

IOL dislocation during the postoperative period can be visually debilitating for patients, particularly if a significant intraocular event triggers this clinical scenario. Late dislocation of an IOL may present as an isolated event, or it may be associated with subluxation of the entire capsular bag complex.
RISK FACTORS
Zonular weakness and dehiscence can lead to partial or total dislocation of the IOL–capsular bag complex. This weakness may be genetic, as in Marfan syndrome, or acquired, as in blunt trauma and capsular phimosis. Pseudoexfoliation is a major cause of late dislocation of the IOL–capsular bag complex. Other causes include extreme myopia and prior vitrectomy.
In patients who are at increased risk of a dislocated IOL, the placement of a capsular tension ring during cataract and IOL surgery can be helpful. This maneuver often distends the bag, but it is not always successful at preventing IOL dislocation. Adjunctive treatment may therefore be necessary.
An increase in the use of 10-0 and 9-0 polypropylene sutures (Prolene, Ethicon) during the past decade to fixate the capsular bag to the sclera has led to a recent increase in the incidence of dislocation of the IOL–capsular bag complex. This is because these sutures weaken and degrade over time.
The development of capsular phimosis triggers the contraction of the capsular bag. Residual epithelial cells in the capsular bag are thought to induce fibrosis of the bag in a purse-string fashion, which initiates and exerts tractional pull on the zonules. The degree of tractional pull is directly related to the amount of fibrosis induced. This situation can be avoided through early diagnosis because traction can be released by placing small relaxing incisions in the capsular margin.
MANAGEMENT
The management of late IOL dislocation mainly involves stabilizing the IOL–capsular bag complex. An anterior or a posterior approach may be used. An adequate vitrectomy should be performed in all cases because vitreous traction is usually present. The choice of surgical intervention depends on the severity of dislocation.
For Mild to Moderate Subluxation
Repositioning and fixation of the IOL–capsular bag complex to the scleral wall. This can be achieved by passing a 7-0 PTFE suture (Gore-Tex, W.L. Gore & Associates) through the IOL haptic and capsular bag. PTFE sutures do not degrade and have high tensile strength; their placement can stabilize the IOL–capsular bag complex.1
For Severe Subluxation/Dislocation
Explantation of the IOL–capsular bag complex, followed by the intrascleral fixation of a three-piece IOL. When dislocation is severe, explantation may be necessary, after which a replacement IOL is implanted. Two methods can achieve satisfactory outcomes.
No. 1: Glued IOL. In this technique, two partial-thickness scleral flaps are created, and a sclerotomy is made beneath these flaps.2 The haptics of a three-piece foldable IOL are externalized through the sclerotomy site, and they are tucked into a scleral tunnel made with a 26-gauge needle (Figures 1 and 2). The scleral flaps are then sealed with fibrin glue.
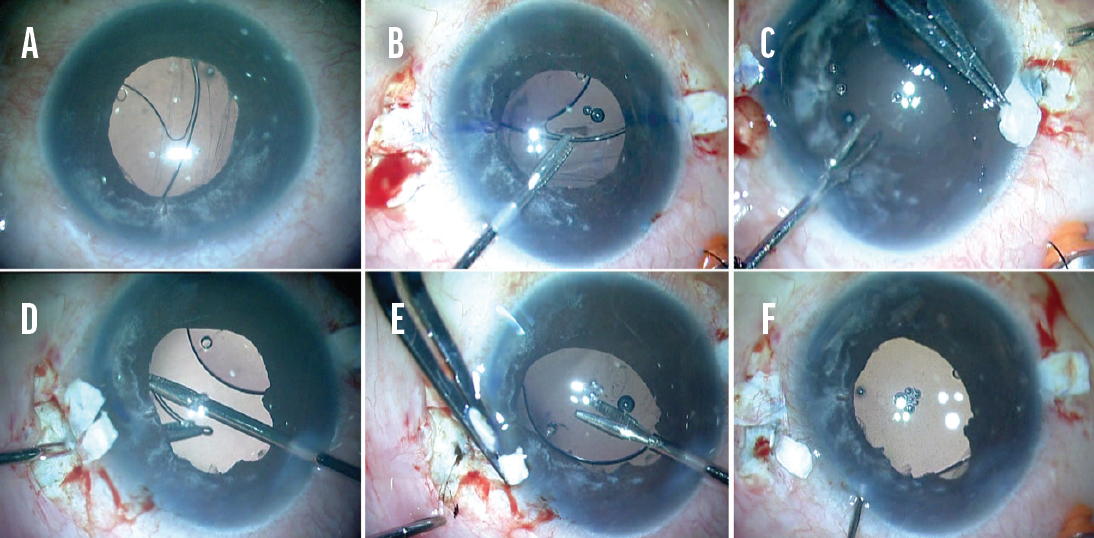
Figure 1. A dislocated one-piece IOL and disrupted vitreous (A). A haptic is grasped (B) and externalized (C). The tip of the haptic is grasped with end-opening forceps (D). The other haptic is externalized (E). The haptics are tucked into scleral pockets, and the flaps are sealed with fibrin glue (F).
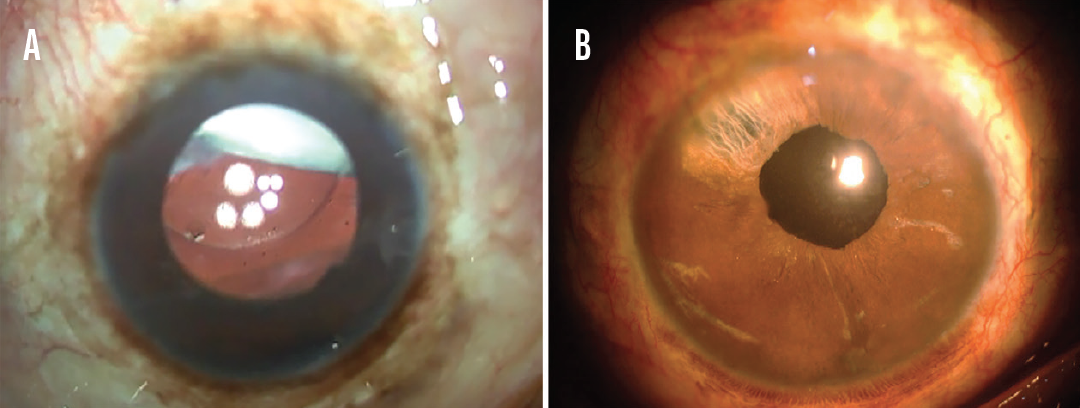
Figure 2. A Soemmering ring is visible in the upper quadrant of an eye with a dislocated IOL (A). The eye after removal of the Soemmering ring, vitrectomy, and glued IOL fixation (B).
No. 2: Double-needle technique described by Yamane et al.3 In this technique, the haptics of a three-piece foldable IOL are threaded into a thin-walled 30-gauge needle. An IOL with PVDF haptics is preferable for Yamane’s method of IOL fixation. The tip of the externalized haptics is reshaped into a flange with low-temperature cautery and tucked into the scleral wall. (For more on this technique, see “Yamane Tips and Tricks”.)
Intrascleral refixation of the existing IOL. If the dislocated IOL is a three-piece design, it may be possible to refixate the lens inside the eye. An advantage of this technique is that manipulation of the IOL occurs in a closed chamber, which minimizes vitreous leakage and avoids postoperative hypotony. Prolonged hypotony has its own set of long-term complications.
Four-flanged fixation of the IOL. In a technique described by Canabrava et al,4 5-0 PTFE sutures are passed through the haptics of a foldable one-piece IOL. Low-temperature cautery is used to create two flanges in the eyelets of the IOL and two flanges outside to insert inside the scleral tunnel and fixate the IOL. (To learn more about Canabrava’s technique, click here to read, “The Best Technologies for Subluxated Cataracts,” from the January issue of CRST.)
SURGICAL PEARLS
The choice of procedure for secondary IOL fixation depends on the surgeon’s preferences and the integrity and status of the ocular anatomy (eg, cornea and iris). The implantation of an anterior chamber IOL should be avoided in an eye with a low endothelial cell count, and an iris fixation procedure should be avoided in an eye with an iris defect.
Postoperatively, patients should be monitored closely for increased IOP and the development of cystoid macular edema.
1. Khan MA, Gupta OP, Smith RG, et al. Scleral fixation of intraocular lenses using Gore-Tex suture: clinical outcomes and safety profile. Br J Ophthalmol. 2016;100(5):638-643.
2. Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S. Fibrin glue–assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34(9):1433-1438.
3. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
4. Canabrava S, Canêdo Domingos Lima AC, Ribeiro G. Four-flanged intrascleral intraocular lens fixation technique: no flaps, no knots, no glue. Cornea. 2020;39(4):527-528.




