CASE PRESENTATION
A 58-year-old woman presents for a consultation. The patient reports that she has experienced 3 months of blurry vision in the left eye following a fall with no head trauma. Ten years ago, the left eye underwent scleral fixation of a PMMA IOL (CZ70BD, Alcon) with 10-0 polypropylene (Prolene, Ethicon) sutures and a pupilloplasty. The patient also underwent a pars plana vitrectomy many years ago for a retinal detachment.
On examination, her BCVA is 20/40 OS. The lids and lashes are normal. The ends of a 10-0 polypropylene suture are seen to be buried under the conjunctiva superiorly and inferiorly. The cornea is clear, and the anterior chamber is deep and quiet. The superotemporal pupilloplasty suture is intact, and temporal transillumination defects are visible. The examination findings are consistent with a temporally subluxated IOL due to the release of the inferior polypropylene suture from the inferior haptic. When the patient is supine, the view of the IOL is lost with posterior hinging owing to a release of inferior fixation (Figure 1). The retinal examination is normal with 360º laser scars from prior surgery.
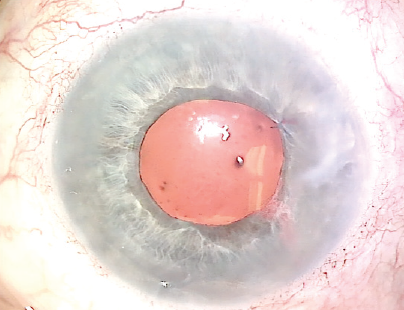
Figure 1. Preoperative appearance of the left eye while the patient is supine. Note the lack of visibility of the IOL and the superotemporal iris suture.
How would you address the dislocated IOL?
—Case prepared by Brandon D. Ayres, MD, and Ashley Khalili, MD

SOON-PHAIK CHEE, FRCS(G), FRCS(ED), MMED(S’PORE)
The options here are resuturing the inferior haptic to the sclera with a stronger suture through the eyelet (technically difficult) or securing the haptic with a belt loop (PTFE [off-label use] or flanged polypropylene). The existing suture, however, is likely to give way during surgery, risking a dropped IOL in this vitrectomized eye. My preference, therefore, would be to perform an IOL exchange and intrascleral haptic fixation and to use the Yamane1 instead of a glued IOL technique.
Under peribulbar anesthesia, the 6 and 12 clock positions at the limbus and 2 mm posteriorly on the conjunctiva would be marked. With anterior chamber infusion running, paracenteses would be created on either side of the sutured haptic and at the 1 and 4:30 clock positions. The pupilloplasty suture would be released. With iris hooks exposing the attached haptic, the sclera would be depressed, bringing the suture into view. The haptic would be grasped with intraocular forceps, and a 27-gauge needle would be used to nick the suture. The IOL would be brought into the anterior chamber and explanted.
After removal of the iris hooks, a superior peripheral iridectomy would be created. A three-piece, round anterior–edged IOL would be inserted into the anterior chamber under a dispersive OVD. The incision would be sutured. Starting 2 mm counterclockwise to the scleral fixation marks, bent 27-gauge needles on insulin syringes filled with balanced salt solution would be made to traverse the sclera and enter the eye at the fixation marks. Beginning with the trailing haptic, the haptics would be threaded into the needle. The haptics would be retrieved, flanged, and buried after IOL centration is confirmed. A four-throw pupilloplasty would be performed using 10-0 polypropylene. The OVD would be removed, infusion halted, and the incisions hydrated.

ZEBA A. SYED, MD
One technique that I find useful in this scenario is a modification of the approach first described by Canabrava and colleagues.2 This particular case offers two unique considerations. First, initial IOL fixation was with a 10-0 polypropylene suture, which is at risk of degradation years later. Second, the patient has a history of pars plana vitrectomy, obviating the need for concurrent vitrectomy at the time of haptic fixation.
To start this case, a single pars plana port would be placed, and a paracentesis would be created for an anterior chamber maintainer. To retrieve the existing IOL, an OVD cannula would be inserted through the pars plana to elevate the IOL and rest it on the iris. After the creation of an adjacent paracentesis, the haptic of the CZ70BD would be externalized, and a 5-0 polypropylene suture would be threaded through the eyelet. Low-temperature cautery would be used to make a flange at the suture’s tail, posterior to the IOL. The externalized haptic can then be returned into the anterior chamber. Next, a 27-gauge needle would be inserted 2.5 mm posterior to the inferior limbus, and intraocular forceps (MicroSurgical Technology) would be used to thread the free end of the 5-0 polypropylene suture into the lumen. Once the needle is externalized, the suture can be shortened to center the IOL and cauterized to create a flange that remains subconjunctival.
It is important to recognize that the superior 10-0 polypropylene suture is at similar risk of future disinsertion. I would therefore consider refixating that haptic using the same approach.


WHAT WE DID: BRANDON D. AYRES, MD, AND ASHLEY KHALILI, MD
Surgical options for this patient are an IOL exchange or refixation of the current lens. An important point of consideration is the need for a large wound, approximately 6 to 7 mm, if the PMMA IOL is to be removed and replaced. Additionally, the pupilloplasty suture may limit full dilation of the pupil and may have to be replaced to improve visualization during surgery.
The risks, benefits, and alternatives to surgery were discussed extensively with the patient, and she elected to undergo IOL refixation. To avoid the need for a large corneal wound, a surgical plan was made to refixate the haptics using a PTFE suture (Gore-Tex CV-8, W.L. Gore & Associates; off-label use). The patient was also made aware of the plan for a pupilloplasty as needed.
A peritomy was created inferiorly, and a centration mark was made 3 mm posterior to the limbus with a marking pen. Two circumlimbal sclerotomies were made 4 mm apart and centered over the 3-mm centration mark. With a Charles lens used for posterior visualization, the inferior haptic was grasped with microforceps, and the haptic was elevated into the anterior chamber. The haptic was then externalized through an inferior paracentesis, and a CV-8 PTFE suture strand was laced through the externalized haptic eyelet (Figure 2). The haptic was then rotated back into the eye, and the suture ends were each externalized through the sclerotomies with microforceps using a handshake technique (Figure 3). The superior haptic was released from polypropylene fixation and fixated with a PTFE suture using the same technique (Figure 4). Iris hooks were placed superiorly to improve visualization and avoid the need to replace the pupilloplasty sutures.
One day after surgery, the patient's visual acuity was 20/80 OS. The cornea had mild peripheral edema, and the anterior chamber was deep with mild cell. The PTFE suture was well covered superiorly and inferiorly by conjunctiva. The IOL was in position and well centered (Figure 5).
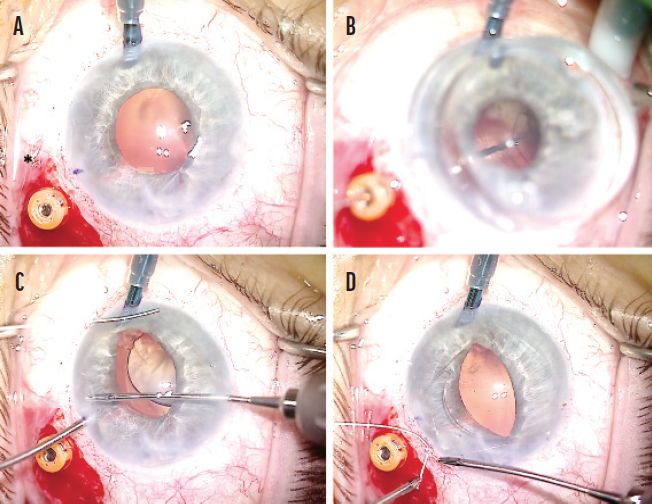
Figure 2. Retrieval of the released inferior haptic of the CZ70BD lens. An anterior chamber maintainer is placed nasally. A trocar and a sclerotomy (indicated with an *) are placed 3 mm posterior to the limbus and 4 mm apart in a circumlimbal fashion after a peritomy is created (A). With posterior visualization using a Charles lens, the inferior haptic is grasped with a pair of microholders (B). The haptic is elevated into the anterior chamber and then externalized through an inferior paracentesis (C). A CV-8 PTFE suture strand is laced through the externalized haptic eyelet (D).
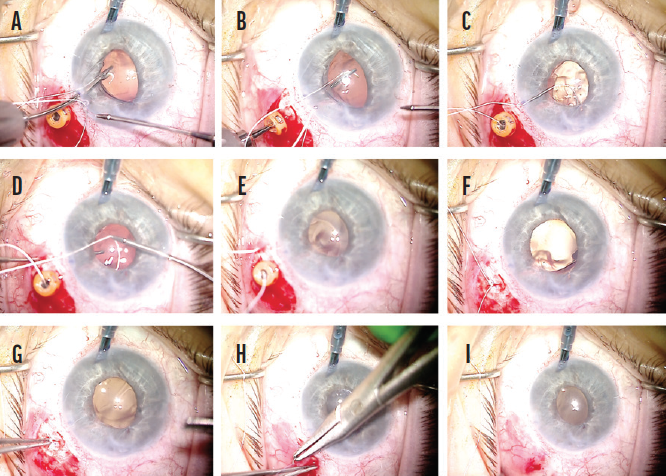
Figure 3. Scleral fixation with a CV-8 PTFE suture using a handshake technique. The suture strand is brought into the anterior chamber with microforceps via the inferior paracentesis (A). The suture end is grasped behind the optic by forceps introduced through the trocar (B) and then externalized (C). Next, the other end of the suture is introduced into the anterior chamber and passed from superior limbal approaching forceps to microforceps placed in the distal sclerotomy (D). With removal of the microforceps, the suture end is externalized through the sclera (E). The trocar is removed, and the suture ends are tied (F). The knot is buried into the sclerotomy (G). The peritomy is closed (H and I).
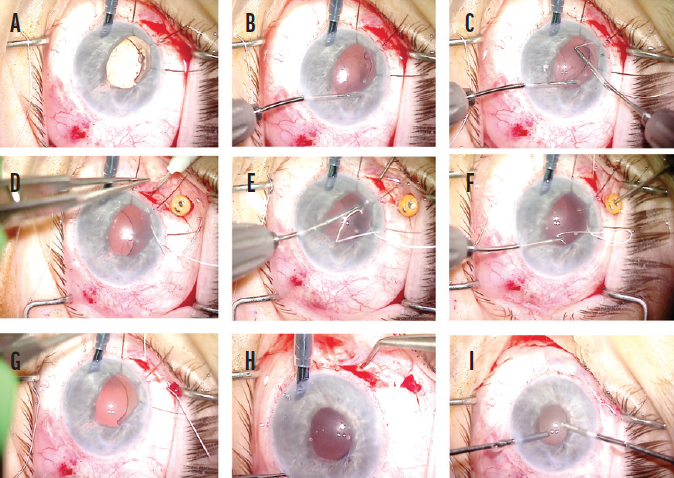
Figure 4. Refixation of the superior haptic. Iris hooks are placed to improve visualization (A). The superior haptic is released from the polypropylene suture (B). A PTFE suture is introduced into the anterior chamber via a superior paracentesis and laced through the eyelet (C). A peritomy is created, and two sclerotomies are created 4 mm apart in a circumlimbal direction and centered over a centration mark located 3 mm posterior to the limbus (D). One end of the suture is handed off through the anterior chamber from one microforceps to another, which was introduced through the sclerotomy (E). The suture is then externalized through the scleral incision using the microforceps. The same steps are repeated for the other suture end via the proximal trocar (F). The trocar is removed, and the knot is tied and buried (G). The iris hooks are removed, and the peritomy is closed (H). The anterior chamber is cleared of OVD (I).
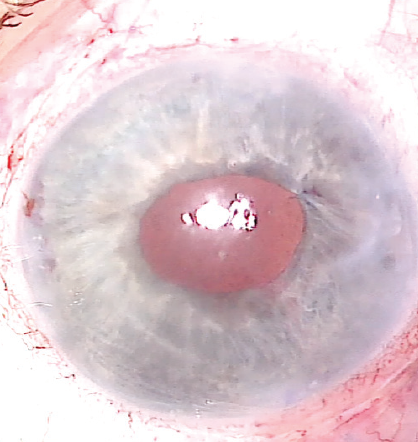
Figure 5. After surgery, the IOL is in position and exhibits good centration and no tilt.
Figures 2 through 5 courtesy of Brandon D. Ayres, MD
The patient began a postoperative regimen of topical steroids and antibiotics. One month after surgery, the patient reported an improvement in her vision. Her visual acuity was 20/40, the corneal edema had resolved, and the IOL was stable.
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
2. Canabrava S, Canêdo Domingos Lima AC, Ribeiro G. Four-flanged intrascleral intraocular lens fixation technique: no flaps, no knots, no glue. Cornea. 2020;39(4):527-528.




