In phototherapeutic keratectomy (PTK), an excimer laser is used to treat a variety of corneal disorders such as surface irregularity, epithelial instability, and superficial opacity. Sequential customized therapeutic keratectomy (SCTK) is a recent evolution of PTK. SCTK is a transepithelial, customized, multistepped approach that addresses corneal higher-order aberrations (HOAs).1-4 This article provides an overview of the SCTK procedure and discusses candidate selection, customized ablation planning, and treatment protocols.
BACKGROUND
HOAs cannot be corrected with spectacles or IOLs and are often underestimated or overlooked by ophthalmologists. HOAs such as spherical aberration and secondary astigmatism, however, can reduce contrast sensitivity, and coma and trefoil can reduce visual resolution.2 The only method by which to reduce or eliminate HOAs is a keratectomy procedure.
The main advantage of SCTK is that it treats corneal HOAs while removing a minimal amount of tissue. The procedure reshapes the corneal surface, and it prioritizes the elimination of HOAs over the correction of ametropia. For that reason, refractive errors—myopia, hyperopia, and astigmatism—can increase after SCTK, but cataract surgery with IOL implantation following SCTK can eliminate these remaining lower-order aberrations (LOAs). In an eye that has a highly aberrated cornea, SCTK may eliminate glare and halos caused by HOAs and optimize the precision of preoperative biometry. Even patients with a history of surface or intrastromal photorefractive surgery may be safely treated with SCTK because the procedure removes a minimal amount of tissue from the areas that were not ablated during prior refractive surgery.
The goal of performing SCTK before cataract surgery is to improve outcomes with the latter procedure. SCTK can also increase the pool of candidates for premium IOLs by eliminating HOAs.
INDICATIONS AND CANDIDATE SELECTION
The indications for SCTK include eyes with HOAs caused by corneal pathological conditions such as certain dystrophies and degenerations; recurrent erosions; traumatic, surgical, and postinfection stromal irregularities; opacities; and neovascularization. SCTK can also be used to treat certain complications of refractive surgery, including a decentered treatment, postoperative corneal scars, an overly small optical zone, and interface problems during LASIK.
Topography, tomography, and aberrometry are used to identify candidates for SCTK before cataract surgery. If corneal HOAs are detected and correspond to alterations in the anterior corneal surface, they can be treated only by reshaping the cornea with customized excimer ablation (ie, SCTK) based on the corneal wavefront. Corneal HOAs caused by alterations in the posterior corneal surface are rare and cannot be corrected with SCTK or cataract surgery.
THE SCTK PROCEDURE
Each step of SCTK entails the use of tomography, topography, and aberrometry followed by the execution of a corneal wavefront–guided customized ablation pattern and wet PTK (ie, smoothing) with a tomographic quality check at the end.
Phase No. 1. Corneal imaging is performed, and corneal wavefront–guided customized transepithelial ablation is executed with a pattern derived from the immediate preoperative corneal wavefront measurement. To save corneal tissue, the ablation pattern is planned using constraints that correct only HOAs; it is decoupled from constraints that correct LOAs. Immediately after the transepithelial ablation, wet PTK is performed.
Phase No. 2. New tomographic imaging is acquired intraoperatively after the excimer laser ablation. The intraoperative tomographic scan and aberrometry are used to check the quantity and quality of residual stromal HOAs and evaluate whether residual stromal thickness corresponds with the surgeon’s expectations.
If corneal HOAs are still present or the surgeon is not satisfied with the outcome, a new corneal wavefront–guided customized ablation pattern, derived from the intraoperative corneal wavefront measurement, can be executed immediately, followed by wet PTK. After the second ablation, tomographic imaging is repeated, and the surgeon checks the anterior corneal shape and quality of the procedure.
A single ablation may suffice. If not, the surgeon can repeat the aforementioned steps as necessary to reshape the cornea as desired, provided that the conventional stromal thickness safety limit of 300 µm is respected.1,2,4
PLANNING THE CUSTOMIZED ABLATION PATTERN
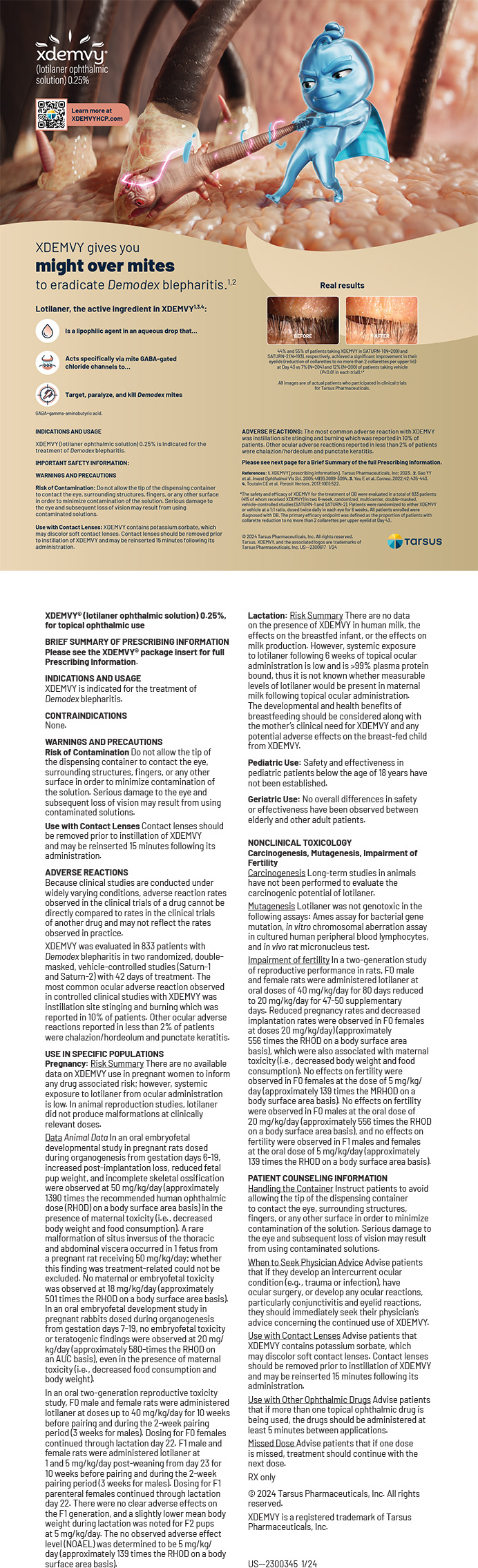
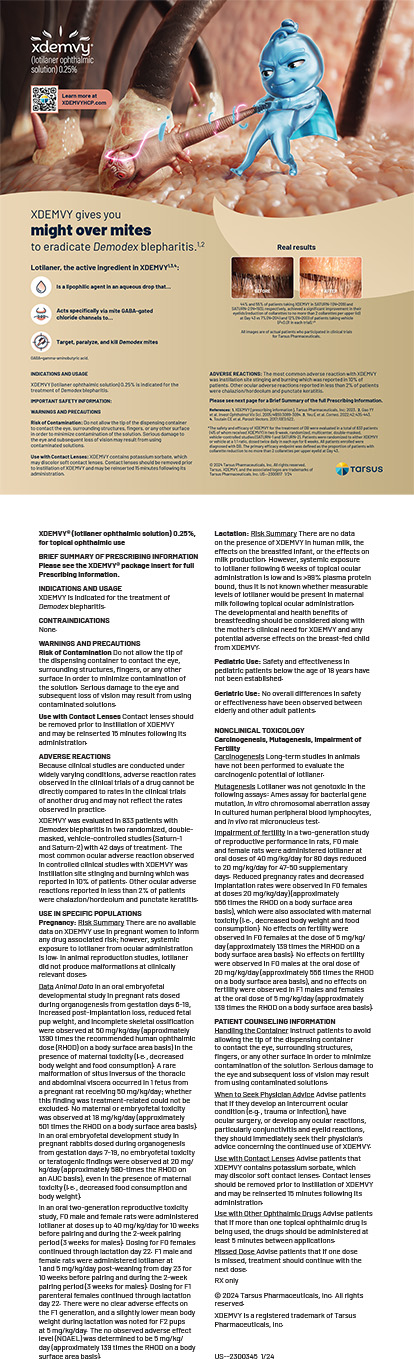
Once a patient’s data are entered (Figure 1), the laser software (Amaris 1050RS, Schwind eye-tech-solutions) automatically displays the ablation pattern calculated to target emmetropia (Figure 2). It must be further customized by the surgeon for SCTK (ie, targeting the selective elimination of the corneal HOAs and not emmetropia).
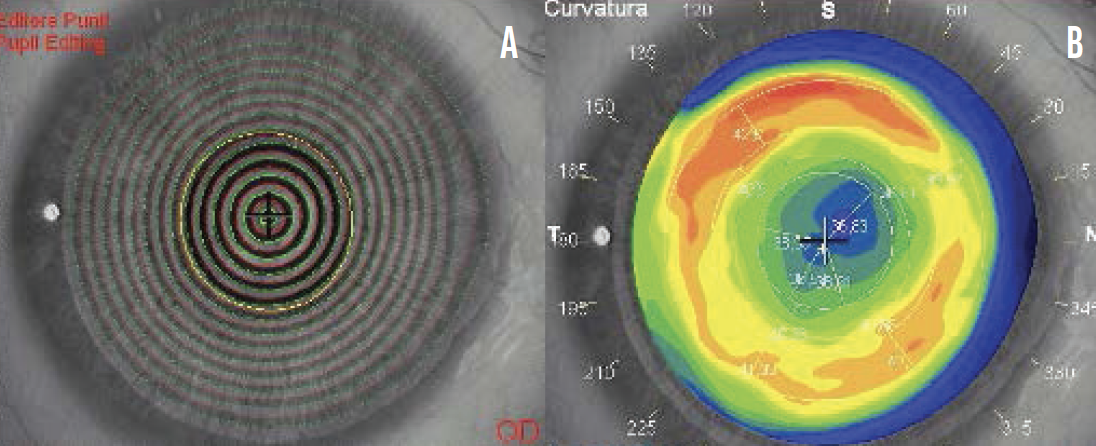
Figure 1. The patient’s data are extrapolated from the topography. The keratoscopy (A) and the tangential map (B) are pictured here. The red ring on the tangential map corresponds to the high dioptric values that typically surrounds a central, slightly decentered, flattened area after myopic correction.
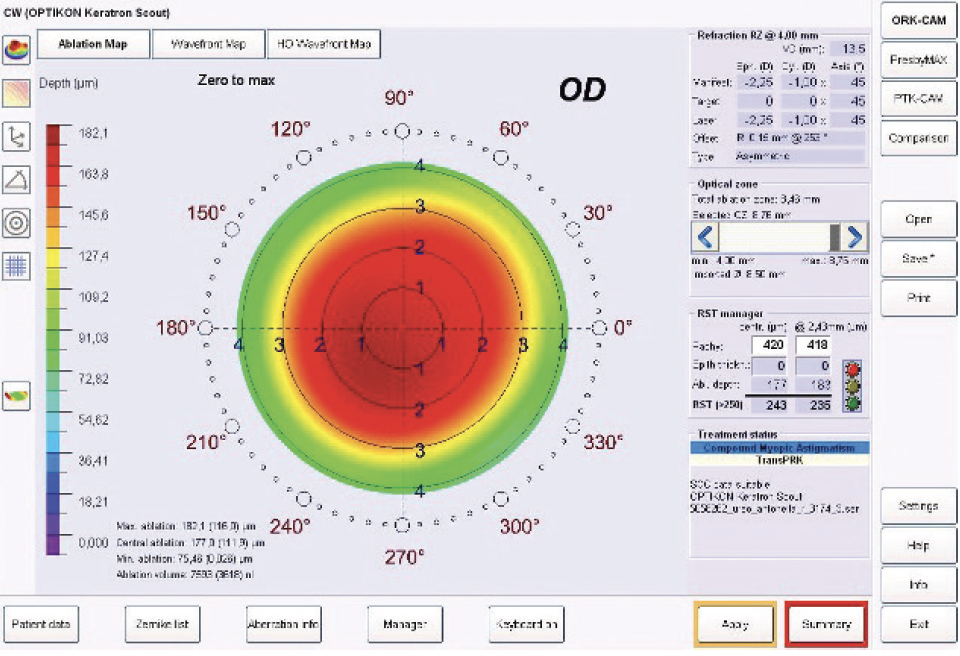
Figure 2. The right eye of a patient who had experienced halos around lights at night and double vision after a myopic photorefractive correction in 2007. The excimer laser main menu and the pattern of ablation that the software calculated targeting emmetropia are depicted here. The pattern will not be executed but will be customized to treat stromal HOAs selectively and independently from the final refractive target, thereby saving corneal tissue.
To eliminate HOAs without considering the final refractive error, treatment is customized using the manager function option. On the refraction display, four constraints (tolerance, sphere, cylinder, and axis) are deselected, and the ablation is minimized by selecting either the depth or volume button (Figure 3). If more of the ablation will occur at the center of the cornea than in the periphery, the pattern should be optimized with the depth option. If most of the ablation will occur at the corneal periphery, volume should be selected.
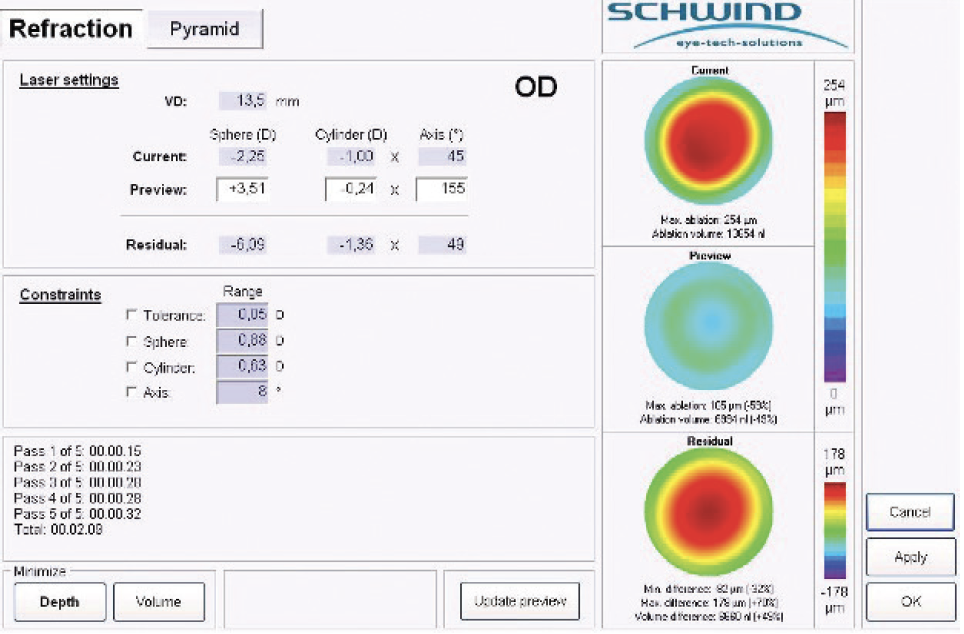
Figure 3. The manager function is selected. Using the refraction module, the four constraints are deselected, and the depth of the ablation is minimized. The previous ablation pattern, which targets emmetropia, is displayed at top right, under current. The new pattern, which is elaborated without constraints and targets selectively HOAs, is shown under preview (center right). The residual pattern at bottom right displays the ablation difference between the aforementioned two patterns. The maximal depth of tissue ablated should be considerably reduced. The predicted final refraction of the patient is calculated at top left of the display, under residual.
The Zernicke pyramid section may be used to minimize the treatment profile further. The surgeon can deselect the treatment of one or multiple HOAs (Figure 4).
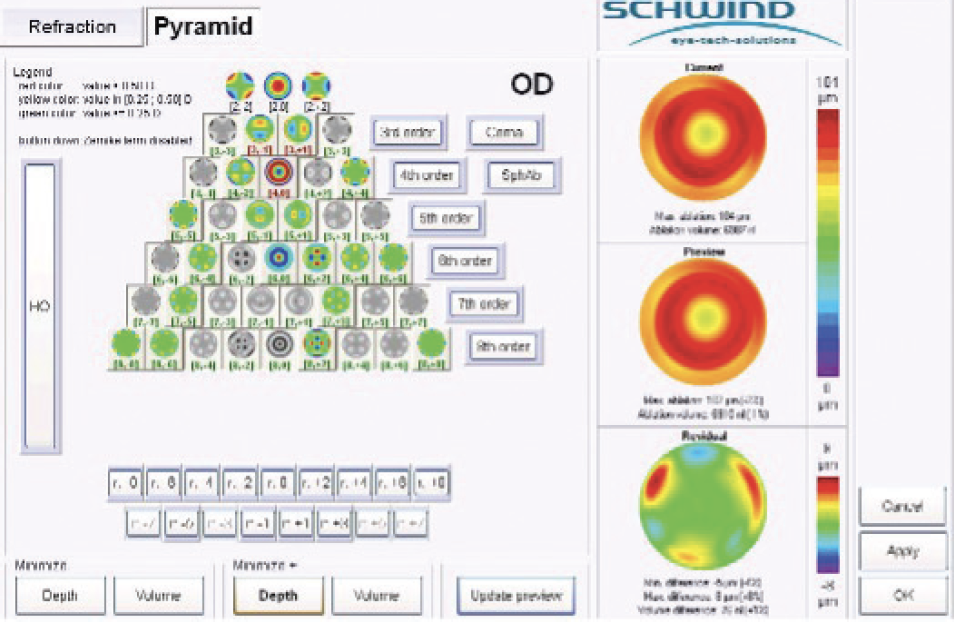
Figure 4. The pyramid module allows further minimization of the ablation pattern, which can be performed with a software calculator, by selecting the depth or volume button or manually by selecting and deselecting specific HOAs that the surgeon would like to treat.
TREATMENT
Oxybuprocaine and lidocaine drops are instilled in the eye before SCTK and during the procedure to reduce patient discomfort. Customized transepithelial ablation is performed, and the ocular surface is irrigated with chilled balanced salt solution. Wet PTK is then performed. The surgeon applies a couple drops of 0.25% hyaluronic acid masking fluid (Femtovisc, Medivis), which has an ablation rate similar to that of stromal tissue, and spreads the fluid over the corneal surface with a Castroviejo spatula while a plano ablation at a depth of 20 μm and a diameter of 10 mm is performed.2,3,5 The planned ablation depth is 20 μm; the presence of the masking fluid, however, reduces the effective ablation depth to around 5 µm.6 This technique has the advantages of regularizing the stromal bed and reducing the risk of haze.
Corrected distance visual acuity is checked, and intraoperative tomography—and eventually topography and aberrometry—is performed. If high-quality measurements are difficult to achieve, the patient can be asked to look down, and a drop of 0.25% hyaluronic acid masking fluid can be instilled on the corneal stroma immediately before topography or tomography to improve the quality of the measurements. This masking fluid has multiple properties, including a superficial tension similar to that of the corneal epithelium. Applying masking fluid to the naked stroma immediately before measurements can simulate the corneal profile after complete reepithelialization.4
If tomography at this point shows that the desired reduction or elimination of HOAs has been achieved, SCTK can be stopped immediately after the first ablation step. The multiple steps of ablation can be repeated if necessary. Once treatment is halted, a sponge soaked in mitomycin C is placed on the corneal surface for 90 seconds. Topical antibiotic drops are instilled, and a bandage contact lens is placed.
The average duration of SCTK is 10 to 20 minutes, but it can take an hour in extreme cases. Patients receive antibiotic eye drops four times a day for a week and are monitored daily until epithelial healing is complete and the bandage contact lens is removed.
An ophthalmologic examination, topography, tomography, and anterior segment OCT are performed 1 month after SCTK. At this point, the patient undergoes a preoperative assessment for cataract surgery, including axial length measurements, keratometry, and IOL power calculation. Cataract surgery and IOL implantation are the final phase.
CONCLUSION
Today, customized procedures for each patient are the norm, and standards for successful cataract surgery are high, even when patients have corneal postrefractive surgery complications, leukomas, and dystrophies. The goal with SCTK is to improve quality of vision by eliminating stromal HOAs and reshaping the corneal profile to a more physiologic and prolate condition while preserving corneal biomechanics.7-9 Residual LOAs can be corrected secondarily with subsequent IOL implantation.
Performing SCTK before cataract surgery on eyes with highly aberrated corneas can dramatically improve postoperative quality of vision and help patients to achieve the best visual acuity with the desired refractive target while eliminating optical aberrations.
1. Vinciguerra P, Vinciguerra R, Randleman JB, Torres I, Morenghi E, Camesasca FI. Sequential customized therapeutic keratectomy for Reis-Bücklers’ corneal dystrophy: long-term follow-up. J Refract Surg. 2018;34(10):682-688.
2. Vinciguerra P, Camesasca FI. Custom phototherapeutic keratectomy with intraoperative topography. J Refract Surg. 2004;20(5):S555-S563.
3. Vinciguerra P, Camesasca FI. One-year follow-up of custom phototherapeutic keratectomy. J Refract Surg. 2004;20(5 suppl):S705-S710.
4. Vinciguerra P, Camesasca FI, Morenghi E, et al. Corneal apical scar after hyperopic excimer laser refractive surgery: long-term follow-up of treatment with sequential customized therapeutic keratectomy. J Refract Surg. 2018;34(2):113-120.
5. Vinciguerra P, Camesasca FI, Torres IM. Transition zone design and smoothing in custom laser-assisted subepithelial keratectomy. J Cataract Refract Surg. 2005;31(1):39-47.
6. Huang D, Tang M, Shekhar R. Mathematical model of corneal surface smoothing after laser refractive surgery. Am J Ophthalmol. 2003;135(3):267-278.
7. Vinciguerra P, Albè E, Camesasca FI, Trazza S, Epstein D. Wavefront- versus topography-guided customized ablations with the Nidek EC-5000 CX II in surface ablation treatment: refractive and aberrometric outcomes. J Refract Surg. 2007;23(9 suppl):S1029-S1036.
8. Vinciguerra P, Munoz MIT, Camesasca FI, Grizzi F, Roberts C. Long-term follow-up of ultrathin corneas after surface retreatment with phototherapeutic keratectomy. J Cataract Refract Surg. 2005;31(1):82-87.
9. Roberts C. The cornea is not a piece of plastic. J Refract Surg. 2000;16(4):407-413.