Advances in ophthalmology help keep our passion for the field alive. Unfortunately, some innovations are not covered by insurance, and patients must pay out of pocket for their use. This can present a dilemma for us as surgeons when our patients cannot afford a treatment from which we believe they could derive benefit. In this situation, we sometimes must set financial consideration aside in order to do what we think is in the patient’s best interest. If we are lucky, our efforts are supported by industry, which reduces our costs. This article shares an example of mine.
ABOUT MARFAN SYNDROME
The worldwide incidence of classic Marfan syndrome (MFS) is approximately one in 5,000 individuals.1 I started working with patients who have MFS in 2000 through a German patient support group.
MFS is an autosomal dominant disorder of the connective tissue that can cause cardiovascular, ocular, and skeletal abnormalities. Ocular involvement is subdivided into major and minor criteria. Ectopia lentis and lens coloboma of any degree are major criteria. At least two of the following minor criteria must be present for a patient to be considered to have ocular involvement:
- An abnormally flat cornea;
- Increased axial length; and
- Hypoplasia of the ciliary muscle or iris that is causing decreased mydriasis.
Mean keratometry values of less than 42.00 D are highly correlated with a diagnosis of MFS. Other secondary manifestations are early severe myopia, retinal detachment, early cataract, glaucoma, amblyopia, and strabismus.
Ectopia lentis occurs in 50% to 80% of patients with MFS, and it is often the presenting sign. In such situations, vision is altered primarily by refractive errors such as high myopia, astigmatism, and induced anisometropia.
SURGical considerations
Surgical intervention to address a dislocated lens due to loose zonules is almost always challenging. An additional consideration is that patients with ectopia lentis from MFS are frequently young.
The most difficult part of surgery in eyes with ectopia lentis is the capsulotomy. A manual approach places stress on the zonules and can cause complete dislocation of the crystalline lens and/or capsular bag. A vitrectomy is often necessary during cataract surgery, which makes the operation more traumatic to the eye.
CASE PRESENTATION
I had been performing laser cataract surgery for several months when a 23-year-old patient with MFS presented with increased lens dislocation in 2013 (Figures 1 and 2). It seemed reasonable to me to consider the benefits of performing the capsulotomy with a femtosecond laser. I contacted technical support at Lensar to discuss the case and decided to proceed with the understanding that it was the first time laser cataract surgery would be performed worldwide on the eye of a patient with MFS.
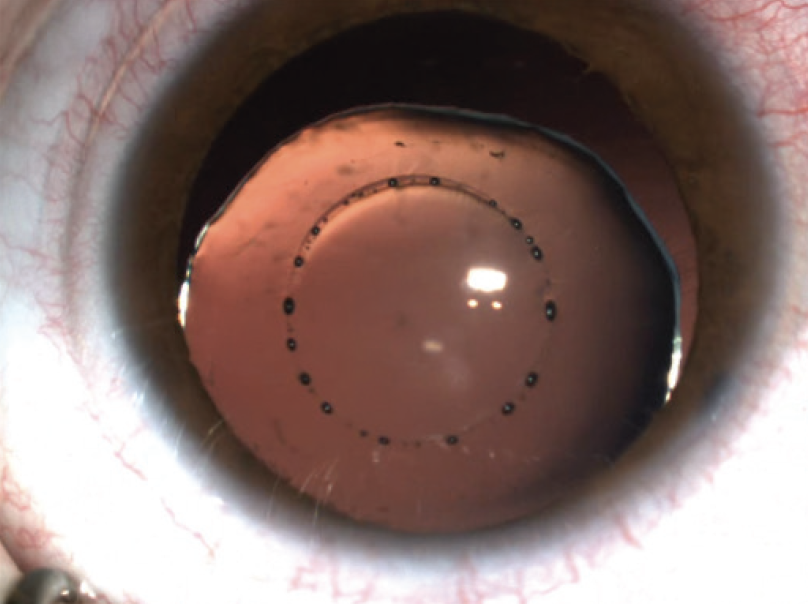
Figure 1. The lens is dislocated in this patient with MFS.
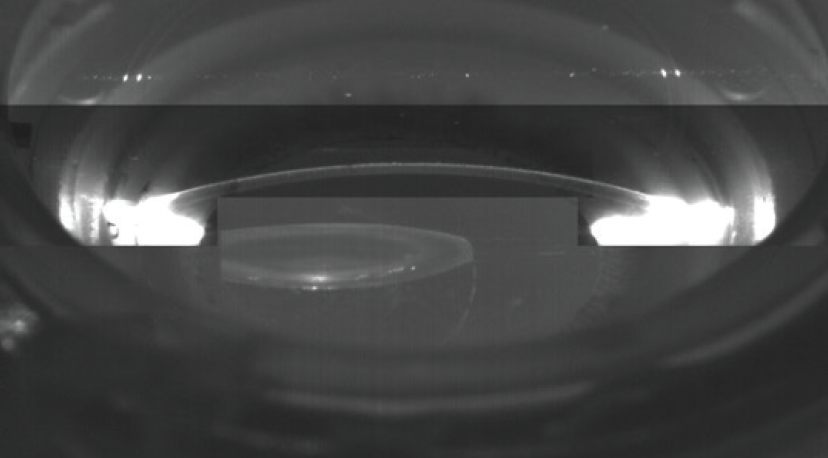
Figure 2. Scheimpflug image of the dislocated lens.
Surgery was performed without complication. A laser was used to perform the capsulotomy and fragment the lens. The capsular bag was stabilized with iris hooks, which were enclaved into the capsulotomy to support the bag during lens aspiration. Scleral fixation of an 11-mm capsular tension ring (Type 1L, Morcher) was performed to stabilize and center the capsular bag. A soft, hydrophilic, one-piece IOL was inserted through a 2.2-mm limbal incision, and it unfolded in a controlled fashion within the capsular bag.
The patient has returned for regular follow-up since undergoing surgery, and he has experienced no complications. He underwent laser cataract surgery with the same technique on the contralateral eye this past year (Figure 3).

Figure 3. Dr. Holland and his first laser cataract surgery patient with MFS.
CONCLUSION
Technical support and partial funding from Lensar allowed me to offer laser cataract surgery to a patient who could otherwise not afford it. Based on the successful experience, I have since performed laser cataract surgery on more than 20 patients with MFS. I find a laser capsulotomy to be superior to a manual approach in patients with ectopia lentis from MFS, and I now recommend laser cataract surgery to all my patients in this situation.
1. Marfan syndrome. MedlinePlus. Accessed January 28, 2022. https://medlineplus.gov/genetics/condition/marfan-syndrome