Keratoconus is a fairly common corneal disorder that demonstrates progressive thinning and steepening of the central or paracentral cornea, leading to irregular astigmatism.
Keratoconus is usually bilateral and often asymmetric. The condition typically becomes apparent in early adolescence (Figure 1) and may progress until the patient is in his or her early 40s. The condition may appear earlier or later in life, and the rate of progression is variable. The hereditary pattern is often unpredictable, but positive family histories have been reported. The incidence of keratoconus is often reported to be one in 2,000 people.1
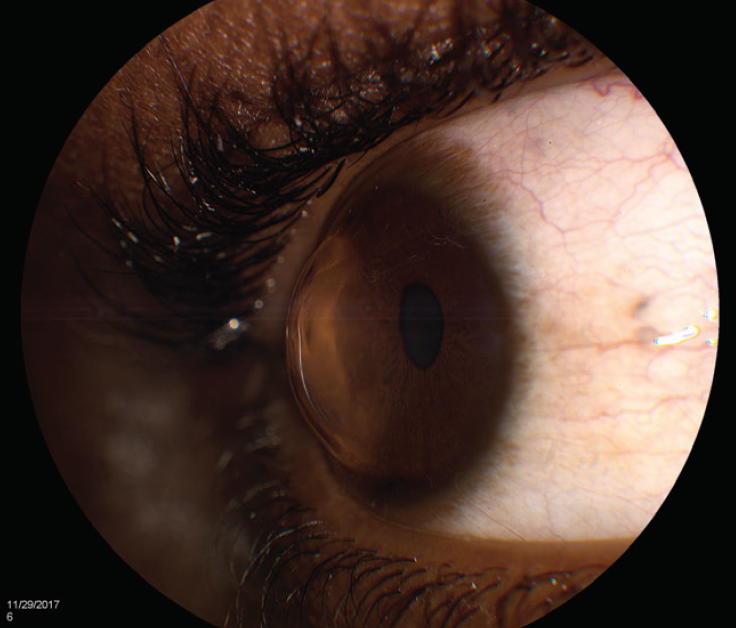
Figure 1. Keratoconus in a young patient requiring CXL.
TREATING KERATOCONUS
Patients with mild keratoconus may benefit from the use of eyeglasses, whereas those with more significant astigmatism warrant the use of rigid contact lenses.
The primary treatment for progressive keratoconus is CXL, in which riboflavin and UV light are applied to induce hardening of the weak and flaccid keratoconic cornea to slow progression.
CHALLENGES WITH CATARACTS
Challenges for surgeons performing cataract surgery in a keratoconic eye are significant due to the topographic irregularity. Recent research has shown that a fair amount of astigmatism is due to the posterior surface of the cornea and, in many cases, mild or forme fruste keratoconus.2
Keratoconus presentation is widely variable, but it is always manifested by a thinned area with varying degrees of regular or highly irregular astigmatism. The normal anterior cornea and the posterior cornea can be thought of as two stacked bowls that don’t nest exactly smoothly. In keratoconic eyes, the bowls may be of varying shapes and sizes.
We now have multiple technologies for measuring posterior corneal curvature, including slit-scan imaging, Scheimpflug imaging, OCT, devices that use reflective imaging (»Cassini; iOptics), swept-source OCT, and improved software for Scheimpflug images (»Pentacam; Oculus Optikgeräte).
Cataract surgery is now a refractive procedure, and patients have high expectations for good UCVA after surgery. Patients with keratoconus who have been successful in achieving good quality BCVA with rigid or scleral contact lenses often expect cataract surgery to yield similar outcomes, despite the fact that they present considerably greater challenges to their surgeons.
AT A GLANCE
- Many surgeons shy away from recommending premium lenses for patients with keratoconus, but, under the right circumstances, cataract surgery with a toric IOL can greatly improve UCVA in a keratoconic eye.
- Choosing the right candidates for this procedure is crucial.
- The author has implanted toric IOLs in many patients with stable mild or forme fruste keratoconus; postoperatively, in 80% of cases, patients see well enough that they do not require contact lenses.
TALKING TORICS
Patients with mild ectasia and an identifiable major axis of astigmatism may benefit from a toric IOL, in that it could allow them to be free of contact lens use postoperatively. But surgeons have generally shied away from recommending premium lens technologies for patients with keratoconus. The prevailing attitude has been that toric IOLs and other premium technologies should not be offered to patients with ocular pathologies that could limit their visual potential. Under the right circumstances, however, cataract surgery with a toric IOL can greatly improve UCVA in a keratoconic eye, even approaching the patient’s previous level of corrected visual function.
As patients age, contact lenses can become more difficult to tolerate, and, as LASIK is not an option in keratoconic eyes, toric IOLs may fill the gap to optimize visual outcomes.
I have implanted toric IOLs in many patients with stable mild or forme fruste keratoconus to reduce astigmatism and improve UCVA postoperatively. In 80% of these cases, the patients now see well enough that they do not require contact lenses. This group includes one patient with 20/20 UCVA, but most are in the 20/30 to 20/40 range, meaning that they retain functional vision without contact lens use. These patients report a significant improvement in their quality of life (unpublished data).
SUCCESS STORIES
Case No. 1
A 63-year-old man with bilateral keratoconus was referred to me for cataract evaluation due to poor visual acuity. His ophthalmic history was significant for a branch retinal artery occlusion in the right eye. Ocular examination revealed 2+ nuclear sclerotic cataracts and a partial Fleischer ring. The fundus examination was unremarkable except for attenuated arterioles.
The patient’s refraction was -2.25 +3.00 X 10º OD with BCVA of 20/100 and -2.00 +2.00 X 15º OS with BCVA of 20/40. Due to the limited visual potential of the right eye, surgery with a toric IOL was contemplated for the left eye only.
In the patient’s left eye, »IOLMaster (Carl Zeiss Meditec) keratometry (K) readings were 44.23 D @ 96° and 47.07 D @ 6°, with 2.84 D of cylinder at 6°. This matched up fairly well with Pentacam (Oculus Optikgeräte) K readings (Figure 1). Topography showed a relatively mild inferotemporal cone. I explained to the patient that astigmatism secondary to keratoconus is usually irregular and that it may not be completely corrected by a toric IOL. I explained that he might still require glasses or contact lenses to achieve optimal BCVA.
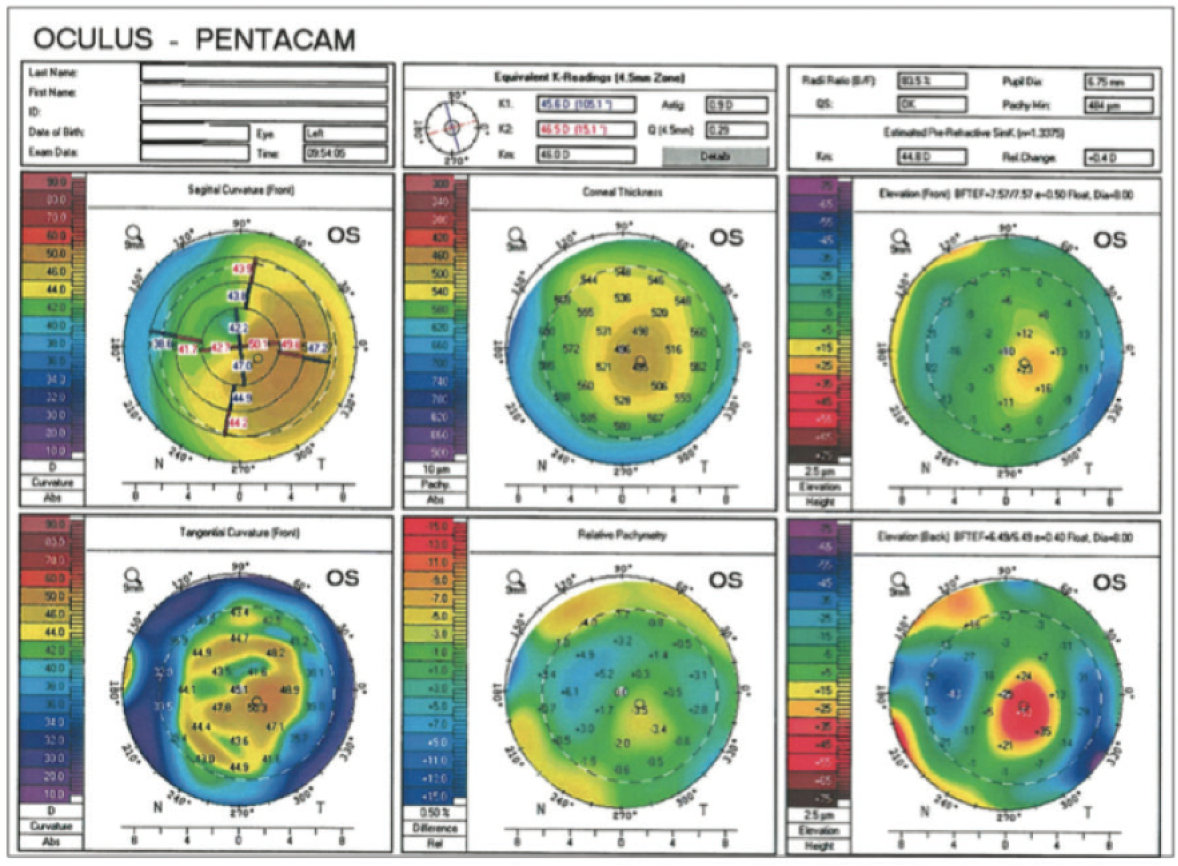
Figure 1. In the left eye of a patient with a mild inferotemporal cone, keratometry readings on IOLMaster, refraction, and Pentacam Comprehensive Eye Scanner all agreed on the axis of astigmatism.
After consulting the Johnson & Johnson Vision toric calculator, I implanted the company’s ZCT300 »Tecnis Toric IOL. Postoperatively, the patient was pleased with the outcome. At the 3-month postoperative visit, his UCVA was 20/25 with a refraction of -0.25 +0.25 X 105º.
Case No. 2
A 64-year-old man was referred for cataract surgery after complaining of experiencing severe glare when driving, particularly at dusk or dawn. His BCVA was 20/200 OD and 20/60 OS. His refractions were -4.25 +2.25 X 67º OD and -3.50 +2.75 X 13º OS. Brightness acuity testing showed glare sensitivity of 20/400 in each eye. He had 2+ nuclear sclerotic cataracts with posterior subcapsular changes and mild scattered macular drusen.
I discussed with the patient elective cataract surgery with a toric IOL and the limitations of this approach. Because there was apical scarring in his right eye, we decided to use a toric IOL only in the left.
Pentacam K readings at the 4.5-mm optical zone disclosed 2.50 D of cylinder at 74° with an inferior cone that demonstrated a fairly regular pattern of astigmatism (Figure 2). This finding correlated well with the IOLMaster Ks of 44.58 D @ 164° and 46.75 D @ 74° for a total cylinder reading of 2.17 D @ 75°. The Alcon Toric calculator suggested the company’s SN6 lens.
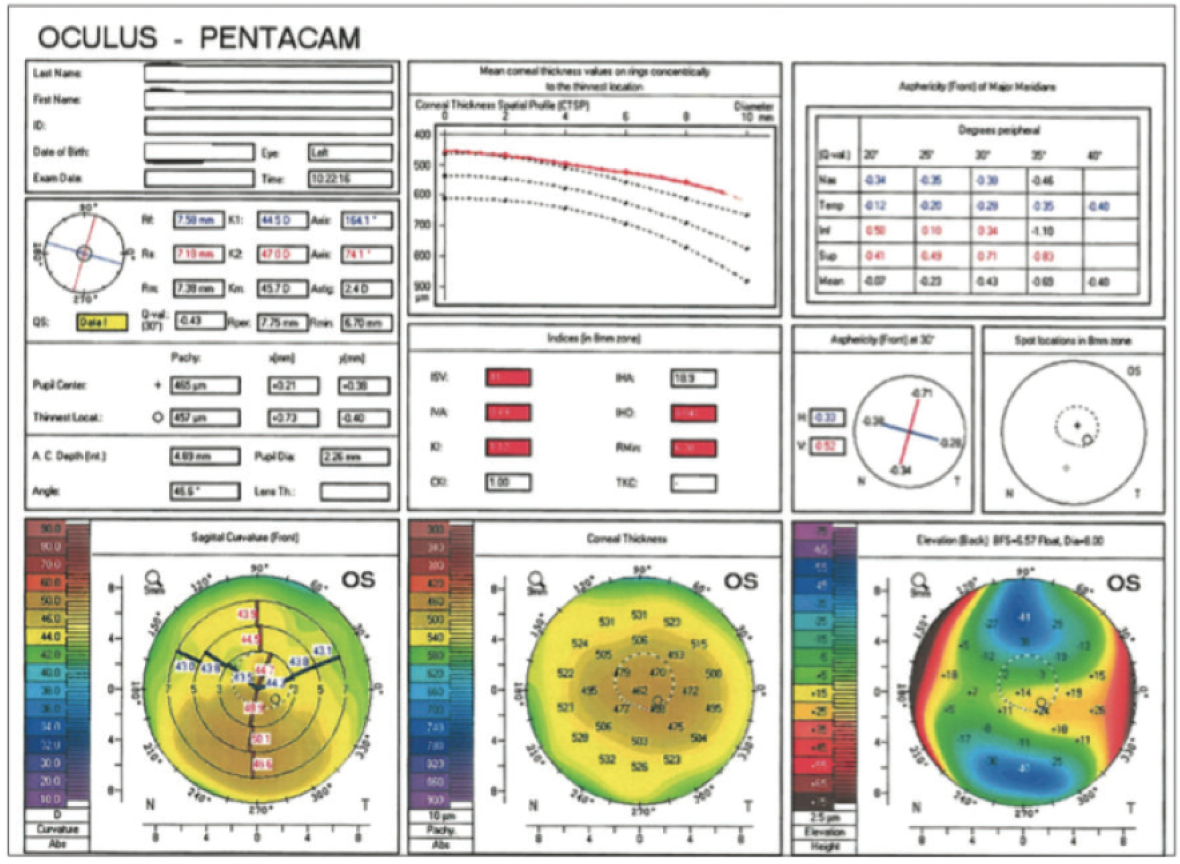
Figure 2. An eye with 2.50 D of cylinder at 74° and a fairly regular inferior cone achieved a postoperative UCVA of 20/30 with a toric IOL.
Uncomplicated surgery was performed. The final postoperative refraction was -0.25 D of sphere with UCVA of 20/30.
PATIENT SELECTION and surgical approach
Choosing the right candidates for this procedure is crucial. A toric IOL should not be implanted in an eye with advanced or unstable keratoconus or one with an apical corneal scar.
I tend to recommend toric IOLs for patients who are older than 50 years, who have had stable topography for several years, and, most important, who have realistic expectations and know that contact lenses or glasses may still be necessary. The astigmatism should not be highly irregular on topography, and the major axis of astigmatism should be identifiable. If the axes of cylinder on topography, keratometry, and manual refraction are all within a few degrees of one another, there is a good chance of success. On the other hand, wildly varying axes at differing optical zones may be a sign of instability or can simply make it very difficult to determine the correct axis for positioning the toric lens.
Young patients who have not undergone CXL should be avoided because their eyes may still undergo significant astigmatic shifts if the ectasia progresses. By the time patients reach their 50s and onward, the cumulative effects of a lifetime of UV light exposure have often provided enough natural crosslinking to help stabilize keratoconic progression.
Informed consent should be carefully worded to include the chance of visual limitations. These patients are incurring out-of-pocket expenses, which may increase their expectations, and therefore, I typically under-promise by telling them that there may be no major improvement in their UCVA after surgery. I explain that the astigmatic axis may shift when the cataract incisions are made, but, in their mildly keratoconic state, their vision may still be improved with contact lenses or glasses after surgery.
Precise preoperative measurements and surgical technique are important. I carefully mark the axis of astigmatism and the major incision at the slit lamp. I perform standard IOL power calculations with the SRK-T or Hoffer Q formulas, and I use the Johnson & Johnson Vision or Alcon toric calculator, depending on whether I am implanting a Tecnis Toric (Johnson & Johnson Vision) or »AcrySof Toric (Alcon) IOL. A capsulorrhexis that overlaps the IOL optic is crucial to help ensure postoperative IOL stability. If a laser capsulorrhexis is not performed, I use a 5.25-mm optical zone marker on the cornea to help guide making the capsulotomy so that the edge of the rhexis will overlap the optic around 360°. I do not use intraoperative keratometry or aberrometry in these eyes.
CONCLUSION
Carefully selected patients with keratoconus can benefit from toric IOLs to reduce astigmatism and provide improved postoperative UCVA without a contact lens. See Success Stories for details of two such cases.
1. Kennedy RH, Bourne WM, Dyer JA. A 48-year clinical and epidemiological study of keratoconus. Am J Ophthalmol. 1986;101:267-73.
2. Koch DD, Ali SF, Weikert MP, et al. Contribution of posterior corneal astigmatism to total corneal astigmatism. J Cataract Refract Surg. 2012;38:2080-2087.