CASE PRESENTATION
Two years after undergoing cataract and IOL surgery, a 67-year-old woman presents with complaints of progressively decreasing vision, worsening light sensitivity, and ocular dryness unresponsive to an intensive artificial tear regimen and punctal plugs. The patient’s ocular history is significant for macular degeneration (she is monitored by a retina specialist), bilateral monovision LASIK in 2002, and posterior capsular opacification after cataract surgery that was treated with a YAG capsulotomy.
OCT shows cystoid macular edema (CME). The patient begins treatment with an NSAID (bromfenac ophthalmic solution twice daily), steroids, and difluprednate ophthalmic emulsion 0.05% (»Durezol; Alcon). Although the retina subsequently shows improvement, her symptoms continue to worsen. The patient complains of a “constant gritty sensation” in her left eye.
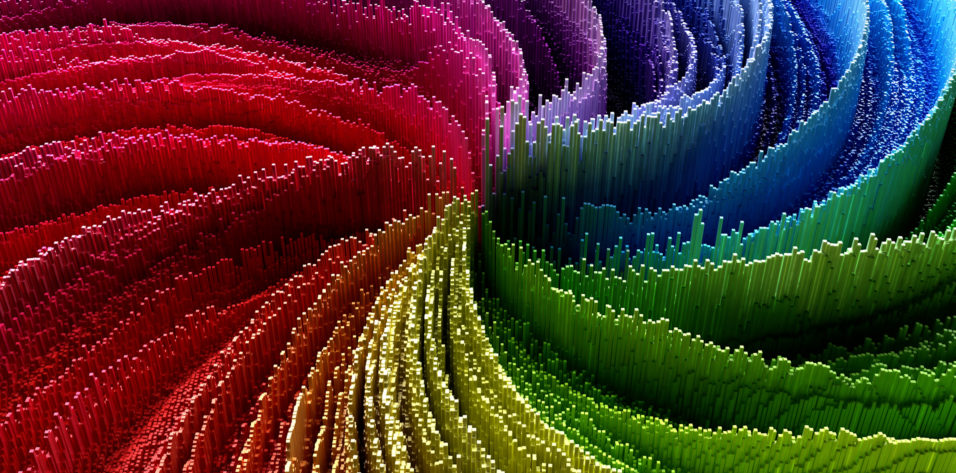
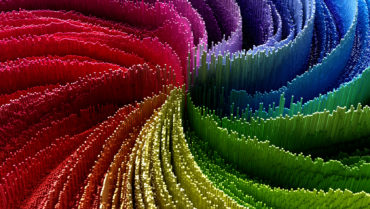
Sixty days after presentation, a slit-lamp examination of the patient’s left eye reveals an infiltrate in the anterior stroma, clefting between the LASIK flap and stroma, and flap edema (Figure 1). Anterior segment OCT (AS-OCT) shows similar findings isolated to the LASIK flap (flap edema and interface fluid clefts; Figure 2). The working diagnosis is IOP-induced steroid keratopathy and possible viral keratitis. The patient begins treatment with oral acyclovir 800 mg five times per day, erythromycin ointment, latanoprost, oral acetazolamide, and sodium chloride hypertonicity ophthalmic ointment, 5% (Muro 128; Bausch + Lomb).

Figure 1. A slit-lamp examination of the left eye reveals corneal edema.
Figure 2. Anterior segment OCT shows LASIK flap edema and interface fluid clefts.
One week later, a slit-lamp examination shows decreasing edema and inflammation, but there is minimal improvement 2 weeks later. An endothelial cell count finds substantial loss (495 cells/mm2) in the left eye (Figure 3). On slit-lamp examination and AS-OCT, however, the underlying stromal bed has a normal appearance, with edema present only in the flap.
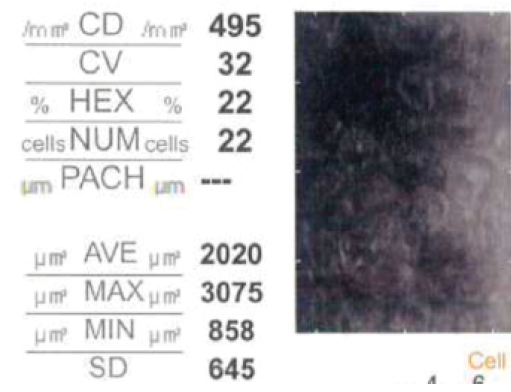
Figure 3. Specular endothelial micrography demonstrates substantial corneal endothelial cell loss.
How would you proceed? Is this how pseudophakic bullous keratopathy presents in post-LASIK eyes? Is Descemet stripping endothelial keratoplasty warranted? Is the cell count confounded by flap edema?
—Case prepared by Bala Ambati, MD, PhD; and Sneha Konda

ALAN N. CARLSON, MD
The timing of this case could not be better as I am currently managing three patients experiencing late-onset LASIK interface fluid collection resulting from recently performed non–refractive surgical procedures. I genuinely believe that we refractive surgeons will see more of this complication as the LASIK patient population ages and requires surgical intervention for other conditions. Furthermore, David M. Maurice, PhD, is being posthumously inducted into the ASCRS Ophthalmology Hall of Fame in 2018 as the father of corneal physiology as it pertains to corneal fluidics, leading to these types of corneal problems.
With respect to this particular patient, macular degeneration made her more susceptible to CME. Two months of topical steroids likely caused her IOP to rise, leading to this phenomenon called by several names, including pressure-induced stromal keratitis (PISK). It is a challenge to measure the IOP precisely because of the water-bed effect from fluid in the interface. Reducing the IOP is usually helpful, but this patient has a very low cell count, giving her marginal pump function.
I recommend a consultation with a medical retina specialist to determine if intravitreal injections of an anti–vascular endothelial growth factor agent would be useful in managing the retinal edema. I would coordinate a Descemet stripping automated endothelial keratoplasty procedure around these injections. Stripping of Descemet membrane is not needed if there is no significant posterior collagenous layer, as seen with Fuchs dystrophy. I have had success performing Descemet stripping automated endothelial keratoplasty and adding temporary compression sutures to the LASIK flap. I do not find venting incisions tremendously useful in cases like this one, and they carry a slight risk of introducing epithelium into the interface. I would avoid removing the epithelium unless it was loose, because the entire flap can dislocate during epithelial removal.

SIMON P. HOLLAND, MB, FRCSC
I think this is a case of either interface fluid syndrome (IFS) or PISK, as recently covered in this series.1 The patient in this case underwent a YAG capsulotomy and then developed CME treated with a 2-month course of topical steroids and bromfenac.
First, it would be critical to assess the peripheral IOP with a »Tono-Pen (Medtronic) or pneumotonometer because these readings are likely to be higher than measured centrally over the flap. Aggressive management of elevated IOP (if present) is needed, and I would assume that the IOP is higher than measured, even peripherally.
Information on why the cell count is low is not provided; perhaps the decrease is related to difficult cataract surgery. Nonetheless, I think Figure 3 is clear enough to show the enlarged endothelial cells despite the flap edema. I would proceed with an endothelial keratoplasty as soon as the pressure was reasonably controlled. Interface fluid may persist, but I am encouraged by the initial improvement in stromal edema after glaucoma treatment was initiated. In my opinion, the longer the clefts remain, the more difficult it will be to eliminate the IFS, because interface inflammation will continue, leading to scarring. I have encountered a similar case of IFS after endothelial failure from chlorhexidine toxicity and several cases after LASIK performed for postkeratoplasty astigmatism. I suspect this patient’s condition may be related to the low endothelial cell count and poor flap edge adhesion.
IFS is rare and difficult to diagnose and treat, so early detection is critical. The complication should be suspected in any patient with edema in the LASIK flap and cornea that has no obvious cause.


MUJTABA A. QAZI, MD; AND JONATHAN CREWS, DO
In post-LASIK eyes, corneal edema from a variety of etiologies, including cataract surgery, uveitis, trabeculectomy, and Fuchs dystrophy, can accumulate within the flap interface.2-5 Furthermore, IFS can relate specifically to steroid use and elevated IOP.6-12 The questions in this case are what is causing the edema and what is the appropriate management strategy if IFS persists despite medical therapy.
The endothelial cell count is low, with significant pleomorphism and polymegathism. If the cornea had a low endothelial cell count preoperatively, then the eye may be predisposed to IFS.
An interesting aspect of this case is that the stromal edema appears to have cleared, based on the results of a slit-lamp examination and AS-OCT, but fluid lingers within the interface. Perhaps the new potential interlamellar space requires less hydrostatic pressure to fill, and thus, as the edema begins to resolve, this space may be the last place to clear.
In addition to continuing to maximize medical glaucoma therapy, we would attempt to lift the flap edge either regionally or 360º to permit temporary egress of the trapped interface fluid. Then, we would repeat IOP measurements, pachymetry, specular microscopy, and AS-OCT to assess whether an endothelial keratoplasty is indicated. Descemet membrane endothelial keratoplasty has been shown to resolve IFS in the setting of Fuchs dystrophy.5

WILLIAM B. TRATTLER, MD
PISK can be a challenge to diagnose. The condition occurs in patients with a history of LASIK. With elevated IOP, fluid can accumulate in the space between the LASIK flap and the underlying stroma, while slit-lamp examination will typically reveal the presence of corneal edema. Oftentimes, eye care providers continue or increase the dosing of steroid eye drops because they assume that the condition is inflammatory. The diagnosis is further confused by Goldmann applanation tonometry, which incorrectly suggests that the IOP is either normal or low. The inaccurate readings result from the fluid pocket in the cornea under the LASIK flap.
Eye care providers aware of PISK will use a Tono-Pen or the »Icare Home Tonometer (Icare USA) to measure the IOP peripheral to the flap, which will reveal if the IOP is elevated. If so, treatment should focus on lowering the IOP, which will help reduce the corneal edema and allow the fluid pocket under the flap to resolve.
In this case, PISK was identified after 2 months of difluprednate use. Neither the initial IOP nor the IOP after topical steroid treatment is provided. When PISK was diagnosed, therapy was changed to eliminate the use of the antiinflammatory drugs, and the patient began administering two IOP-lowering agents along with sodium chloride hypertonicity ointment at bedtime. She was also placed on acyclovir for a presumed herpes simplex virus corneal infection, although no description of a dendrite was provided. Nor were any other specific findings of herpes simplex virus identified. Erythromycin ointment was also started, again with no description provided as to why it would be needed.
After 2 weeks of hypotensive therapy, an endothelial cell count was attempted despite the continuing presence of flap edema. Not surprisingly, the endothelial cell count was abnormal. Endothelial cell counts are known to be unreliable in the presence of corneal edema, so I would disregard this measurement for now. Because no IOP reading has been provided, my main concern is that the IOP is still elevated enough for some degree of PISK to remain and that it is responsible for the continued flap edema. I would measure the IOP on the peripheral part of the cornea and initiate additional therapy to lower the IOP. In some cases, surgical intervention such as micropulse cyclophotocoagulation using the »Cyclo G6 Glaucoma Laser System (Iridex) or microinvasive glaucoma surgery may be required. I would expect the flap edema to resolve and the patient’s vision to improve after the IOP is reduced to a low level. Endothelial surgery is not indicated. Of note, if the main issue were inadequate endothelial cell functioning, I would expect the entire cornea to have demonstrated edema rather than just the flap edema noted.
1. Gorovoy MS, Hoffman RS, Maloney RK, Carlson AN. Persistent LASIK flap interface fluid after DSAEK procedure. Cataract & Refractive Surgery Today. February 2018; 18(2):19-21.
2. Ortega-Usobiaga J, Martin-Reyes C, Liovet-Osuna F, et al. Interface fluid syndrome in routine cataract surgery 10 years after laser in situ keratomileusis. Cornea. 2012;31(6):706-707.
3. McLeod SD, Mather R, Hwang DG, Margolis TP. Uveitis-associated flap edema and lamellar interface fluid collection after LASIK. Am J Ophthalmol. 2005;139(6):1137-1139.
4. Kang SJ, Dawson DG, Hopp LM, et al. Interface fluid syndrome in laser in situ keratomileusis after complicated trabeculectomy. J Cataract Refract Surg. 2006;32(9):1560-1562.
5. Luceri S, Baksoellah Z, Ilyas A, et al. Interface fluid syndrome after laser in situ keratomileusis (LASIK) because of Fuchs endothelial dystrophy reversed by Descemet membrane endothelial keratoplasty (DMEK). Cornea. 2016;35(12):1658-1661.
6. Dawson DG, Schmack I, Holley GP, et al Interface fluid syndrome in human eye bank corneas after LASIK: causes and pathogenesis. Ophthalmology. 2007;114(10):1848-1859.
7. Han SB, Woo SJ, Hyon JY. Delayed-onset interface fluid syndrome after laser in situ keratomileusis secondary to combined cataract and vitreoretinal surgery. J Cataract Refract Surg. 2012;38(3):548-550.
8. Najman-Vainer J, Smith RJ, Maloney RK. Interface fluid after LASIK: misleading tonometry can lead to end-stage glaucoma. J Cataract Refract Surg. 2000;26(4):471-472.
9. Galal A, Artola A, Belda J, et al. Interface corneal edema secondary to steroid-induced elevation of intraocular pressure simulating diffuse lamellar keratitis. J Refract Surg. 2006;22(5):441-447.
10. Hamilton DR, Manche EE, Rich LF, Maloney RK. Steroid-induced glaucoma after laser in situ keratomileusis associated with interface fluid. Ophthalmology. 2002;109(4):659-665.
11. Belin MW, Hannush SB, Yau CW, Schultze RL. Elevated intraocular pressure-induced interlamellar stromal keratitis. Ophthalmology. 2002;109(10):1929-1933.
12. Galvis V, Tello A, Revelo ML, Valarezo P. Post-LASIK edema-induced keratopathy (PLEK), a new name based on pathophysiology of the condition. BMJ Case Rep. 2012. doi:10.1136/bcr-2012-007328.