scleral contact lens overrefraction to confirm that much of his vision loss is not from astigmatism. The refraction matches the topography, so it would make sense if the patient’s vision loss is caused by the cataract. A toric IOL is an option because the cylinder is regular, albeit high.
There are limits to the amount of astigmatism that can be corrected with any of the toric IOLs available in the United States, where I practice. The patient may be happy with some residual with-the-rule astigmatism. He is young, so he may develop against-the-rule astigmatism as he ages. The highest toric power available in this country treats about 4.00 D of astigmatism at the corneal plane, which would leave 4.00 D of astigmatism. Operating on the axis (ie, creating the wound at 106º) would be reasonable, but it would require operating from a superior position, which I often do when necessary.
Residual astigmatism could be corrected with corneal refractive surgery. I would favor PRK over LASIK because of the scarring. With most laser platforms, treatment would have to be customized based on the refraction. Topography-guided PRK might be an option, but the treatment plan might differ because the residual rather than the topographic astigmatism would be treated.
Based on my experience, the iDesign Advanced WaveScan Studio System (Johnson & Johnson Vision) would be able to capture some of the patient’s refraction, but I would be inclined to perform a standard treatment based on the refraction. I would assess the postoperative refraction on two different dates.
Corneal refractive surgery can be performed if the patient desires additional astigmatism correction or if a toric IOL cannot be placed at the time of cataract surgery. Most excimer laser platforms can treat a maximum of 3.00 D of astigmatism, but newer designs can treat a greater amount if the astigmatism is mixed versus myopic in nature.
This combined approach should facilitate treatment of the patient’s refractive error, provided he is a candidate for PRK. Careful counseling to set reasonable expectations is important because it may be difficult to place a toric IOL if the integrity of the capsule has been compromised.

TOBIAS H. NEUHANN, MD, FEBOS-CR
Every traumatic cataract has its own history and therefore its own distinct anatomic features. In the current situation, I cannot know with certainty what to expect intraoperatively, so I would recommend laser cataract surgery for two reasons. First, the appearance of the endothelium is abnormal, and the cell count is significantly reduced. Second, the zonules are likely to be weak in the area of the synechiae. Synechiae sometimes assume the role of the zonules, and the full extent of the subluxation may become clear only if the synechiae are detached.
The question is which IOL to implant. The patient desires the best possible distance vision, so I would discuss two options with him. The first is a custom premium toric IOL. It would have to be perfectly aligned. I would favor an AT Torbi IOL (Carl Zeiss Meditec) because it is unlikely to rotate postoperatively.1 A capsular tension ring (CTR) would be inserted before IOL implantation to prevent uneven shrinkage of the capsular bag, which can cause late rotation of an IOL.
The second option I would discuss with the patient in case the first strategy proves inappropriate or unviable intraoperatively is the implantation of an IC-8 IOL (AcuFocus). This lens can correct some of his astigmatism and much of his ametropia as well as the possible dysphotopsia caused by the corneal scar. Once refractive stability is achieved—probably 3 months after surgery—a manual refraction would be performed to determine the residual refractive error. If the patient cannot or does not wish to wear spectacles or contact lenses, a custom secondary or piggyback IOL can be implanted.
An advantage of the two-stepped approach is that the patient decides whether to have a refraction of -1.75 D, as in the left eye, or maximum distance vision with monovision. The target refraction will likely be achieved because the subjective refraction influences the add-on or supplementary IOL calculation.

ZEBA A. SYED, MD
I would ask the patient about his best corrected visual acuity in the right eye before a cataract developed to help determine the visual impact of the corneal scar. If he has excellent visual potential and is highly motivated to minimize or eliminate his dependence on spectacles after cataract surgery, I would consider implanting a toric IOL to reduce his astigmatism.
The situation described in the case presentation is unusual in that the patient has somewhat regular corneal astigmatism despite the presence of a traumatic scar. I would explain to him that the toric IOLs currently available in the United States, where I practice, cannot eliminate his corneal astigmatism but can debulk it to a reasonable degree. It is critical to ensure that the axis of corneal astigmatism measured with biometry matches the axis measured with the Pentacam. I would take posterior astigmatism into consideration when performing biometry to determine the final magnitude of correction required.
After the implantation of a toric IOL, the patient’s residual cylinder can be corrected with either spectacles or refractive surgery. If he chooses the latter, limbal relaxing incisions and astigmatic keratotomy are options. He should again be counseled that the astigmatism likely can be reduce—but not eliminated—which may decrease his dependence on spectacles.
Zonular dialysis is another surgical consideration. In the absence of capsular support, the toric IOL may rotate in the capsular bag. I would inform the patient of this risk. I would also consider placing a CTR at the time of cataract surgery to reduce the risk of postoperative IOL rotation.

WHAT I DID: AUDREY R. TALLEY ROSTOV, MD
When planning surgery, I wanted to be prepared for different possible scenarios. I therefore had on hand an intrascleral fixation kit (MicroSurgical Technology), a CTR, trypan blue dye, and an additional OVD, all of which could be opened at a moment’s notice.
Laser cataract surgery was performed with the Lensar Laser System (Lensar) under a peribulbar block. A customized capsulotomy was centered on the capsular bag. The option of a customized capsulotomy was selected, and its toric nubs were aligned with the axis of astigmatism. Laser arcuate incisions were created at an optical zone of 8 mm.
Two biaxial incisions were created with a diamond blade, and Viscoat (Alcon) was injected. Horizontal microscissors (MicroSurgical Technology) were used to cut the nasal anterior synechiae. Some of the OVD was removed, and trypan blue dye was injected. An additional amount of OVD was injected, and the free-floating capsulotomy was removed with microcapsulotomy forceps. Hydrodelineation was performed carefully. Phacoemulsification was then carefully executed with an additional OVD placed to protect the bag in the area of zonular dialysis.
A CTR was inserted. An enVista Toric IOL (model 575 at the highest cylinder power available; Bausch + Lomb) was implanted and aligned with the toric nubs on the capsulotomy. I selected this IOL because the cornea was irregular and the IOL would add zero spherical aberration if it was slightly decentered after surgery.
The patient has done well postoperatively. He has 2.00 D of residual astigmatism but is happy with his outcome.
1. Lesieur G, Dupeyre P. Toric IOL rotation: hypotheses, mistakes, and opportunity. Cataract & Refractive Surgery Today. February 2022. Accessed March 29, 2022. https://crstoday.com/articles/feb-2022/toric-iol-rotation-hypotheses-mistakes-and-opportunity-2/




