
Cataract surgery is a safe and predictable procedure that provides patients with reliable postoperative outcomes and improves both their quality of vision and visual function.1-4 We surgeons sometimes forget, however, that the quality of the postoperative result is directly related to the quality of the preoperative examination.
IT ALL STARTS PREOPERATIVELY
The most common complaints we hear from patients who receive presbyopia-correcting IOLs are the result of one of the following:
- Residual refractive errors (sphere and cylinder);
- Ocular surface/dry eye disease;
- Higher-order aberrations;
- Posterior capsular opacification (PCO);
- Retinal pathology;
- Positive and negative dysphotopsias;
- IOL decentration; and
- Problems with neural adaptation.
The best defenses against unhappiness with presbyopia-correcting IOL technologies are taking time to understand patients’ needs and desires before surgery and executing a perfect preoperative examination. For starters, evaluate patients’ personalities. Are they obsessive or perfectionists? Are they demanding or anxious? Do they have unrealistic expectations? Are they unable to comprehend the information shared with them about the surgery itself or their options? Patients with these traits are generally not the best candidates for presbyopia-correcting IOLs. The availability of more lens designs makes it easier for us to match IOL technologies to patients’ needs.
The next step is to conduct a thorough preoperative examination, including optical biometry; measurements of axial length, lens position and thickness, and anterior chamber depth; keratometry readings with a minimum of two reliable devices; topography and/or tomography; macular OCT to rule out retinal pathology; and dry eye testing. Patients with an epiretinal membrane with retinal thickening or macular drusen, for example, do not fare well with diffractive IOL technologies. Likewise, patients with signs of ocular surface disease or inflammation often are not good candidates for presbyopia-correcting IOLs until their symptoms are under control.5 Ocular surface optimization also helps to ensure that we can obtain accurate measurements preoperatively.
MY PATIENT IS UNHAPPY, SO NOW WHAT?
Even with careful patient selection and a thorough preoperative evaluation, residual refractive errors can occur, and patients can experience undesirable visual outcomes with presbyopia-correcting IOLs. Perhaps the lens is not perfectly centered postoperatively, PCO develops, or the patient experiences symptoms such as blurry, low-quality vision or halos and glare. Any of these outcomes may require an IOL exchange procedure but not before considering three appropriate management tactics.
Woodward et al6 conducted a retrospective review of patients who were dissatisfied with their visual outcomes with multifocal IOLs. The investigators reported that, after appropriate treatment, only 7% of eyes required an IOL exchange. From that study, I learned that I can effectively manage the majority of unhappy presbyopia-correcting IOL patients by addressing one of the following:
- Dry eye disease;
- Residual refractive error; and
- PCO (Figure).
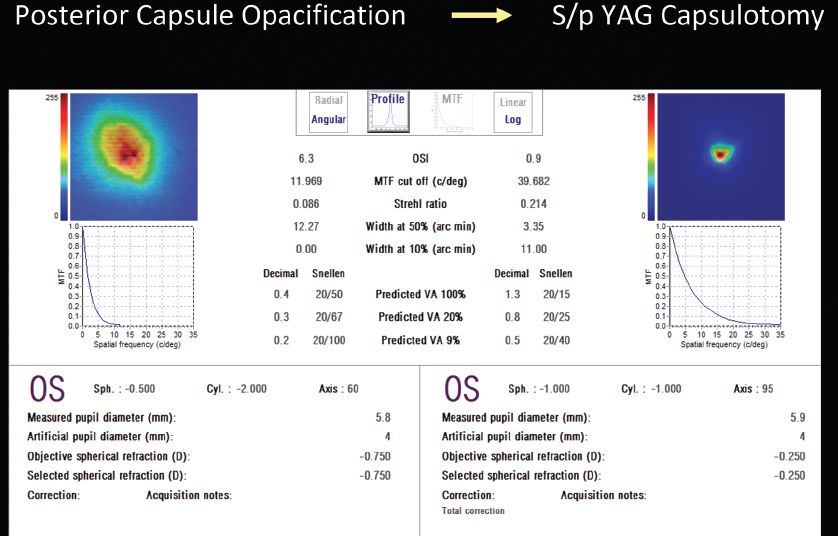
Figure. Laser capsulotomy for PCO.
If employing these three strategies does not resolve the patient’s complaint, then I will explant the IOL. There are several good options for this. One is to exchange the presbyopia-correcting IOL for a standard monofocal, usually in the dominant eye only, to minimize positive dysphotopsias such as halos and glare. Another option is to implant an enhanced monofocal IOL (Tecnis Eyhance, Johnson & Johnson Vision) or a beam-shaping IOL (AcrySof IQ Vivity, Alcon). Visual disturbances such as glare, halos, and starbursts with these lenses are similar to with standard monofocals.
Next-generation nondiffractive extended depth of focus lenses flatten the defocus curve, which increases the tolerance of residual refractive error (ie, defocus). Newer extended depth of focus IOLs may be suitable for certain patients who are deemed poor candidates for multifocal IOLs but who desire adequate intermediate and/or near spectacle independence. Further studies are needed on the pinhole IOL and accommodating and pseudoaccommodating lenses.
In any of these scenarios, I explain to patients that they may give up some of their functional near vision and that they may need readers more often. When I leave the presbyopia-correcting IOL in the patient's nondominant eye, they usually do really well.
CONCLUSION
Successful postoperative outcomes with presbyopia-correcting IOLs start with the preoperative assessment. Conducting a thorough preoperative examination, managing patient expectations, and hitting the postoperative refractive target are all crucial elements of any surgeon’s plan. When an IOL exchange is required, however, I recommend explanting the presbyopia-correcting IOL from the dominant eye only so that the patient retains some spectacle independence.
1. Davis G. The evolution of cataract surgery. Mo Med. 2016;113:58-62.
2. Finger RP, Kupitz DG, Fenwick E, et al. The impact of successful cataract surgery on quality of life, household income and social status in South India. PLoS One. 2012;7:e44268.
3. Lamoureux EL, Fenwick E, Pesudovs K, et al. The impact of cataract surgery on quality of life. Curr Opin Ophthalmol. 2011;22:19-27.
4. Lansingh VC, Carter MJ, Martens M. Global cost-effectiveness of cataract surgery. Ophthalmology. 2007:1670-1678.
5. Gouveal L, Waring GO IV, Brundrett A, Crouse M, Rocha KM. Objective assessment of optical quality in dry eye disease using a double-pass imaging system. Clin Ophthalmol. 2019;13:1991-1996.
6. Woodward MA, Randleman JB, Stulting RD. Dissatisfaction after multifocal intraocular lens implantation. J Cataract Refract Surg. 2009;35(6):992-997.




