CASE PRESENTATION
An 84-year-old-woman presents with a complaint of fluctuating, blurry vision that she says is more significant in her left eye. She underwent uneventful cataract surgery and the implantation of a monofocal toric IOL in each eye 2 years ago.
The patient has with her a copy of the IOL card for the left eye only, and it shows that she received a 23.50 D Tecnis Toric IOL (model ZCT600, Johnson & Johnson Vision). She says that her vision has never been consistently clear postoperatively.
The patient has mild to moderate open-angle glaucoma in each eye that has been stable for years, and she administers travoprost at bedtime. She reports being diagnosed with mild Fuchs dystrophy and says one specialist recommended that she receive a corneal transplant and an IOL exchange in the left eye followed by the right eye. She has since visited several ophthalmologists to request their opinions.
On examination, the patient’s BCVA is +1.00 -3.00 x 77º = 20/25 OD and +0.75 -2.25 x 100º = 20/40- OS. Keratometry (K) readings are 42.00/48.00 D @180º OD and 42.00/48.25 D @ 2º OS. Trace blepharitis but no occult ocular surface disease (OSD) or corneal staining is evident in each eye. Both eyes have 1+ guttae with no occult corneal edema; endothelial specular microscopy is shown in the Figure.
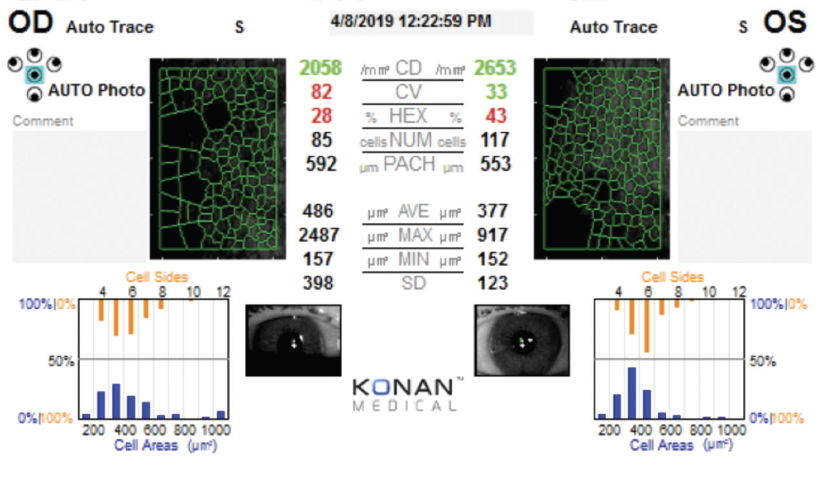
Figure. Endothelial specular microscopy at the initial evaluation.
Ultrasound pachymetry readings are 550 µm OD and 546 µm OS. The toric IOLs are neither decentered nor tilted. Trace to 1+ posterior capsular opacification (PCO) is observed in each eye. The posterior segment examination is significant for cup-to-disc ratios of 0.45 OD and 0.30 OS without evidence of maculopathy.
The patient expresses frustration and confusion and says that she thought she had routine cataract surgery. She wants to avoid further surgery and asks what can be done medically to improve her vision.
How would you proceed?
—Case prepared by Alanna Nattis, DO, FAAO


ARJAN HURA, MD, AND WILLIAM F. WILEY, MD
Managing the patient’s expectations and treating potential causes of loss of BCVA are essential in this situation. Five issues warrant consideration.
No. 1: Glaucoma. What is the patient’s IOP? What is the target IOP? We would obtain visual field tests and OCT scans of the retinal nerve fiber layer for evidence of disease progression. The patient is 84 years old. Is medical therapy with travoprost necessary, and is it contributing to OSD that may be affecting her vision?
No. 2: OSD. Fluctuating vision with known blepharitis could be contributing to OSD. Lissamine green staining may show occult signs of OSD, and the results of meibomian gland expression might be revealing. Does the patient find that her vision is worse during certain activities?
No. 3: Fuchs dystrophy. The pachymetry readings are normal and the corneas free of edema. The patient may be, however, experiencing subclinical symptoms. Does she find that her vision is worse in the morning?
No. 4: PCO. Is the PCO central and potentially visually significant?
No. 5: IOL position. The toric IOLs are neither decentered nor tilted, but have they rotated? The axes of astigmatism differ between the manifest refraction and K readings. The patient has 6.00 D of against-the-rule astigmatism with a steep K reading of greater than 48.00 D OU. The IOL noted on the IOL card corrects approximately 4.00 D of astigmatism at the corneal plane. It is possible that residual astigmatism was not discussed preoperatively with the patient. Given the high against-the-rule astigmatism, does she have an ectatic disorder such as pellucid marginal degeneration? She is 84 years old, but could an ectatic disorder have caused additional astigmatism to develop after surgery? We would acquire topography, or tomography would be performed.
Each of the issues should be addressed. Selective laser trabeculoplasty can be considered as a means of IOP control that does not affect the ocular surface, or additional IOP-lowering drops can be started if the IOP is unacceptable. An Nd:YAG laser capsulotomy can be performed if the PCO is thought to be visually significant. A trial of sodium chloride hypertonicity ophthalmic solution 5% (Muro 128, Bausch + Lomb) can be conducted followed by repeat manifest refraction and topography. Lid scrubs, meibomian gland expression, and OSD management should be performed to optimize the ocular surface. Rigid gas permeable and scleral contact lenses can be considered after the aforementioned measures to maximize the patient’s BCVA. Her UCVA is not given in the case presentation, but her optimized BCVA after the management described may be acceptable.

ERIC D. ROSENBERG, DO, MSCENG
Medical management should almost always take precedence over surgical management. The physical examination findings and the diagnostic imaging are consistent with mild to moderate Fuchs dystrophy.
I would like to know whether the patient experiences an improvement in her vision over the course of the day. Is it worst in the morning? Does it get better after she blows her hair dry? If it’s the latter, then there may be corneal edema relative to the baseline corneal thickness even though edema seems to be absent on physical examination. Over the years, I have come to realize that many of my patients with Fuchs dystrophy who have undergone Descemet membrane endothelial keratoplasty have a central corneal thickness in the range of 420 to 470 µm. Because the patient’s right eye has a central corneal thickness of 550 µm, it may not show occult signs of swelling or scarring on examination.
The toric IOLs are centered and on axis, but the patient’s BCVA is reduced. My first step would therefore be to prescribe sodium chloride hypertonicity ophthalmic solution 5%, with one drop administered to each eye three times in the morning and the instillations spaced 5 minutes apart. The results of treatment should indicate whether the patient’s Fuchs dystrophy is visually significant, requiring continuous medical management and possibly surgical management in the future.

WHAT I DID: ALANNA NATTIS, DO, FAAO
I thought that the patient’s fluctuating vision was likely caused by either evaporative dry eye disease or symptomatic Fuchs dystrophy. Staining with lissamine green and fluorescein dye, however, revealed no obvious OSD. Guttae were present in each eye, but there was no occult evidence of corneal decompensation or edema. Moreover, the patient complained of fluctuating vision throughout the day, not just in the morning. This is more typical of Fuchs dystrophy. An examination found no evidence of pseudophacodonesis. Ultrasound biometry confirmed that the power and axial orientation of each IOL were correct.
Based on these findings, I suspected that the patient was experiencing subclinical episodes of corneal edema and initiated topical therapy with sodium chloride hypertonic ophthalmic solution 5% administered four times daily in each eye.
At a follow-up visit 3 weeks later, the patient reported a subjective improvement in her vision but noted that it was now blurrier in the morning than in the afternoon. Her BCVA remained 20/25 OD and 20/40 OS. An examination found no evidence of corneal edema, and ultrasound pachymetry readings were unchanged from her initial visit. I adjusted her dosing regimen of sodium chloride hypertonic ophthalmic solution 5% to hourly administration upon waking for a total of three instillations and one dose administered at bedtime. I asked her to return in 1 month for a morning appointment.
At her follow-up 1 month later, the patient reported that the fluctuations were significantly better and said that her vision had improved. Her BCVA was +0.50 -1.00 x 90º = 20/25 OD and +0.75 -1.50 x 100º = 20/30 OS, likely from corneal deturgescence. She was content to continue her medication regimen, and she was happy not to require further surgical intervention.
Two years later, the patient continues to adhere to the prescribed therapy, and she has not required additional intervention.