
Although, ideally, the IOL remains in place after its implantation, explantation is required in certain situations. This article describes the main factors in my decision to remove an IOL and shares my preferred approach.
RATIONALE
Before proceeding, it is important to be certain that removing the IOL will solve the problem at hand. The main reasons for explanting a monofocal IOL are decentration and opacification of the lens. Problems such as glare, halos, and poor quality of vision are common reasons to consider explanting a presbyopia-correcting IOL. (For more on this topic, see the article, “When to Exchange a Presbyopia-Correcting IOL and What to Put in Its Place.") Residual ametropia from an incorrect power calculation and severe dislocation or tilt of an IOL are additional reasons for potential explantation of both monofocal and presbyopia-correcting IOLs.
I thoroughly evaluate patients who present with problems after cataract surgery to determine whether the IOL should be removed. I take several factors into account when making a decision. For example, many patients with dysphotopsias experience neural adaptation over time. I therefore counsel these patients to wait at least 12 weeks to achieve their true visual potential. At that time, I will reevaluate them, and together we will make a final decision. My explantation rate for multifocal IOLs is low because most of my patients report fewer visual disturbances as time passes.
During a planned explantation surgery, I may find that the lens is slightly dislocated and sitting partially in the sulcus because the haptic was not placed correctly during cataract surgery. This situation can be remedied by repositioning rather than explanting the IOL. Another issue that may cause visual problems is when the capsular bag becomes dislocated after cataract surgery. This can be fixed by placing a capsular tension ring or suturing the bag to the sclera to avoid explanting the IOL.
A FOUR-STEP APPROACH
Once a clear requirement for removing the IOL is established, surgery should occur as soon as possible to avoid severe anterior capsular fibrosis. I typically use a four-step approach.
Step No. 1: Get the IOL into the anterior chamber. My approach can be broken into two main variations. If the posterior capsule is intact, a paracentesis is created, and an attempt is made to loosen adhesions to the lens with a cohesive OVD and a small cannula. The IOL is then slowly moved into the anterior chamber. If the integrity of the posterior capsule has been compromised, a trocar is inserted. Depending on visibility, an anterior vitrectomy is performed. The IOL is then released into the anterior chamber.
Step No. 2: Dissect the IOL. The IOL is cut into two or three strips. For this step, my preference is to use 23-gauge MST Micro-Holding Forceps to stabilize the IOL and 19-gauge Packer/Chang IOL Cutters (both instruments from MicroSurgical Technology) to cut the lens (Figure 1).
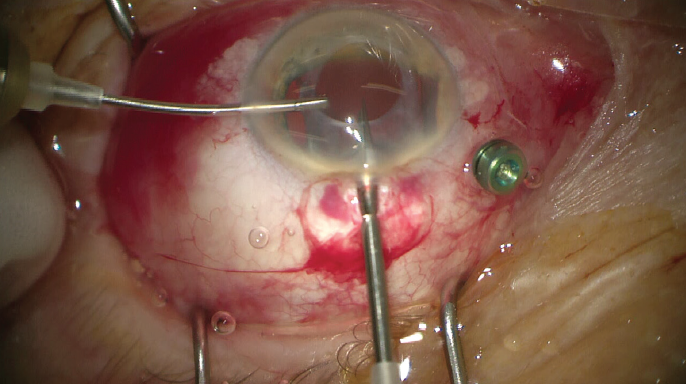
Figure 1. The one-piece IOL is stabilized with 23-gauge forceps while a 19-gauge cutter is used to cut the lens.
Step No. 3: Remove the IOL. The IOL pieces are extracted through a small incision to minimize trauma (Figure 2).
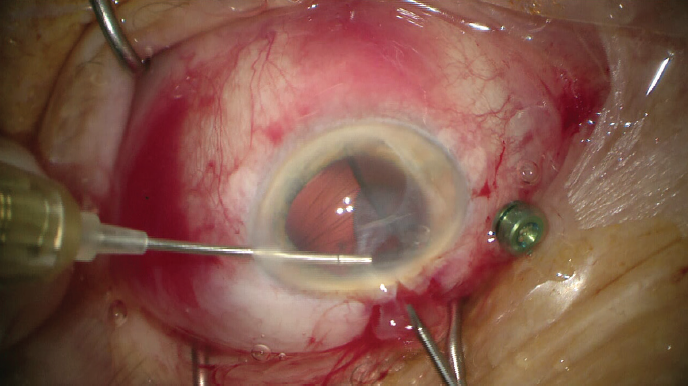
Figure 2. The IOL is explanted in longitudinal slices with 23-gauge forceps.
Step No. 4: Implant a new IOL. Lens selection depends on several factors, including ocular anatomy, the model of the original implant, and the method of its explantation (ie, whether it had to be rotated out of the capsular bag or the IOL and capsular bag had to be explanted). Ideally, the lens selected will fit well into the position vacated by the original IOL.
If the capsular bag equator is intact or partly open, a three-piece IOL is my preference. I will attempt to implant the lens in the bag if the equator is intact. If, however, the adhesions are too strong and the entire capsule cannot be opened, the lens is implanted in the ciliary sulcus. If zonular weakness is evident or suspected, a secondary fixation strategy such as scleral fixation with a suture or the double-needle Yamane technique may be used. The OVD is removed, and the eye is closed. (For more on scleral fixation, see the article, “Yamane Tips and Tricks.")
STRATEGIC PLANNING
After performing more than 100 explantations in 2020, I can say that each case is unique. Therefore, my strategy depends on what occurs intraoperatively. In a recent case, the IOL was loosened, cut into pieces, and explanted. Because the capsule was intact, I decided to implant another one-piece IOL in the bag.
I prepare a detailed surgical plan in advance of every explantation procedure. Preoperatively, I attempt to determine, based on the type of IOL, where the strongest adhesions may be in an effort to anticipate where the lens should be loosened. This helps to ensure that the IOL can be released from the capsular bag into the anterior segment. I also have a backup plan based on the following two questions:
- Am I capable of performing the surgical alternative?
- Are the necessary tools on hand for potential complications?
CONCLUSION
Explantation is not always indicated. When it is, a thorough preoperative assessment is essential to creating a primary surgical plan and a backup option.




