Light adjustable lens technology has been available in Europe for more than a decade, in the form of an IOL first known as the Light Adjustable Lens (LAL, Calhoun Vision) and now as the RxLAL (RxSight). The RxLAL and its associated Light Delivery Device (LDD, RxSight) were approved by the FDA in 2017 and obtained the CE Mark in Europe in 2010. In our experience with the lens, the precision of its optics is impressive.
Our patients have appreciated the extra effort and customizability it provides. The practical process shares some similarities with the typical cataract journey, although there are some differences that must be discussed with patients prior to surgery. When this discussion is framed appropriately, it can promote patient compliance and enhance the patient experience.
PATIENT DISCUSSION
Managing patient expectations is important in any cataract surgery procedure, but especially with the RxLAL. Patients must be aware that they are required to wear the UV-protection glasses we provide during all waking hours until 24 hours after their last lock-in procedure. For most patients, this represents about 4 weeks. Interestingly, patient acceptance of the UV-protection glasses is very high, and several patients have even customized their glasses with rhinestones!
Upon initial lens stabilization, which occurs about 2 to 3 weeks after surgery, the first lens adjustment can be performed to change the spherical or spherocylindrical power of the lens. Most patients undergo one to three adjustments and one or two lock-ins, with a minimum of 48 hours between treatments. The absolute minimum, as calculated by the cumulative light dose of the LDD, is one adjustment and one lock-in (see Watch It Now), and the average number of total treatments is approximately three per eye.
Dr. Walton performs a lock-in procedure with the Light Delivery Device.
CONSIDERATIONS IN PATIENT SELECTION
As with any technology, selecting appropriate patients for the RxLAL is crucial. The first consideration is pupil size. Postoperatively, the pupil must be able to dilate to at least 6 mm for each adjustment and lock-in procedure. We therefore recommend a minimum preoperative pupil size of 7 mm, as postoperative dilation can be limited by inflammation or dilator muscle fatigue after multiple dilations. For patients taking an alpha blocker and for those who dilate slowly, it is appropriate to counsel them preoperatively that their adjustment and lock-in visits will take longer than average because of the time needed to reach appropriate dilation.
The RxLAL has a UV filter in the posterior aspect of the optic, but even with this precaution in place there are some cautions to consider regarding using the lens in patients with significantly compromised maculas or those taking any photosensitizing medications. Most of these concerns are theoretical, but we recommend caution.
The most common medication we encounter that requires caution is hydrochlorothiazide. For patients taking this or other photosensitizing medication, our practice obtains preoperative clearance from the prescribing physician to stop the drug from seven doses before the first adjustment until beyond the final lock-in. The medication does not need to be stopped before surgery.
In the United States, the LDD is approved for postoperative adjustment of 0.75 to 2.00 D of cylinder and 2.00 D of sphere. In Europe, it has a CE Mark for adjustment of up to 3.00 D of cylinder. An ongoing US clinical study will determine if correction as low as 0.50 D, instead of 0.75 D, of astigmatism is safely feasible.
Most surgeons have encountered astigmatic patients whose powers or axes vary on different measurements, and we all know that surgical planning for a toric IOL can be somewhat of a guessing game. In the FDA trials, the RxLAL outperformed toric IOLs.1
Further, we must remember that an underlying issue in astigmatic correction is the health of the ocular surface. The same eyes that have varying topographies preoperatively can have varying refractions postoperatively. As a result, patients should be counseled that an RxLAL lens can help them to obtain the best vision that their eyes can achieve.
Because light adjustment treatments can last up to 2 minutes and require good fixation and stillness, patients who cannot position well at the slit lamp or remain stable may have a difficult time at the LDD. Pay special attention to patients who cannot breathe without significant movement.
CHOOSING LENS POWER
Lens power selection with the RxLAL is just like with any other IOL. We currently use the Barrett Universal II and Barrett True-K formulas. A more important consideration is choosing postoperative refractive targets. Evidence suggests that 20% to 31% of patients switch ocular dominance or distance preference after cataract surgery.2,3 Some surgeons advocate targeting both eyes for distance at implantation. In our experience, however, patients can become frustrated with having no near vision. Bifocal UV-blocking glasses are available from the company and can be helpful in the postoperative period.
Our general advice is to target distance in the patient’s distance-preferred eye and about half of the anticipated postoperative myopia in the patient’s near-preferred eye. For example, if we think someone needs a plano result in the right eye and -1.50 D in the left, we would choose an IOL targeting distance in the right eye and -0.75 D in the left. That patient will then be functional in the immediate postoperative period and can easily have either eye adjusted thereafter.
We are participating in an ongoing study looking at incorporating an extended depth of focus treatment in the RxLAL. The results of this study may affect our IOL power selection decisions, potentially leading to using a more distance-dominant target with extended depth of focus treatment applied to one or both eyes.
SURGERY DAY AND POSTOPERATIVE CARE
The surgery itself is straightforward. The three-piece monofocal lens unfolds rapidly in the eye and does not require marking or alignment. The lens can be placed in the bag or the sulcus. Two goals in surgery are minimizing iris trauma, because the iris must be able to dilate well postoperatively, and avoiding the need for a corneal suture. If a suture is needed, consider removing it when safe and allowing the cornea to stabilize for a few weeks before adjusting and locking in the lens. Patients must leave the OR with UV-protecting glasses on and strict instructions for compliance with UV protection.
We typically treat or lock-in both eyes on the same day. Once the eyes are stable after surgery, the discussion is similar to before LASIK. Refract the patient, consider using trial frames to let the patient reevaluate vision goals, and then start the dilation process. Most patients need multiple sets of dilation drops. We have found that, for most patients, 48 hours between adjustments and lock-ins is too soon for optimal dilation, probably due to dilator muscle exhaustion. Consider using a pledget soaked in a mixture of phenylephrine and tropicamide. Cyclopentolate is another option.
Many refractive practices have a specialized refractionist or optometrist perform the measurements and lead the targeting discussion. Regardless of whether the surgeon or someone else is measuring and discussing, anticipate a moderate amount of chair time. We have found that most of our patients end up wanting to change their target by small amounts. For example, some patients find that -2.00 D is too near, and they settle on -1.50 D at the second adjustment. Ultimately, the target spherocylindrical refraction is entered into the LDD, and the computations are handled by the device.
Because adjustment and lock-in visits typically start around the 3-week postoperative time frame, they often are scheduled in addition to—rather than corresponding with—the routine postoperative visits. We advise anticipating changes to the clinic template to accommodate these visits.
After verifying the patient and lens and entering the refraction and target, the treatment is as simple as having the patient stare at a green fixation light and using a specialized handheld contact lens, similar to a YAG laser lens. Ring lights are used to ensure appropriate tilt of the lens, and then a red reticle is visible through the oculars of the device (Figures 1–4). The red reticle is aligned to the IOL edges, and the passive tracking system is engaged. When poor alignment is detected, an audible beep sounds as a prompt to realign.
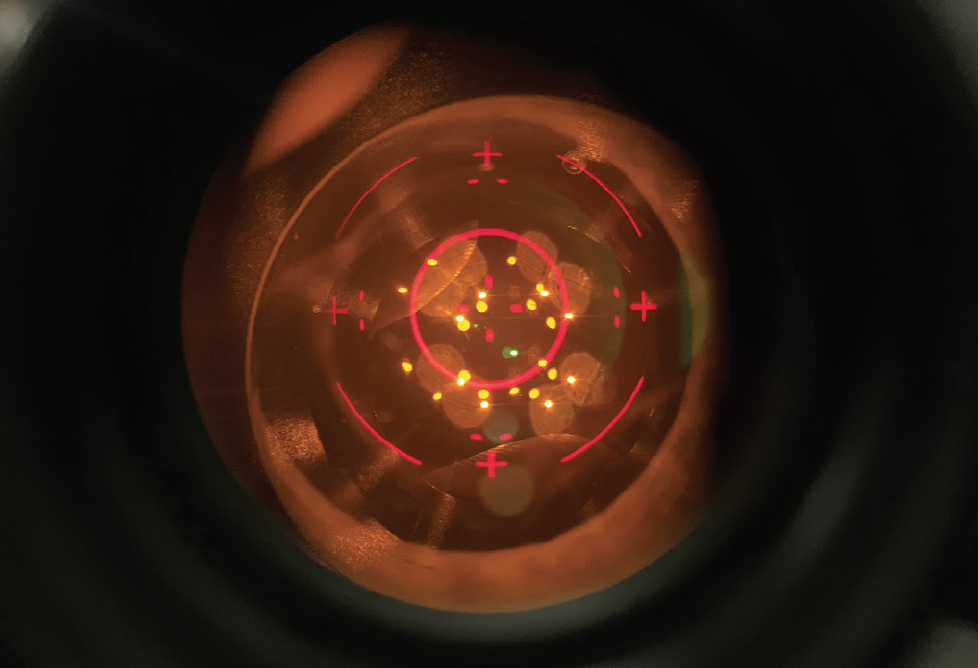
Figure 1. View through the oculars before a treatment. The aiming reticle is centered on the lens. The white and yellow reflections are Purkinje images from the illuminating ring. A bubble in the coupling gel is visible at the 1 clock hour, but can be easy to overlook.
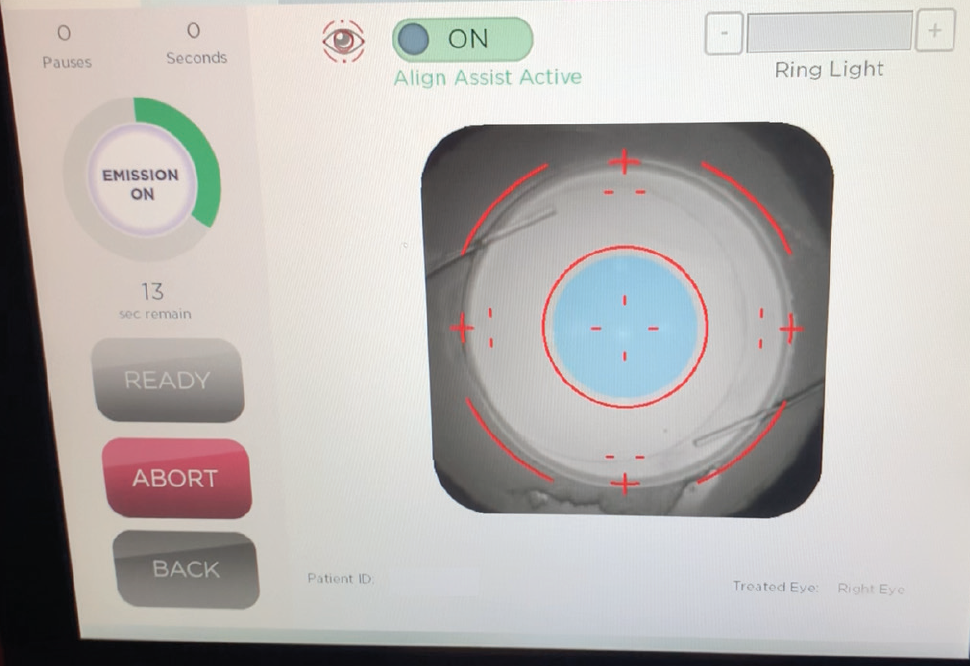
Figure 2. Screen view during a treatment with good dilation and centration. The infrared view shows an overlay of the aiming reticle. The blue circle represents the center of the IOL as detected by the LDD software’s passive Align Assist alert feature.
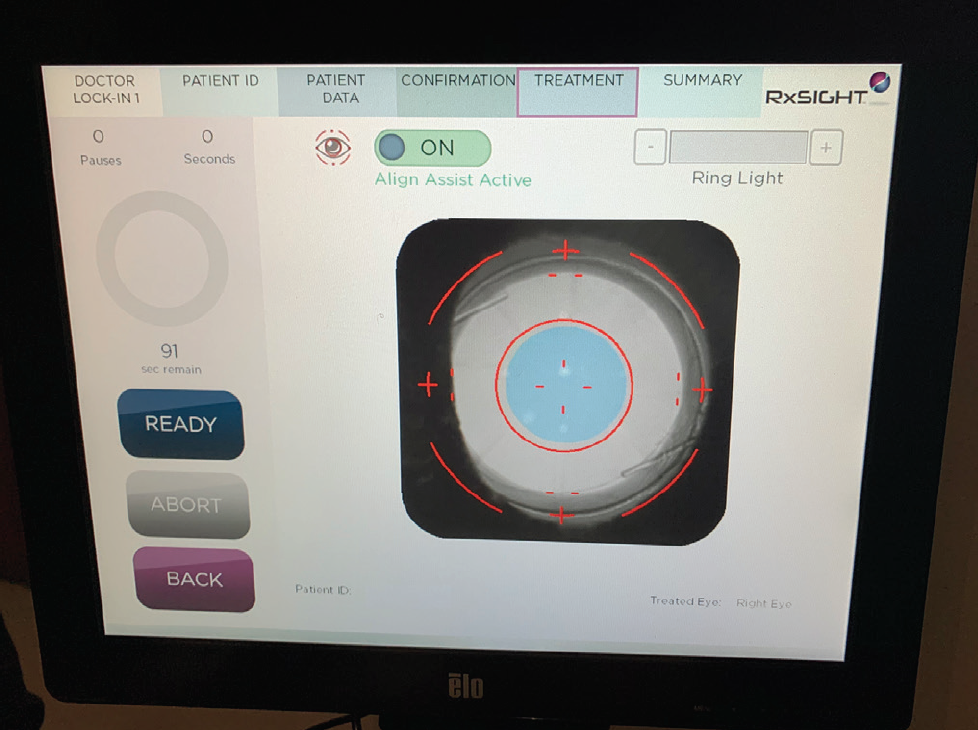
Figure 3. Screen view of an RK patient focusing on the lens. Note that, even with good dilation, care has be taken to expose the whole IOL.
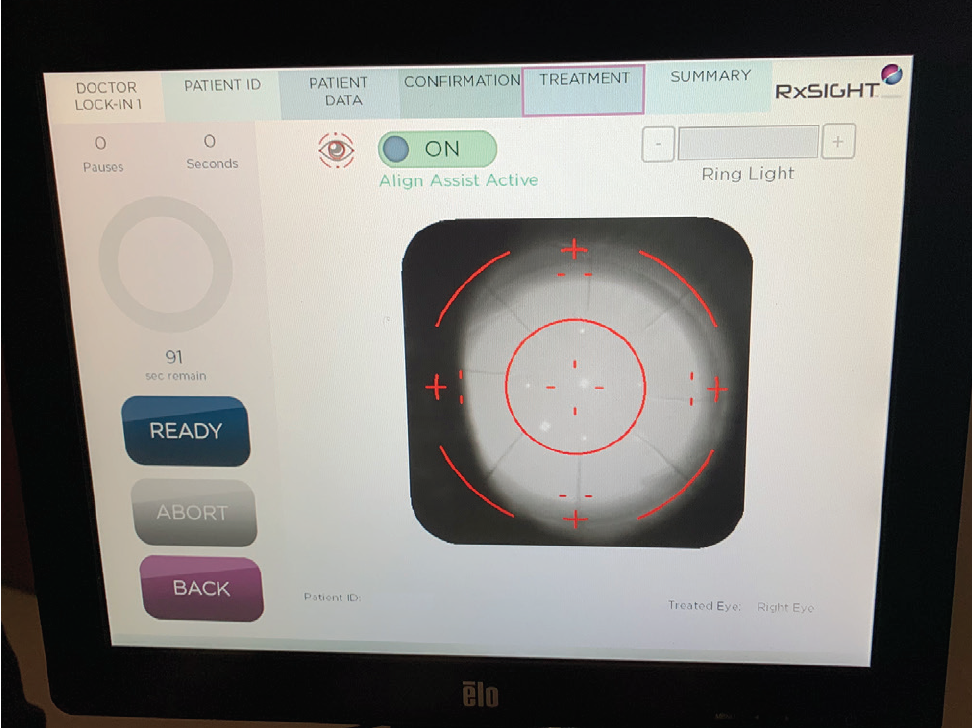
Figure 4. The same patient as Figure 3: The infrared on-screen image is focused on the RK incisions.
The patient sees a bright blue light, also visible to the surgeon through the oculars as a blue glow over the part of the IOL we are attempting to swell. For example, to steepen the lens and increase its power, we expose the central lens to the light to polymerize the macromers dissolved in that area. As those macromers are removed from solution, the new diffusion gradient brings new macromers centrally as they redistribute, resulting in central swelling.
CONCLUSION
The RxLAL is a great new option for patients and surgeons. We have found that appropriate patient screening and expectation management, clinical flow optimization, and thoughtful use of the adjustability are keys to success.
1. Data on file with RxSight and Alcon.
2. Lee M, Shin KL. Clinical study of changes in eye dominance after pseudophakic conventional monovision. J Korean Ophthalmol Soc. 2019;60(6):534-540.
3. Schwartz R, Yatziv Y. The effect of cataract surgery on ocular dominance. Clin Ophthalmol. 2015:9;2329-2333.