CASE PRESENTATION
A 64-year-old man is referred for a cataract evaluation of his right eye. The patient says that the vision in this eye has been reduced since it was injured by a hockey stick 20 years ago. He likens the current vision in his right eye to looking through mud and describes extreme light sensitivity. The patient was originally referred to a retina specialist out of concern that retinal surgery would be necessary at the time of cataract removal.
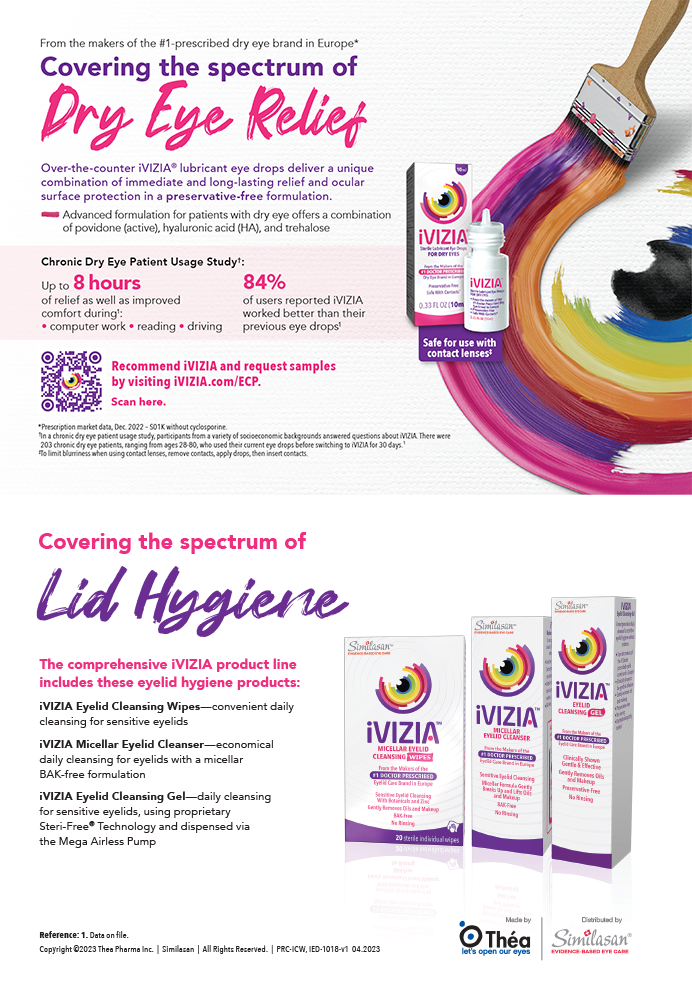
On examination, the patient’s BCVA is 20/400 OD, and his UCVA is 20/20 OS. An afferent pupillary defect is visible in the right eye, and the right pupil is irregular. A slit-lamp examination of the eye shows a quiet conjunctiva and a clear cornea. The iris is nonreactive and fixed at approximately 7 mm with several small sphincter tears. A hypermature cataract and zonular dehiscence in the temporal quadrant are evident (Figure 1). A slit-lamp examination of the left eye is within normal limits.
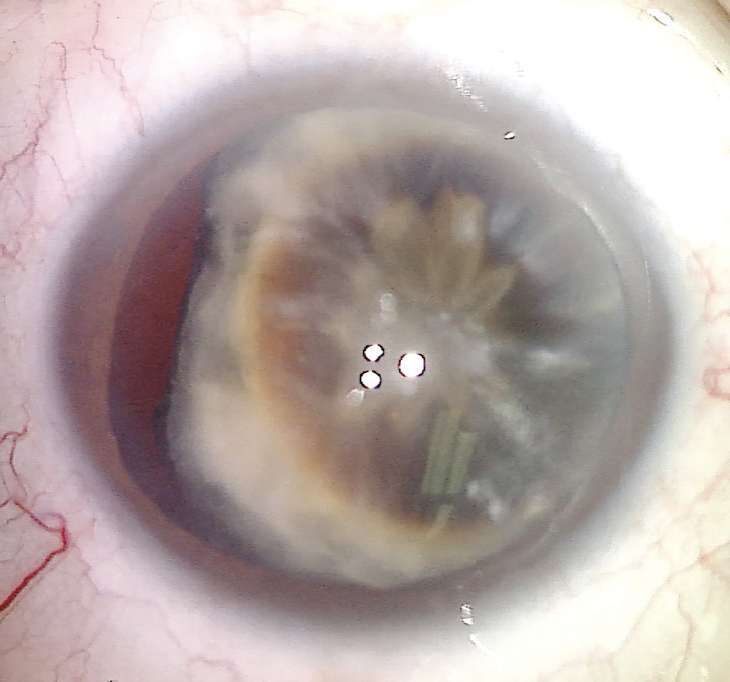
Figure 1. The preoperative appearance of the undilated pupil of the right eye. A mature cataract and temporal zonular dehiscence are evident.
Visualization of the posterior segment of the right eye is challenging because of the mature nature of the lens. There is no evidence of a retinal detachment or mass on a B-scan ultrasound. A dilated examination of the left eye shows a healthy optic nerve and retina.
How would you proceed?
—Case prepared by Brandon D. Ayres, MD

CRISTOS IFANTIDES, MD, MBA
An illuminated muscle light would be placed against the closed eyelid and sclera to elicit entopic phenomena and determine if the patient can see a Purkinje tree. This quick test can indicate the gross visual potential of an eye with an opaque cataract. If the result is relatively symmetric between the two eyes, sutureless extracapsular surgery (manual small-incision cataract surgery [MSICS]) with a pars plana–assisted anterior vitrectomy would be my recommendation.
After the placement of an anterior chamber maintainer and 23-gauge pars plana port, triamcinolone acetonide would be administered to identify vitreous in the anterior segment, and a pars plana–assisted anterior vitrectomy would be performed to pull any vitreous backward. The capsule would be stained with trypan blue dye, and a vitrector would be used to remove the dye from the posterior segment. A superior peritomy would then be created. A superior tunnel approach would be used for the main MSICS incision to avoid the area of zonular loss.
An 8-mm capsulotomy would be created, and then the entire lens would be prolapsed into the anterior chamber and delivered out of the main wound. If the bag remains stable, a capsular tension ring (CTR) would be inserted, and an Ahmed Segment (Morcher) would be placed temporally to stabilize the IOL–capsular bag complex. If the capsular bag cannot be salvaged or if it has fused to the lens, it would be removed, followed by scleral fixation of an IOL using a modified Yamane/MSICS technique.
It is imperative to decrease the pupillary aperture to address the patient’s extreme light sensitivity. Multiple 10-0 polypropylene (Prolene, Ethicon) sutures on a CIF-4 needle would be placed for the pupilloplasty using a single-pass four-throw technique.

ABHAY R. VASAVADA, MS, FRCS
The patient should be informed of both the primary surgical plan and the backup plan in case the nucleus drops or the posterior capsule ruptures during surgery. Laser cataract surgery would be my preference in this eye with a dense, mature cataract, and preexisting zonular loss because it would allow me to perform an OCT-guided anterior capsulotomy of the desired size and centration. The nucleus would be divided into as many pieces as possible with a horizontal chopping technique, torsional ultrasound, and maximum vacuum. I would be sure to divide the leathery central plate, and I would avoid excessive lateral separation maneuvers because of the compromised capsular bag. Capsular hooks would be placed to help stabilize the bag.
Repeated injections of a dispersive OVD would be performed. If the nucleus can be successfully removed, a Cionni CTR (Morcher) would be used to fixate the bag to the scleral wall with a PTFE (Gore-Tex, W.L. Gore & Associates) suture. After IOL implantation, a single-pass four-throw pupilloplasty would be performed.
If the posterior capsule ruptures or the nucleus drops during the procedure, a thorough pars plana anterior vitrectomy would be performed. In this situation, my preference would be to use Yamane’s flanged IOL fixation technique.1 If a retina surgeon is not available to comanage the case, an adequate anterior vitrectomy should be performed, the eye should be sutured, and the patient should be referred a retina surgeon.
If the operating surgeon does not feel confident about performing phacoemulsification on the eye, intracapsular cataract extraction and the scleral or intrascleral fixation of the IOL are appropriate choices.

WHAT I DID: BRANDON D. AYRES, MD
The risks and benefits of and alternatives to surgery were discussed extensively with the patient. Informed consent for complex cataract surgery with possible anterior vitrectomy and an iris repair was obtained. Possible limitations in vision were also discussed extensively with the patient because it was evident that the optic nerve had sustained damage.
After the creation of two paracenteses and a 2.4-mm main incision, the anterior chamber was filled with an OVD. The anterior capsule was painted with trypan blue dye to improve visualization of the continuous curvilinear capsulorhexis (CCC). After the CCC was performed, two capsular support hooks were placed in the temporal meridian to help prevent further zonular loss (Figure 2). Because the cataract was hypermature, a hybrid approach to disassembling the lens was taken. Phacoemulsification was performed to create a central groove in the lens. An OVD was then used to create space between the anterior capsule and the lens, after which a miLoop (Carl Zeiss Meditec) was placed in line with the groove and the lens was bisected. The lens was rotated 90º, and the miLoop was used to divide the lens into quadrants (Figure 3). The lens material was removed with phacoemulsification, and retained cortical material was removed with irrigation and aspiration.
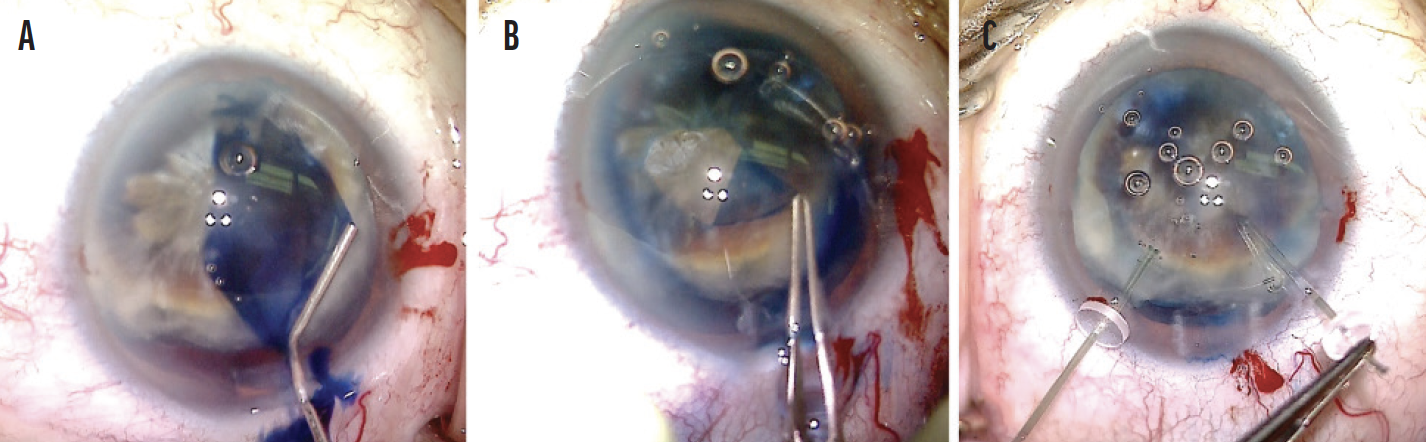
Figure 2. The capsule is painted with trypan blue dye (A), a CCC is created (B), and capsular retractors are placed in the bag (C).
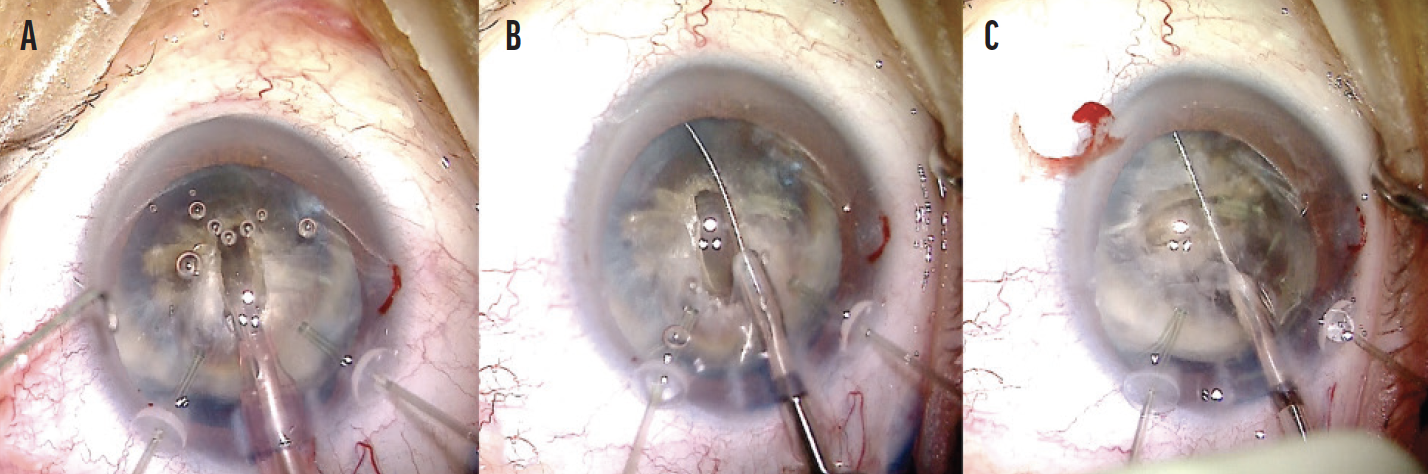
Figure 3. The lens is divided with phacoemulsification and the use of a miLoop. A groove in the lens is created with phacoemulsification (A). A miLoop is placed in the capsular bag directly in line with the groove, and the device is used to bisect the lens (B). The lens is rotated 90º, and the miLoop is used once again to bisect the lens into four quadrants (C).
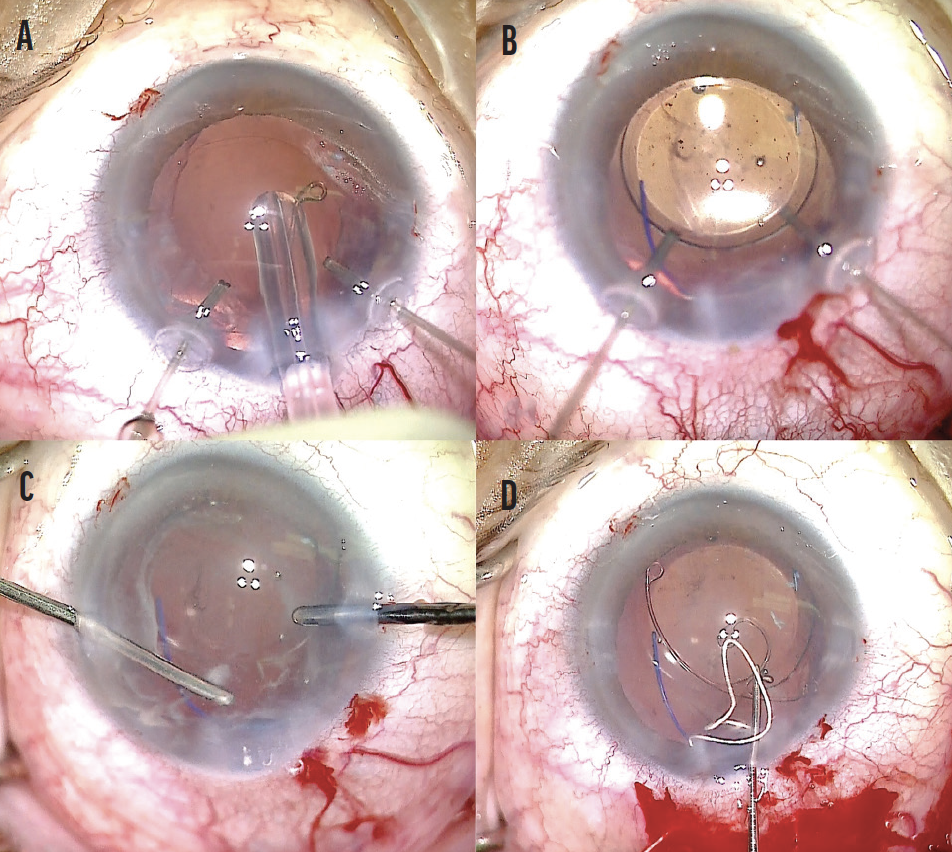
Figure 4. A CTR is placed in the capsular bag (A). A three-piece IOL is inserted into the capsular bag, and the haptics are positioned in line with the zonulopathy (B). An anterior vitrectomy is performed, and triamcinolone acetonide is instilled to help visualize the vitreous (C). An Ahmed Segment is used for fixation of the capsular bag and centration of the IOL (D).
To manage the zonulopathy, a peritomy was created in the temporal conjunctiva, and two scleral incisions were created 3 mm apart approximately 2.5 mm posterior to the limbus. An Ahmed Segment was laced with a 7-0 PTFE suture. Using a handshake technique, the PTFE suture was threaded into the eye of the capsular tension segment and through the main incision. The suture was then externalized through the scleral incision. The segment was carefully positioned in the capsular bag, and the suture was tied and adjusted on the scleral surface to ensure proper IOL centration. The knot was buried in the scleral wound, and the conjunctiva was sutured closed.
The last step of the surgery was to repair the iris. Luckily, a test using microforceps revealed that the iris tissue had not lost its elasticity. A polypropylene cerclage suture was used to reduce the pupil size to approximately 4 mm (Figure 5). Once the knot was secure, the OVD was removed with the I/A unit. The incisions were then hydrated and found to be watertight.
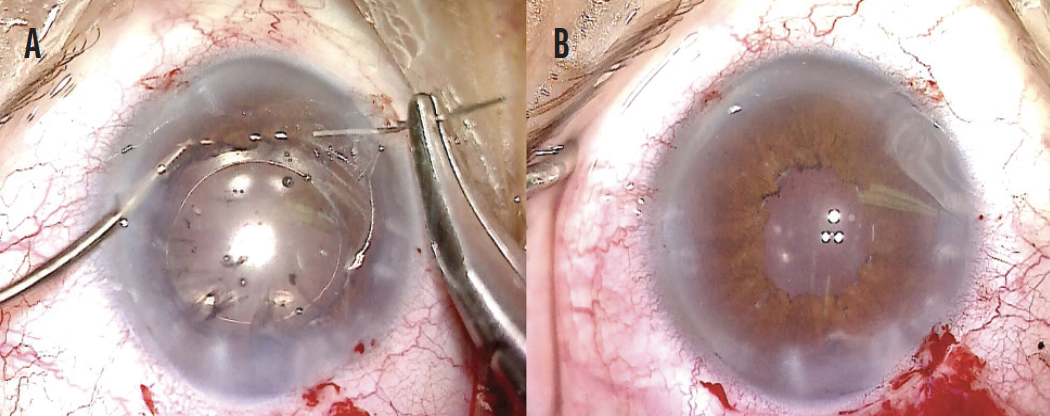
Figure 5. A 10-0 polypropylene cerclage suture (A). At the end of the case, the IOL is well positioned, and the cerclage suture is completed (B).
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.