The Buzz on EDOF IOLs
AcrySof IQ Vivity
Ashley Brissette, MD, MSc, FRCSC

The AcrySof IQ Vivity (Alcon; Figure 1) is a nondiffractive extended depth of focus (EDOF) lens. Whereas traditional refractive multifocal IOLs use rings to split light energy, the Vivity’s innovative design of two transition zones reshapes the wavefront—what the company refers to as X-Wave technology. Specifically, a 1-µm plateau located on the central 2.2-mm optic creates a transition that shapes and stretches the wavefront. Shifting the wavefront anterior to the retina can provide intermediate (66 cm) and near (44 cm) vision.

Figure 1. The AcrySof IQ Vivity.
Courtesy of Alcon
The Vivity is the first nondiffractive EDOF lens available in the United States. The nondiffractive design helps to reduce the incidence (reported at < 3.8%) of visual disturbances compared to diffractive designs (data on file with Alcon). In FDA clinical studies, 89% of patients achieved 20/25-2 or better uncorrected distance visual acuity, 86% achieved 20/25-2 or better uncorrected intermediate visual acuity, and 91% achieved 20/40-2 or better uncorrected near visual acuity.1 The Vivity can provide excellent vision in bright and dim environments because the X-Wave technology functions independently of pupil size.
In my experience, the Vivity can provide patients with a range of vision while limiting the dysphotopsias they experience. This IOL can be an excellent option for the following individuals:
- Those who wish to be less dependent on glasses after cataract surgery but who are not good candidates for a multifocal lens because of mild glaucoma, higher-order aberrations after refractive surgery, or ocular surface disease; and
- Those who may be bothered by dysphotopsias and have concerns about their quality of vision when driving at night.
Another factor in my use of the Vivity is that intermediate vision has become more important to my patients. Many of them spend a lot of time looking at computer screens, tablets, and smartphones, and they want to be able to read a menu at a restaurant. The Vivity does not require patients to sacrifice quality distance vision to gain intermediate and near vision. That said, I counsel patients that they may need to wear glasses to read fine print and note that they probably will not require glasses for most daily activities.
1. Alcon. AcrySof IQ Vivity patient information brochure. Accessed December 16, 2021. www.accessdata.fda.gov/cdrh_docs/pdf/P930014S126D.pdf
Tecnis Symfony and Tecnis Synergy IOLs
Daniel H. Chang, MD

More than 5 years ago, the Tecnis Symfony IOL (Johnson & Johnson Vision) became the first EDOF IOL approved by the FDA for the treatment of presbyopia. More recently, in April 2021, the nontoric Tecnis Synergy and the toric Tecnis Synergy Toric II (Johnson & Johnson Vision) IOLs—hybrid EDOF/trifocal lenses—received FDA approval. I have implanted the Symfony IOL in my mother and mother-in-law, which speaks to the confidence I have in its ability to achieve great outcomes and patient satisfaction. That said, there are limitations with all presbyopia-correcting IOLs, including the potential for unwanted visual phenomena.
When selecting a presbyopia-correcting IOL for my patients, I attempt to strike a reasonable balance between vision quality, range of vision, and dysphotopsias. The primary reason to remove a dysfunctional lens or a cataract is to improve vision quality. Increasing patients’ range of vision with a pseudoaccommodating IOL entails a trade-off in vision quality and the potential induction of dysphotopsias, particularly in low-light and low-contrast conditions such as when driving at night.
The Tecnis Multifocal IOLs (Johnson & Johnson Vision) were the first IOLs available on the US market to correct spherical aberration and to compensate for the loss of vision quality inherent to multifocality. In addition to correcting spherical aberration, according to the Tecnis Symfony’s directions for use, the IOL actively corrects chromatic aberration to deliver vision quality comparable to that achieved with a monofocal IOL.1 The Symfony also provides good intermediate and near vision.
The Tecnis Symfony is associated with a lower level of dysphotopsias than multifocal IOLs. This, however, might have been oversold, leading to unrealistic expectations and dissatisfaction among patients and surgeons. Thankfully, there are now two major improvements to the Tecnis Symfony’s material and design. A violet light filter (OptiBlue; Figure 2) was added to lessen the severity of halos while still allowing the transmission of blue light, which is important for scotopic vision and circadian rhythm entrainment. Improvements in the manufacturing and lathing process further reduced light scatter to improve contrast and to reduce starburst symptoms.
Figure 2. The Tecnis Symfony plus OptiBlue.
Courtesy of Johnson & Johnson Vision
I have implanted hundreds of Tecnis Symfony OptiBlue IOLs during the past year. I have encountered fewer patient complaints about dysphotopsias, I have found the lens to be more tolerant of refractive error, I have performed fewer refractive enhancements, and I have spent less overall chair time with patients. My colleagues and I have initiated a prospective randomized controlled trial to validate these observations. The Tecnis Symfony OptiBlue IOL may not have as wide a range of vision as the Tecnis Synergy IOL, but the latest version of the Symfony promises to improve on its predecessor as a well-tolerated option that can provide excellent vision quality while minimizing dysphotopsias. (For more on the Tecnis Synergy IOL, see “Is the Needle Moving?,” and “As IOL Technology Improves, There Is Less Reason to Mix and Match.”)
1. Johnson & Johnson Vision. Tecnis Symfony Extended Range of Vision IOL DFU. Accessed January 27, 2022. https://www.jnjvisionpro.com/sites/us/files/public/z311215_01.pdf
Small-Aperture Lens
John A. Vukich, MD

Small-aperture or pinhole optics increase depth of focus and depth of field. This concept has been around for centuries, and it is one that ophthalmologists learn during their first week in the clinic when they use a pinhole to refine refractions.
When a small aperture is used to extend the intermediate and near vision ranges, it also collimates stray rays of light passing through an aberrated cornea. A small-aperture IOL can therefore benefit patients who have atypical corneas such as those with keratoconus, corneal scarring, or a history of radial keratotomy. It can also be an appropriate lens for patients who desire blended vision to enhance their near vision.
LENS CHARACTERISTICS
The IC-8 IOL (AcuFocus; Figure 3) is a one-piece, aspheric, hydrophobic acrylic, monofocal lens with an embedded mask. The IOL has a large landing zone for achieving an emmetropic result, and it can eliminate much of the noise in the visual system from higher-order aberrations. The lens’ wavefront-filtering design eliminates unfocused peripheral rays so that only central rays focus on the retina. Its small aperture provides an extended depth of focus that makes the implant more tolerant of residual sphero-cylindrical refractive error than a multifocal IOL.
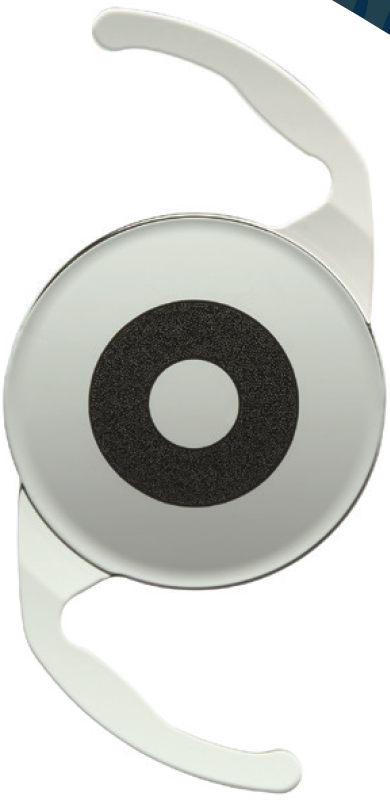
Figure 3. The IC-8 IOL.
Courtesy of AcuFocus
The IC-8 IOL is not currently available in the United States, but it has been used abroad for years with excellent results. Studies have shown that the IC-8 can provide up to 3.00 D of extended depth of focus and tolerate up to 1.00 D of deviation from the target manifest refraction spherical equivalent (data on file with AcuFocus). The IC-8 is not a toric IOL, but its pinhole effect can negate the optical effect of up to 1.50 D irregular astigmatism.
MY EXPERIENCE
I have served as a principal investigator and medical monitor of the IC-8 FDA clinical trials. The lens is unique in that it can achieve a variety of blended vision results. For example, an emmetropic endpoint may be used for distance in one eye, and an IC-8 may be implanted in the contralateral eye with a target of -0.75 D myopia. The depth of focus achieved with the IC-8 can avoid compromising the patient’s distance vision, so binocular vision and depth perception are maintained. This makes the lens a good choice for patients who desire blended vision to enhance their near vision in addition to patients who have atypical corneas.
Update on Trifocal IOLs in the United States
By Bret L. Fisher, MD

Presbyopia-correcting IOLs are an important and growing segment of the cataract surgery market in the United States. (Editor’s note: For more on this topic, see “Is the Needle Moving?,” pg 30.) Currently, approximately 40% of my cataract surgery patients elect to receive some type of premium IOL, and most of these lenses are presbyopia-correcting IOLs. By lessening or eliminating patients’ dependence on glasses after surgery, presbyopia-correcting IOLs can increase their postoperative satisfaction.
As a refractive cataract surgeon, I have an almost overwhelming number of IOLs from which to choose. (Editor’s note: For more on this topic, see “The Positive and Negative Ripple Effects of Expanded IOL Options,” pg 46.) An important recent addition to the IOL technology available in the United States is a trifocal lens, the AcrySof IQ PanOptix IOL (Alcon).
ABOUT THE IOL
I first implanted a PanOptix IOL in 2017 while serving as an investigator for the FDA trials (Figure 4). This lens’ share of the US presbyopia-correcting IOL market is approximately 74%, and more than 1.4 million PanOptix lenses have been implanted globally (data on file with Alcon).
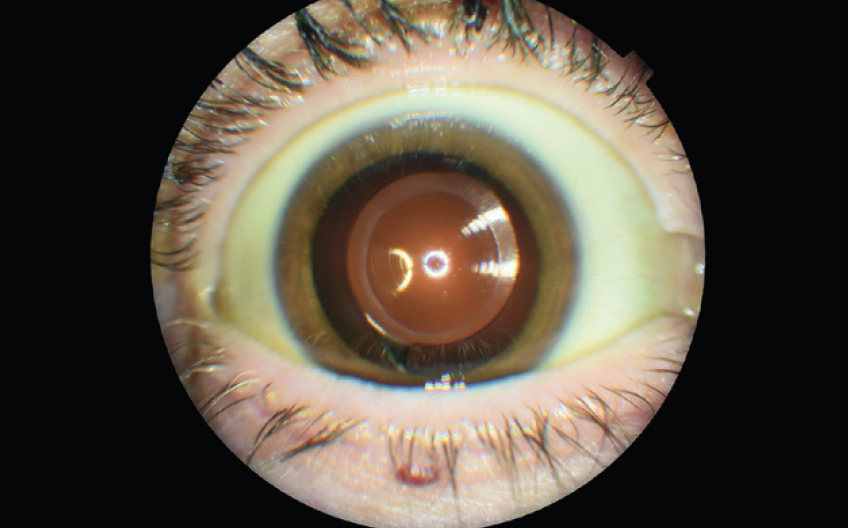
Figure 4. Postoperative image of the PanOptix IOL in situ.
Courtesy of Bret L. Fisher, MD
The PanOptix is available in a wide range of spherical and cylindrical powers. It is my go-to lens for patients who want the greatest degree of spectacle independence after cataract surgery. I appreciate the range of vision that the IOL provides: All my patients in the FDA study achieved 20/25 or better visual acuity through the entire visual range.1 The rate of nighttime dysphotopsias has been low and acceptable; most of my patients describe dysphotopsias as mild.
PATIENT SELECTION
I consider any patient who expresses a desire for spectacle independence after cataract surgery to be a candidate for the PanOptix IOL unless they have significant macular, optic nerve, or corneal disease. For example, individuals with uncontrolled, advanced dry eye disease or significant corneal scarring or guttata are poor candidates for a trifocal IOL. Patients with epithelial basement membrane dystrophy, however, may be able to achieve success with the PanOptix after undergoing a superficial keratectomy. I routinely implant the lens in patients with a history of LASIK (off-label use) and have achieved good results. I determine candidacy on a case-by-case basis.
I am particularly careful about setting realistic expectations in patients with low to moderate myopia who are used to reading without glasses. The preoperative conversation with these individuals tends to be longer than with other patients.
1. Fisher BL. Cumulative visual acuity of a novel trifocal IOL. Paper presented at: ASCRS/ASOA Annual Meeting; May 3-7, 2019; San Diego.
New-Generation Monofocal IOLs
By Jeremy Z. Kieval, MD; Karl G. Stonecipher, MD; and Elizabeth Yeu, MD
The Tecnis Eyhance
Jeremy Z. Kieval, MD

The FDA approved the Tecnis Eyhance and Eyhance Toric II IOLs (both from Johnson & Johnson Vision; Figure 5) in February 2021. The Eyhance is the first in a new class of monofocal IOLs available in the United States that provides additional depth of focus without sacrificing the modulation transfer function or inducing dysphotopsias that are associated with multifocal and EDOF IOLs.

Figure 5. The Eyhance Toric II IOL.
Courtesy of Johnson & Johnson Vision
FILLING A GAP
I have found that anyone undergoing cataract surgery can benefit from the extended depth of focus that the Eyhance IOL offers.1,2 The IOL also fills a gap in my patient population, namely the following three groups:
- Individuals who cannot afford a presbyopia-correcting IOL;
- Those who hesitate to choose a presbyopia-correcting IOL because of concerns about halos; and
- Those who are not candidates for a presbyopia-correcting IOL because of ocular pathology.
The Eyhance can improve uncorrected intermediate visual acuity, and many of my patients have noticed a slight increase in their depth of focus when working at the computer or viewing the dashboard while driving a car. Because the Eyhance is classified as a monofocal IOL, I do not present any expectations for presbyopia correction when discussing this lens with patients. Instead, I focus the conversation on the refractive target. That said, my patients in whom a plano refraction is targeted with this lens are more likely to have a reduced need for reading glasses after surgery than those who received a standard Tecnis monofocal IOL (Johnson & Johnson Vision).
In my experience, the Eyhance performs exceptionally well in patients who elect a monovision or a myopic refractive target. When a postoperative refraction of -1.00 to -1.25 D is targeted in the near eye, the implantation of this IOL allows most patients to have a full depth of focus from intermediate to near, and they can often read to J1+. Pseudophakic monovision is not the same as phakic monovision, but my patients who receive an Eyhance are less likely than those with a standard monofocal IOL to complain about needing reading glasses.
1. Mencucci R, Cennamo M, Venturi D, Vignapiano R, Favuzza E. Visual outcome, optical quality, and patient satisfaction with a new monofocal IOL, enhanced for intermediate vision: preliminary results. J Cataract Refract Surg. 2020;46(3):378-387.
2. Auffarth GU, Gerl M, Tsai L, et al; Quantum Study Group. Clinical evaluation of a new monofocal intraocular lens with enhanced intermediate function in cataract patients. J Cataract Refract Surg. 2021;47(2):184-191.
RayOne EMV
Karl G. Stonecipher, MD

The RayOne EMV (model 200E, Rayner) is a UV light–absorbing one-piece IOL intended for placement in the capsular bag using the RayOne injection system (Rayner). Antivaulting haptic technology allows the IOL to be implanted through a sub–2.2-mm corneal incision and promotes rapid centration and fixation in the capsular bag. The IOL is available in powers from 10.00 to 30.00 D in 0.50 D increments. A toric version is not currently available. The lens has an Abbe value of 56; that of the crystalline lens is 47. The refractive index values of the RayOne EMV and crystalline lens are 1.46 and 1.4, respectively.1 Three to 6 months after surgery, the average offset was 0.08 mm, and mean rotation of the IOL was 1.83º in one study.2 In another study, the posterior capsular opacification rate was 1.7% at 24 months.3 The RayOne EMV is unique because it has positive spherical aberration at the center of its optic and a blended edge region to maintain visual acuity and contrast sensitivity (Figure 6). Graham D. Barrett, MB BCh SAf, FRACO, FRACS, designed the IOL for patients who can tolerate defocus in the second eye or monovision. Even with a target of plano in both eyes, patients can achieve an increased range of vision and improvement in functional intermediate and near vision (data on file with Rayner). With a monovision strategy, elongated optical performance in the hyperopic direction allows the lens to maintain some distance vision in the patient’s nondominant eye. By complementing natural positive corneal spherical aberration, the RayOne EMV can provide consistent visual results across a wide range of corneas and optic alignments (Figure 7).
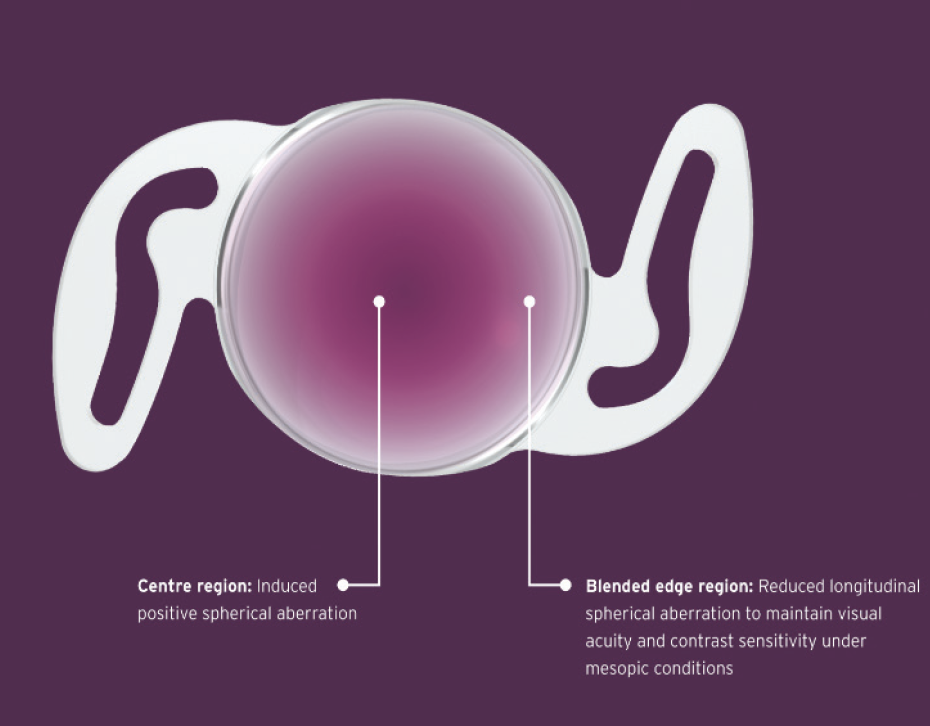
Figure 6. The different regions of the RayOne EMV that make its design unique.
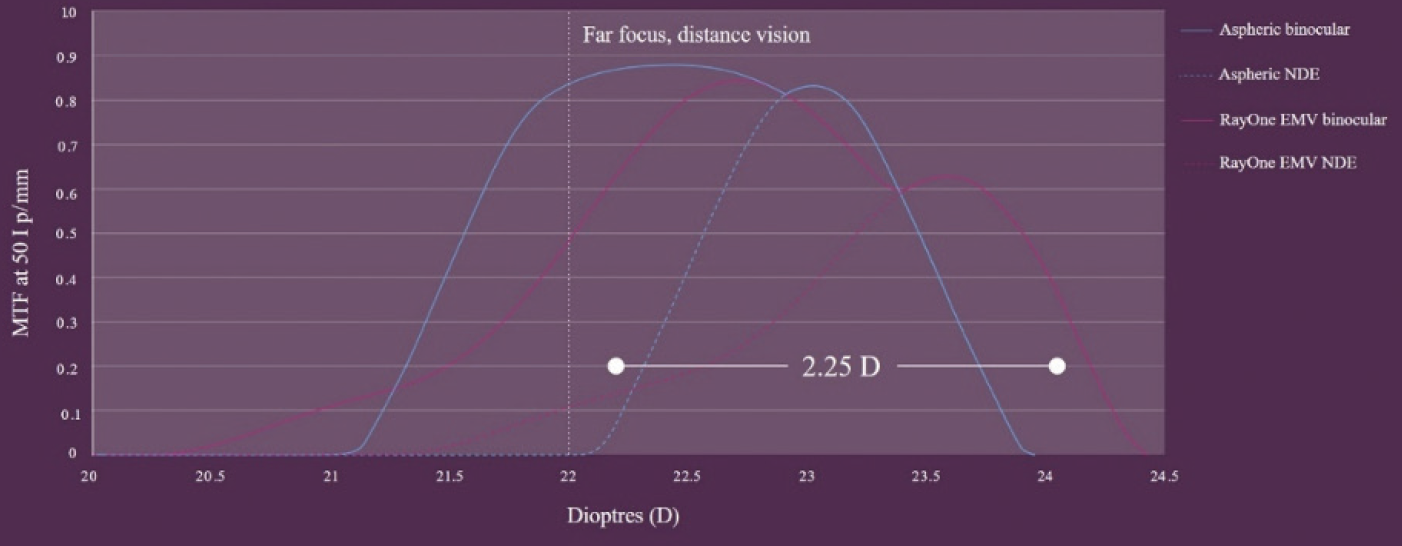
Figure 7. The modulation transfer function graph shows the binocular optical performance of the RayOne EMV and of a competitor’s negatively aberrated aspheric IOL when targeted for a monovision offset of 1.00 D.
PERSONAL PREFERENCES
I use the RayOne EMV as an increased-range-of-vision lens. Because a toric version is not currently available, my candidates for the IOL are patients who have less than 1.50 D of astigmatism and those I expect will benefit from and be able to tolerate monovision. I currently limit the use of the IOL to individuals with normal corneas and no history of ocular surgery. I use Rayner’s lens constants (Figure 8).
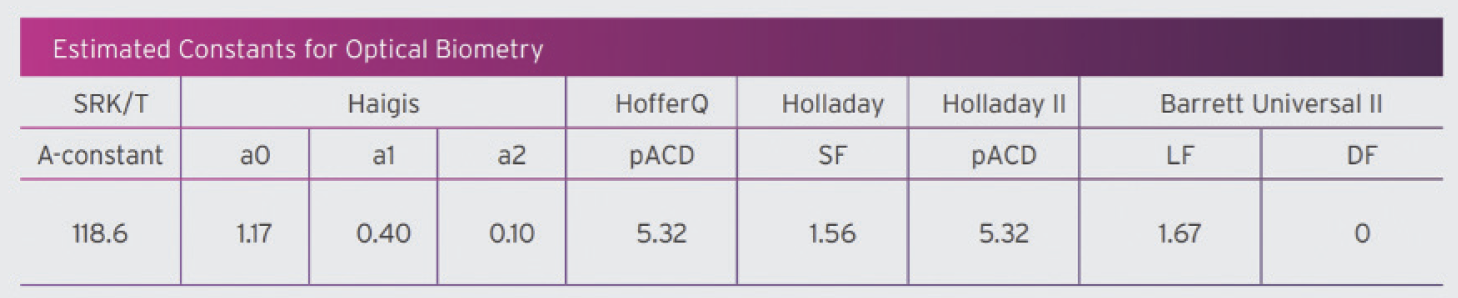
Figure 8. The estimated lens constants of the RayOne EMV for optical biometry.
Figures 6–8 courtesy of Rayner
The RayOne EMV has provided my patients with great distance vision and an increased range of vision at near (Figure 9). Spectacle independence has varied based on how much the offset was adjusted on the second eye (the nondominant eye for most patients), but most of my patients can function without reading glasses. I prefer to correct the first eye for distance vision and then discuss with patients the concept of blended vision to improve their intermediate and/or near vision. None of my patients to date has required a refractive enhancement or IOL exchange.
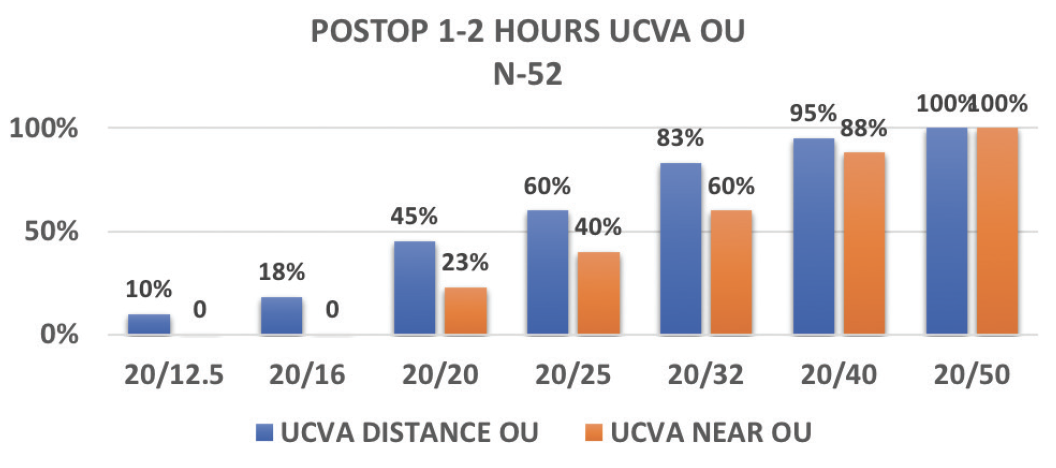
Figure 9. Immediate bilateral postoperative results in patients from Dr. Stonecipher’s practice.
Courtesy of Karl G. Stonecipher, MD
1. Zhao H, Mainster MA. The effect of chromatic dispersion on pseudophakic optical performance. Br J Ophthalmol. 2007;91(9):1225-1229.
2. Bhogal-Bhamra GK, Sheppard AL, Kolli S, Wolffsohn JS. Rotational stability and centration of a new toric lens design platform using objective image analysis over 6 months. J Refract Surg. 2019;35(1):48-53.
3. Mathew RG, Coombes AGA. Reduction of Nd: YAG capsulotomy rates after implantation of a single-piece acrylic hydrophilic intraocular lens with 360º squared optic edge: 24-month results. Ophthalmic Surg Lasers Imaging. 2010;41(6):651-655.
IPure
Elizabeth Yeu, MD

Refractive results have never been more important to cataract surgery patients than they are today. Practitioners aim to provide patients with a greater depth of focus as well as higher quality of vision, and several IOLs on the market are designed with these goals in mind. The IPure (Beaver-Visitec International) is a monofocal IOL with a uniquely patented aspheric optic design that provides high contrast sensitivity in various lighting conditions; maintains natural corneal depth of focus; and is less sensitive to natural off-axis conditions, lens decentration, and corneal aberrations.1
LENS DESIGN
The IPure is a modified spherical aberration lens, and it has the benefits of both a spherical and a negative aspheric IOL. The three-zone aspheric optic of the IPure is designed to increase depth of focus (Figure 10).1 The 2.4-mm central optical zone (zones 1 and 2) has neutral spherical aberration, providing better contrast sensitivity than a standard aspheric IOL. Within zone 1, which is the very center of the optic, the spherical aberration is slightly positive. The peripheral optic zone (zone 3) has -0.18 µm spherical aberration.
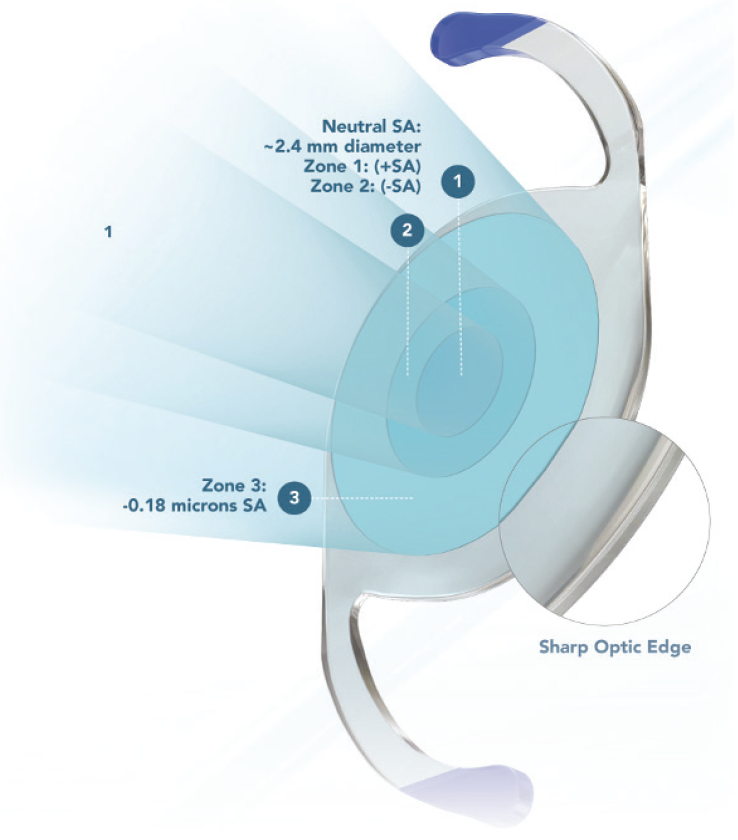
Figure 10. The IPure IOL has a three-zone aspheric optic design.
Courtesy of Beaver-Visitec International
When the pupil is in the dilated state, this optical system can provide higher quality of vision because it neutralizes the corneal spherical aberration and its functional power decreases. The smooth and even optic surface of the IPure is designed to reduce light scattering on the lens surface,2 and a sharp optic edge reduces posterior capsular opacification.
The IPure comes preloaded. The blue haptics are highly visible inside the injector to promote controlled folding. In a study of 600 IOL release bench tests, 100% of the lenses exhibited normal lens-releasing behavior (data on file with Hoya Medical). Further, in one human trial comparing preloaded and nonpreloaded IOL delivery systems, none of the IPure IOLs required additional manipulation in the eye compared to 32% of the IOLs that were manually loaded into an injector.4
CLINICAL USE
The IPure IOL can provide a high quality of vision for any patient, but this lens is a great choice particularly for individuals with aberrated corneas, including those with a history of laser vision correction and those with keratoconus. It’s also a great choice for patients whose corneal aberrations I do not want to alter.
I can confidently implant the IPure in patients who are good candidates for this lens and know that it can provide them with the best of both worlds—higher vision quality and increased depth of focus. In my experience, aiming for -0.25 to -0.50 D in the nondominant eye and plano in the dominant eye provides better intermediate and near vision than what most patients can achieve with a standard monofocal lens.
CONCLUSION
The modified spherical aberration design of the IPure IOL is a unique concept to achieve high contrast sensitivity in various lighting conditions while maintaining natural corneal depth of focus. This IOL has quickly earned a spot in my armamentarium of IOLs.
1. Sanger D et al. Hoya Corporation. Intraocular lens. US Patent No. US8647383. February 11, 2014.
2. Werner L. Glistenings and surface light scattering in intraocular lenses. J Cataract Refract Surg. 2010;36:1398-1420.
3. Chung B, Lee H, Choi M, Seo KY, Kim EK, Kim TI. Preloaded and nonpreloaded intraocular lens delivery system and characteristics: human and porcine eyes trial. Int J Ophthalmol. 2018;11:6-11.
Advances in Light-Adjustable Technology
By Jonathan Solomon, MD, MHA

Cataract surgeons historically have relied on IOLs with fixed powers to meet the visual needs of our patients. The use of such technology, however, requires us to predict both the desired postoperative refraction and the spherical and cylindrical powers of the IOL necessary to attain this target. When selecting an IOL, we must gauge the trade-off between quality and range of vision that each patient will accept.
The availability of the Light Adjustable Lens (RxSight) allows us to avoid making these difficult predictions. The Light Adjustable Lens is made of a special photosensitive material that can be adjusted in response to UV light after lens implantation to correct the patient’s particular refractive error (Figures 11 and 12).
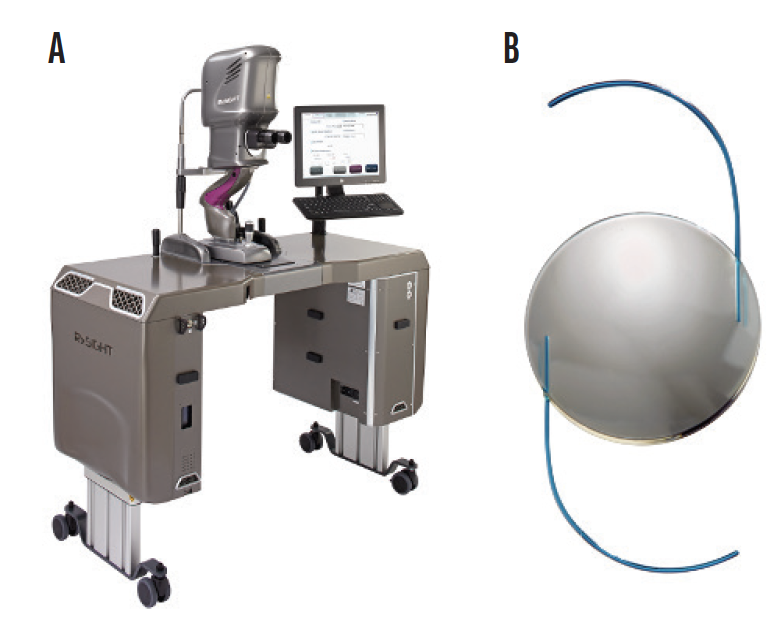
Figure 11. The Light Delivery Device (RxSight; A) delivers targeted UV light to shape the Light Adjustable Lens (B) and precisely customize vision for each patient.
Courtesy of RxSight
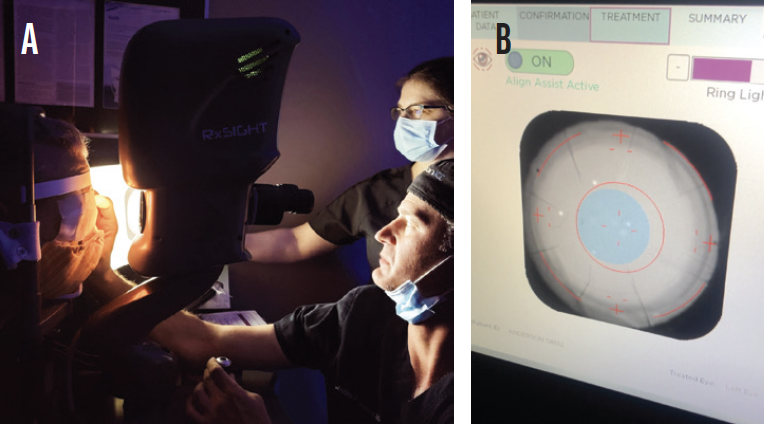
Figure 12. Dr. Solomon performing an in-office treatment with the Light Adjustable Lens (A). The screenshot of a light adjustment treatment for a post–radial keratotomy eye (B).
Courtesy of Jonathan Solomon, MD, MHA
PROCEDURAL STEPS
Step No. 1: Surgery. The Light Adjustable Lens is implanted as a monofocal IOL with a baseline depth-of-focus curve that is like those of the Tecnis Eyhance and AcrySof IQ Vivity IOLs. I typically implant the Light Adjustable Lens bilaterally and space out the cataract procedures by 1 week to allow better coordination of the postoperative refractive adjustments. Both eyes are targeted for emmetropia. Approximately 2 to 3 weeks after surgery on the second eye, the patient returns for a bilateral refraction and determination of the preferred eye for near vision.
Step No. 2: Customization of vision. Trial frames are used to allow patients to evaluate different levels of myopia in the office with reading or other near materials they have brought in for this purpose. Typically, a plano result is targeted for the distance eye, and the refractive target is -0.50 to -0.75 D sphere for the near eye. Because sphere and cylinder can be treated in 0.25 D steps, up to three total refractive adjustments may be made.
The broadening of the depth of focus with the Light Adjustable Lens is symmetric on both the myopic and hyperopic portions of the defocus curve, which can result in additional distance acuity when a myopic target is selected and excellent binocular vision at distance, intermediate, and near with minimal anisometropia. During the adjustment phase of treatment, patients frequently request that the level of myopia in the near eye be adjusted for greater near or distance vision. Occasionally, a patient will request mild myopia in the distance eye as well, which highlights the benefit of being able to customize vision.
CONCLUSION
Many of my practice’s most satisfied patients received the Light Adjustable Lens, and they enjoy a great quality and range of binocular vision.




