As the year draws to a close, it is a natural time to take stock. What was achieved? What was learned? Asked to reflect on the gains of 2017 in ophthalmology, members of CRST’s editorial board cast their votes for the best technologies, research, and surgical pearls. Because this issue went to press before 2018, developments from the last weeks of 2017 are not included. Nevertheless, this year had plenty to offer.


Transection
“Kind of low-tech but nothing short of brilliant” is how William J. Lahners, MD, of Sarasota, Florida, described the miLoop (IanTech).
Seven surgeons chose this single-use, disposable instrument as the year’s best new technology. The device features “a flexible, retractable nitinol snare that can be used to transect even the densest cataracts into multiple segments,” commented Philadelphia surgeon Richard Tipperman (Figure 1). “Nitinol is a metal alloy which has ‘memory,’ and the snare is formed to mimic the shape of a cataractous lens.”
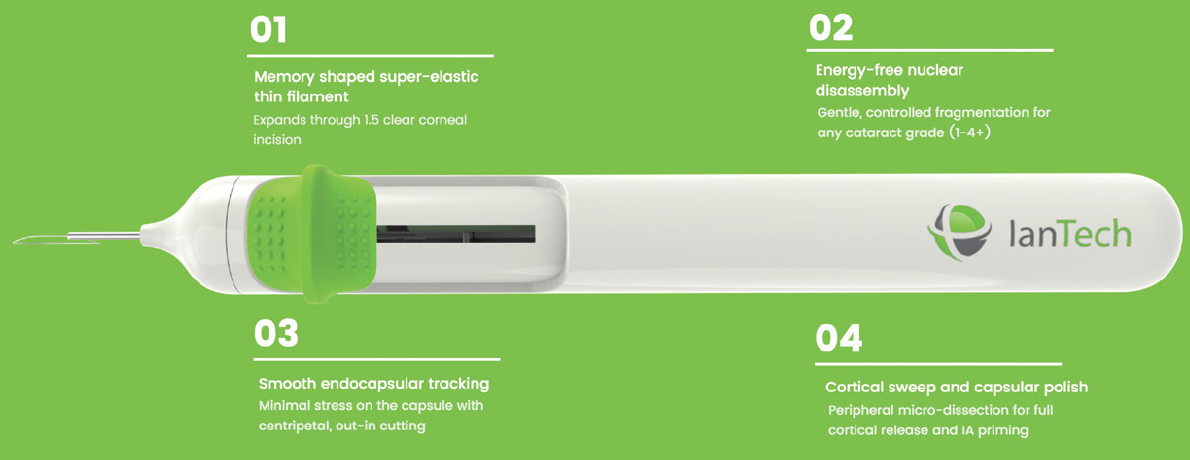
Figure 1. The miLoop received more votes than any other technology for the year’s best from CRST’s panel.
According to Sheri Rowen, MD, of Newport Beach, California, the snare can safely bisect “any part of the crystalline lens without the use of laser or phaco energy.” She has found the instrument extremely useful for dense brunescent and white cataracts. “The miLoop snare wraps around the lens inside the capsule and easily is manipulated to cut the lens in perfect fragments, which are then easily removed with phaco ultrasound,” she commented.
All cataract surgeons have encountered lenses with a leathery posterior shell that slows extraction, even with the best femtosecond laser technology, Dr. Lahners remarked. “This device can bisect the toughest lenses in seconds and greatly facilitates those challenging cases where the phaco [tip] cannot even cut a groove,” he said.
Chief Medical Editor Robert J. Weinstock, MD, of Largo, Florida, highlighted the instrument’s assistance with prechopping rock hard cataracts prior to phacoemulsification. “This novel device can greatly ease the removal of cataracts in these challenging cases and potentially reduce the incidence of capsular tears and vitreous loss, which is common in [eyes with] extremely dense and large cataracts,” he said.
Echoing this sentiment, Miami surgeon William B. Trattler stated, “This technology helps break up dense cataracts into small pieces and loosens the cortex, resulting in less inflammation in the eye and less postoperative corneal edema.”
Dr. Tipperman cited a presentation on the miLoop that won the “Best Paper of Session” award for the “Cataract Phaco Techniques, Instrumentation, and IOL Fixation” session at the 2017 annual meeting of the American Society of Cataract and Refractive Surgery (ASCRS).1 “I was one of the moderators on the panel for this session, and during the discussion portion, it was interesting to hear many audience members who have used this device speak about what a ‘game changer’ it would be for extremely dense cataracts, especially in locations where maintenance and use of more complex phacoemulsification machines pose a challenge,” he said. “Accomplished and excellent phacoemulsification surgeons who have utilized this device praise the safety, simplicity, and ease of use and see it both as an adjunct and standalone device to aid cataract surgery.”
Seattle surgeon Audrey R. Talley Rostov anticipated using the technology herself as an adjunct to a femtosecond laser for surgery on eyes with dense cataracts. Dr. Lahners believes the instrument “has great potential to help the 25,000,000 people around the world that are blind due to cataracts, especially in areas where phaco technology is unavailable.” Dr. Rowen suggested that the miLoop will be useful in resident cases and procedures with poor corneal visibility as well.
P. Dee G. Stephenson, MD, noted that the instrument can pass through a relatively small pupil. “It can cut through soft or dense cataracts, so it has the ability to work on any cataract surgery,” she added. “There is a small learning curve for a large gain.” (See video below.)
William F. Wiley, MD, uses the miLoop device to transect a cataract.

Capsulotomy
Both Chief Medical Editor Steven J. Dell, MD, of Austin, Texas, and Vance Thompson, MD, of Sioux Falls, South Dakota, voted for the Zepto (Mynosys), a device Dr. Thompson called “amazing.” The disposable technology allows cataract surgeons to automatically create a perfectly circular capsulotomy (referred to as a “precision pulse capsulotomy”). Commented Dr. Dell, “The ability to create quick and reliable capsulotomies, even in dense lenses with limited visibility, is an attractive feature of this promising technology.”

IOLs
Los Angeles surgeon Uday Devgan and Cathleen M. McCabe, MD, of Bradenton and Sarasota, Florida, both nominated the AcrySof IQ ReStor +2.5 D Multifocal Toric IOL with Activefocus (Alcon).
“This is the multifocal IOL that I’ve been waiting for,” Dr. Devgan said. “It gives a wider range of vision, but it [is] still distance dominant, and toric corrections are available, too. It’s not as perfect as having youthful accommodation, but certainly, it is the best of the current [multifocal IOLs].”
Dr. McCabe cited the platform’s improved rotational stability and “the monofocal-like distance acuity and contrast sensitivity.” She continued, “The lens allows me to provide excellent visual outcomes and [an] improved range of vision for my premium lens cataract surgery patients.” She added that this particular multifocal toric design enables her to provide patients who have significant corneal astigmatism with greater independence from reading glasses.

Data for Cataract Surgery
Arthur Cummings, MB ChB, FCS(SA), in Dublin, Ireland, was most impressed by the Argos (Movu), an optical coherence tomography swept-source biometer launched in the United Kingdom and Ireland this year.
“It is easier to use and quicker than our Lenstar [Haag-Streit] and IOLMaster 500 [Carl Zeiss Meditec] and can capture data with dense cataracts where the other two may fail,” he commented. “Of all the biometry devices that we have, it is also the device that my staff prefer to use, given its speed and ease of use. It seems to provide the same IOL prediction as the other two devices do, and an ongoing comparative study that we are doing will look at other parameters (like [anterior chamber] depth, lens thickness, [white-to-white] measurements, etc.) more closely.

Pinhole Implant
Cincinnati surgeon Michael E. Snyder nominated the latest iteration of the XtraFocus Pinhole Implant (Morcher), designed by Claudio Trinidade, MD. Dr. Snyder remarked that the device “is able to achieve functional, high-quality vision in patients with irregular corneas from old [radial keratotomy], keratoconus, post-LASIK ectasias, [penetrating keratoplasty], and the like under circumstances in which their only alternatives are either scleral contact lenses or penetrating keratoplasty. This ingenious black device has now been redesigned with an open-loop sulcus configuration. The black acrylic material is transparent to infrared light.” Dr. Snyder added that Dr. Trinidade’s video of this device, “Tiny Hero Against the Evil Axis,” won the grand prize at the 2017 ASCRS film festival.

Vitrectomy
According to Lisa Brothers Arbisser, MD, of Davenport, Iowa, Vitesse (Bausch + Lomb), “a hypersonic vitrectomy system, is the most important new, truly disruptive device in the ophthalmic surgical space. Since the 1970s, we have removed vitreous with a cutter, a needle within a needle that shears the vitreous matrix after sucking it into a port. … We have lessened traction with higher cut rates [and] become more minimally invasive with smaller-gauge instrumentation, but nothing has materially changed until now. Vitesse effectively liquefies vitreous [via] an effective cutting rate of 1.7 million cuts per minute at the tiny port with unprecedented rapidity and vastly lower flow and turbulence. As I write this, the first posterior segment cases have just been performed, and we have yet to explore this tool for unplanned vitrectomy for the anterior segment surgeon.”
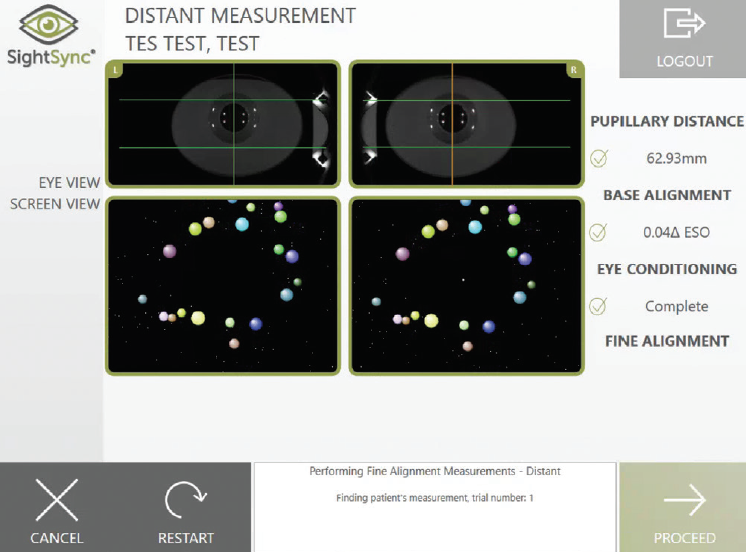
Figure 2. The SightSync test on the Neurolens System.

Dry Eye Disease
Cynthia Matossian, MD, of Doylestown, Pennsylvania, selected the TrueTear (Allergan). When inserted by the patient into his or her nose, the two prongs of the handheld device contact the ophthalmic branch of the trigeminal nerve and stimulate cranial nerve VII, which innervates the lacrimal glands, thereby increasing tear production.

Headache Relief
John Berdahl, MD, of Sioux Falls, South Dakota, voted for the Neurolens System (eyeBrain Medical). According to the company, the system uses the proprietary SightSync test and eye tracking technology to objectively measure the amount of binocular misalignment a patient is experiencing at distance and near (Figure 2). Neurolenses integrating a progressive prism design and the patient’s refractive correction can then be prescribed. Dr. Berdahl reported that he has had patients whose use of this technology has produced “incredible improvement” in headaches caused by “proprioceptive misalignment.”


Ocular Surface
Dry eye disease (DED) narrowly beat out IOLs as the panel’s most popular topic in the category of best research or review article/presentation of the year.
Christopher Starr, MD, of New York asserted, “Nothing can compare to the scope and influence of the mighty TFOS DEWS II report. In my opinion, it is easily the most important research publication of 2017.”2-12 Dr. Berdahl agreed.
Mitchell A. Jackson, MD, of Lake Villa, Illinois, selected work by CEDARS/ASPENS13 that he considers to be one of the main algorithms for treating ocular surface disease in addition to the TFOS DEWS II report. Dr. McCabe concurred, saying that the former “provides a roadmap for the diagnosis and treatment of patients with dysfunctional tear syndrome. This important paper expands previous recommendations to include current technologies and clinical decision making.”
Dr. Trattler nominated a research collaboration by 11 US surgeons, including himself, who studied the incidence of DED prior to cataract surgery.14 “The results from the PHACO [Prospective Health Assessment of Cataract Patients’ Ocular Surface] study were very surprising, as it found a much higher incidence of dry eye in patients presenting for cataract surgery than what was previously thought.”
Voting from Laguna Hills, California, John A. Hovanesian, MD, picked a study that Preeya K. Gupta, MD, presented at the 2017 annual meeting of the ASCRS.15 The researchers found “that 56% of asymptomatic children aged 4 to 17 have signs of meibomian gland atrophy, suggesting preclinical dry eye,” he said. That such a young population was affected by early signs of DED disturbs him. “It’s hard to ignore that the typical American diet today contains a small fraction of the omega-3 oils that it did one or two generations ago,” he remarked. (See Listen Up.)

LISTEN UP
When CRST’s panel was asked to identify the best research published or presented in 2017, one of the most popular subjects was dry eye disease. In this episode of the podcast Informed Consent, Frank Bucci Jr, MD; Sheri Rowen, MD; and Alice Epitropoulos, MD, join Marguerite McDonald, MD, to discuss the effect of omega-3 fatty acids.
Click on the microphone to listen now.

IOLs
Dr. Tipperman nominated a three-part “tour de force of the latest … thinking and information regarding IOL power calculations.”16-18 Reading these articles, he said, gives anterior segment surgeons “information to provide the best care possible for their patients in terms of implant power calculations while also outlining future work and potential advances in the field.”
Both Dr. Dell and Karolinne Maia Rocha, MD, PhD, of Charleston, South Carolina, nominated a publication by Shin Yamane, MD, and colleagues.19 Dr. Dell commented that this innovative and elegant double-needle technique for IOL fixation “can be a life-saver in difficult clinical situations where fixation support is required in the absence of adequate capsular or zonular support.”
Dr. Matossian chose a task force’s “excellent review” of the minimal criteria for defining an extended-depth-of-focus IOL.20

Endophthalmitis
Endophthalmitis prophylaxis in cataract surgery was on the minds of Drs. Arbisser and Stephenson this year. Dr. Arbisser selected a large published analysis of intracameral moxifloxacin by Haripriya and colleagues.21
“Although this study is a retrospective clinical registry design, I believe it to show compelling evidence of efficacy due to the huge number of consecutive patients operated [on] just over a 2-year period,” she remarked. “There is a nearly sixfold decrease in the incidence of endophthalmitis in phacoemulsification cases with intracameral moxifloxacin use!”
Dr. Arbisser began using self-preserved intracameral moxifloxacin hydrochloride ophthalmic solution 0.5% (Vigamox; Alcon) off label immediately after reading the original study on the subject by the European Society of Cataract & Refractive Surgeons.22
“I never saw an infection thereafter,” she stated, noting the safety of this form of prophylaxis.23 “There are now several reliable sources of intracameral moxifloxacin available, and it’s debatable whether we will ever have a specifically on-label FDA-approved source. How many avoidable blinding cases of endophthalmitis will we suffer while waiting?”
Considering the small but devastating risk of vancomycin-associated hemorrhagic occlusive retinal vasculitis24 and moxifloxacin’s broad spectrum of antimicrobial activity, Dr. Arbisser said she cannot imagine cataract surgery without the latter intracameral agent for prophylaxis.
Dr. Stephenson was impressed by the latest data from the Aravind Eye Care System in Tamil Nadu, India, presented in a reply to a letter regarding the study by Haripriya and colleagues.21,25 All patients in the study received 0.5 mg of moxifloxacin ophthalmic solution 0.5% (0.1 mL; Auromox [Aurolab; not available in the United States]) as a direct intracameral injection at the conclusion of cataract surgery.
“Dr. Chang [and colleagues] updated the data to include all cases performed through March 2017,” she said. “There are now 1,087,907 consecutive eyes [on which cataract surgery was] performed during the 51 months starting in January 2013. The endophthalmitis rate was 0.02% in the 555,550 eyes that received [intracameral] moxifloxacin prophylaxis, compared to 0.07% in the 532,357 eyes that did not. What makes the Aravind study so strong [are] the large number of cases done in a short amount of time and the efficiency and cost-effectiveness. Not only are the cataract protocols standardized between all the [Aravind Eye Care System] hospitals, but they use the same viscoelastic and sterilization and draping techniques. This makes this one of the strongest studies to date supporting the efficacy of intracameral moxifloxacin.”

Cornea
Casting his vote from Charleston, South Carolina, George O. Waring IV, MD, selected research showing a combined tomographic and direct in vivo biomechanical analysis to be a “sensitive way of detecting subclinical (fruste) ectasia among eyes with normal topography in [cases of great asymmetry] … where one eye appears topographically normal.”26 He added that the method “may also confirm unilateral ectasia, potentially characterizing the inherent ectasia susceptibility of the cornea, which should be the subject of future studies.”
Dr. Lahners nominated research on the viability of donor corneas.27 “The Cornea Preservation Time Study (CPTS) is a prospective blinded study with 36 participating clinical sites, including over 50 corneal surgeons, and 23 participating eye banks,” he explained. “It is the first of its kind to study whether endothelial keratoplasty (a corneal transplant surgery) using donor corneas preserved beyond 8 days may be as successful as a surgery using donor corneas preserved less than 8 days. This landmark study has shed an enormous amount of information on how long donor corneas can safely be kept in preservation media. It will have a huge impact on corneal transplantation practice patterns in the United States and may help prevent donor shortages that some predict due to increasing population age and other eye banking challenges.”

Refractive Surgery
Dr. Cummings nominated a multicenter, international study in which he was involved, although he emphasized that his participation was not the reason for his vote. Rather, he said the study “demonstrated the power of modern LASIK. Patients with myopia and myopic astigmatism were treated with LASIK using the WaveLight Refractive Suite [Alcon], and the primary endpoint was comparing binocular [uncorrected distance visual acuity] 1 month postoperatively to preoperative binocular [corrected distance visual acuity]. The findings were nothing short of spectacular, with a statistically significant improvement in uncorrected postoperative visual acuity over preoperative best-corrected visual acuity. The most basic ablation profile was used, namely the wavefront-optimized profile, and yet the results were so convincing.”28

Presbyopia
Dr. Rowen nominated the first presentation on CSF-1 (PresbiDrops; Orasis Pharmaceuticals; not FDA approved), which she delivered at the European Society of Cataract & Refractive Surgeons’ meeting this autumn.29 “This is a novel drop formulation for temporary improvement in near vision,” she said. “Early data in 3/4 study groups showed [a] statistically significant improvement of three lines of reading vision. This could be another bridge to correct near vision for presbyopia.”

Astigmatism
Dr. Weinstock selected a study in which he participated on how much cyclotorsion occurs during the laser portion of laser cataract surgery.30 He commented that the research demonstrated “the importance of a preoperative imaging [device] to account for and eliminate this error for more accurate astigmatism management with the femtosecond laser and the advantage of a registration process with the Cassini [i-Optics] and Lensar Laser System [Lensar].”
BOOKMARK FROM 2016
Los Angeles surgeon Robert K. Maloney nominated a study published after CRST’s article on the best of 2016 went to press. Although the study does not officially fit the best of 2017, Dr. Maloney considers it to be the best review of the current state of laser cataract surgery.1 In it, the authors discussed the benefits of the laser for decreasing endothelial cell damage and improving the capsulotomy, he said.
“It suggests that femtosecond [laser cataract] surgery does not decrease the risk of posterior capsule rupture, but that, in my opinion, is only because the studies compared experienced manual surgeons to novice laser surgeons,” Dr. Maloney remarked. “It is still worth reading to understand where the field is.”
1. Popovic M, Campos-Möller X, Schlenker MB, Ahmed II. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14 567 eyes. Ophthalmology. 2016;123(10):2113-2126.


Drop Regimens
Casting his vote from Pekin, Illinois, William I. Bond, MD, chose a pearl Dr. Berdahl shared during a talk at Imprimis’ booth during the 2017 ASCRS meeting. “Only give 0.15 mL of the Dropless formula rather than the 0.2 mL initially recommended,” Dr. Berdahl advised, according to Dr. Bond. He went on to explain, “0.2 mL causes a good deal of volume pressure in the eye, with [an] increased chance of wound trouble and issues with pressures [postoperatively]. I had been doing the technique in this manner by practical experience but was very pleased to see someone recommending it rather than just doing it that way myself.”
Dr. Waring selected advice Dr. Dell discussed this year but credited to Louis E. Probst, MD. Specifically, Dr. Waring said these surgeons use nonsteroidal anti-inflammatory drugs and no steroids as their standard regimen after PRK, an example of a trend in ophthalmology toward fewer eye drops. “Dr. Dell’s experience is a great example of rethinking the dogma of our traditional postoperative regimen,” Dr. Waring stated. “Dr. Dell and Dr. Probst recommend use of the bromfenac molecule for this purpose.”
For Dr. Weinstock, the year’s top pearl came from Beau Swann, MD, who he said has developed a surgical technique for patients undergoing laser cataract surgery whose small pupils resist dilation with convention drops. In the laser suite, the patient receives a drop of diluted povidone-iodine, Dr. Weinstock explained. Then, the ophthalmologist uses a surgical microscope for visualization, and with a tuberculin syringe and a 30-gauge needle, he or she injects 0.2 mL of phenylephrine 1% and ketorolac 0.3% (Omidria; Omeros) into the anterior chamber via a nasal clear corneal injection site. According to Dr. Weinstock, within 1 minute, the pupil usually dilates sufficiently to permit the laser capsulotomy and nuclear fragmentation. He said that a study is underway to demonstrate the safety and effectiveness of the technique.

Pupilloplasty
Dr. Jackson’s favorite tip this year was Dr. Agarwal’s single-pass, four-throw suture technique as an option for pupilloplasty.31 Dr. Jackson watched Dr. Agarwal perform the procedure live at his surgical center in Chennai, India, just prior to the 2017 annual meeting of the Intraocular Implant and Refractive Society of India. “This technique is an excellent, fairly atraumatic approach to [repairing] traumatized pupils” and, indirectly, to helping patients with narrow angles, Dr. Jackson said.

IOL Positioning
“I learned something about toric IOLs that, on reflection, I should have known but was simply not practicing,” Dr. Cummings revealed. He said that, after placing a toric IOL in the bag, he would normally press down on the optic to “settle” the lens into position and, he hoped, prevent its rotation during the postoperative period. One of his colleagues suggested he expand the haptics with a Sinskey hook or another instrument before completing the procedure so as to maximize contact between the haptic and the equator of the capsular bag and thus further reduce rotational risk prior to exiting the eye for the last time.
Dr. Hovanesian voted for the primary buttonholing posterior capsulotomy taught by Dr. Arbisser. The surgeon intentionally opens the posterior lens capsule and positions the posterior chamber IOL’s optic posteriorly through the opening, he said. “Naturally, this must be done in Berger’s space without violating the anterior hyaloid,” Dr. Hovanesian remarked. “This technique gives rock-solid lens positioning in three dimensions and prevents future [posterior capsular opacification]. While this is not for every case—or every surgeon—it probably deserves a future in our field of cataract surgery.”
Dr. Starr found his favorite surgical pearl of the year in the published research of Bonnie A. Henderson, MD.33,34 Her work showed “that positioning the haptic-optic IOL junction in an inferotemporal orientation may reduce the incidence of negative dysphotopsia after cataract surgery,” he said. Based on this information, Dr. Starr now attempts to leave all nontoric IOLs in this position.

Challenging Cataracts
Several years ago, Dr. Arbisser listened to a talk by Richard Mackool, MD, that included footage of what she termed a “video oddity.” She recalled, “A cortical opacity was in the way of his view for making the capsulorhexis. He happened to stroke the capsule with a cannula and noticed he could move the opacity out of the way. He joked that maybe he didn’t even have to continue with the cataract surgery but simply move the opacity out of the visual axis. We all laughed and forgot about it until this year. Professor Chee Soon Phaik, another brilliant surgeon, has made use of this capacity to ‘milk’ the contents of an intumescent lens with high intralenticular pressure to the periphery, manually flattening the profile of the bulging capsule. This simple, thinking-out-of-the-box maneuver significantly decreases the risk of [capsulorhexis] runout in these challenging cases.”35

IOL Power Calculations
Warren E. Hill, MD, has always been Dr. Tipperman’s “spiritual guru for all things regarding IOL calculations and biometry,” he said, so he paid close attention when he heard Dr. Hill praise the Barrett Rx IOL formula.
“I think most surgeons are already aware of how powerful the Barrett Universal IOL calculator is for IOL calculations in general,” Dr. Tipperman commented. “The Rx formula, which is built on the Universal formula, helps surgeons analyze and treat postoperative IOL power surprises.”
He paused to acknowledge Dr. Berdahl and David R. Hardten, MD, for developing astigmatismfix.com, which Dr. Tipperman described as a simple and straightforward website to help surgeons analyze toric IOL surprises and make corrections for misalignments.
As “great and groundbreaking” as the website is, he said, “the Barrett Rx calculator takes things further and represents a significant improvement and enhancement. This is because, at times, not only is a surgeon dealing with toric [lens] misalignment, but there is also a spherical power error or a toric power error.” Sometimes, simple rotation of the lens will solve the IOL power problem, he noted. Other times, however, it is necessary to change the toric and/or the spherical power, and sometimes, a piggyback IOL can be used, he said.
“The Barrett Rx formula allows surgeons to calculate the new spherical power for an IOL exchange, the strength of a piggyback IOL, and a ‘three-part solution’ for toric IOL surprise, including the appropriate axis orientation of the IOL, the best toric power, and any changes needed in the spherical power of the IOL,” Dr. Tipperman said.
He stated that the formula should definitely be in every cataract surgeon’s toolkit, and it may be accessed through the ASCRS website (seen here).36
D. Brian Kim, MD, posted a video of his modification of the Yamane scleral haptic fixation technique just in time to assist William J. Lahners, MD, in his first attempt at performing it.32 Dr. Lahners nominated the video as the year’s best surgical pearl. “A three-piece IOL can be fixed to the sclera without sutures in a method similar to the glued IOL technique of [Amar Agarwal, MBBS, FRCOphth], but with a more secure method of scleral fixation and no conjunctival dissection,” Dr. Lahners told CRST.

Astigmatism
The best surgical advice Dr. Devgan said he got this year was from Larry Berstein, MD. Because cataract surgeons cannot accurately predict surgically induced astigmatism, the best bet is to keep the phaco incision on the steep or even the flat axis, Dr. Devgan stated. In that way, the vector magnitude may change, but at least the vector direction will be the same.
“Think of it this way: if an airplane is flying and it experiences a direct headwind or a direct tailwind, then the speed of the plane changes, but its direction does not,” he explained. “[In contrast,] if you have a crosswind, then both the speed and direction are altered.”

Corneal Inlays
“The most valuable surgical pearl I learned was in discussion with [Jeffrey Whitman, MD] regarding the use of [mitomycin C] with [the] Raindrop Near Vision Inlay [ReVision Optics],” Dr. McCabe shared. “These eyes have remarkably clear inlay margins and a significantly reduced incidence of even very mild haze.” She is now combining bilateral LASIK treatment with the inlay in the patient’s nondominant eye. She applies mitomycin C 0.02% to the flap bed and the underside of the flap for 15 to 20 seconds prior to rinsing with balanced salt solution and placing the inlay. Dr. McCabe said the technique has expanded the population of patients who can benefit from the technology.
1. Ianchulev T, Tyson FC, MacDonald S, et al. Adjunct micro-interventional endocapsular lens fragmentation can significantly reduce phaco energy and fluidics: results of the Leep 103 RCT. Paper presented at: ASCRS/ASOA Annual Meeting; May 5-9, 2017; Los Angeles, CA.
2. Nelson JD, Craig JP, Akpek EK, et al. TFOS DEWS II introduction. Ocul Surf. 2017;15(3):269-275.
3. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15(3):276-283.
4. Sullivan DA, Rocha EM, Aragona P, et al. TFOS DEWS II sex, gender, and hormones report. Ocul Surf. 2017;15(3):284-333.
5. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15(3):334-365.
6. Willcox MDP, Argüeso P, Georgiev GA, et al. TFOS DEWS II tear film report. Ocul Surf. 2017;15(3):366-403.
7. Belmonte C, Nichols JJ, Cox SM, et al. TFOS DEWS II pain and sensation report. Ocul Surf. 2017;15(3):404-437.
8. Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report. Ocul Surf. 2017;15(3):438-510.
9. Gomes JAP, Azar DT, Baudouin C, et al. TFOS DEWS II iatrogenic report. Ocul Surf. 2017;15(3):511-538.
10. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II diagnostic methodology report. Ocul Surf. 2017;15(3):539-574.
11. Jones L, Downie LE, Korb D, et al. TFOS DEWS II management and therapy report. Ocul Surf. 2017;15(3):575-628.
12. Novack GD, Asbell P, Barabino S, et al. TFOS DEWS II clinical trial design report. Ocul Surf. 2017;15(3):629-649.
13. Milner MS, Beckman KA, Luchs JI, et al. Dysfunctional tear syndrome: dry eye disease and associated tear film disorders – new strategies for diagnosis and treatment. Curr Opin Ophthalmol. 2017;27(suppl 1):3-47.
14. Trattler WB, Majmudar PA, Donnenfeld ED, et al. The Prospective Health Assessment of Cataract Patients’ Ocular Surface (PHACO) study: the effect of dry eye. Clin Ophthalmol. 2017;11:1423-1430.
15. Stevens M. Prevalence of meibomian gland atrophy in a pediatric population. Paper presented at: ASCRS/ASOA Annual Meeting; May 5-9, 2017; Los Angeles, CA.
16. Koch D, Hill W, Abulafia A, Wang L. Pursuing perfection in intraocular lens calculations: I. Logical approach for classifying IOL calculation formulas. J Cataract Refract Surg. 2017;43(6):717-718.
17. Hill W, Abulafia A, Wang L, Koch. Pursuing perfection in IOL calculations. II. Measurement foibles: measurement errors, validation criteria, IOL constants, and lane length. J Cataract Refract Surg. 2017;43(7):869-870.
18. Wang, L, Koch, D, Hill, W, Abulafia A. Pursuing perfection in intraocular lens calculations: III. Criteria for analyzing outcomes. J Cataract Refract Surg. 2017;43(8):999-1002.
19. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
20. MacRae S, Holladay JT, Glasser A, et al. Special report: American Academy of Ophthalmology Task Force consensus statement for extended depth of focus intraocular lenses. Ophthalmology. 2017;124(1):139-141.
21. Haripriya A, Chang DF, Ravindran RD. Endophthalmitis reduction with intracameral moxifloxacin prophylaxis: analysis of 600,000 surgeries. Ophthalmology. 2017;124(6):768-775.
22. Barry P, Seal DV, Gettinby G, et al; ESCRS Endophthalmitis Study Group. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: preliminary report of principal results from a European multicenter study. J Cataract Refract Surg. 2006;32(3):407-410.
23. Arbisser LB. Safety of intracameral moxifloxacin for prophylaxis of endophthalmitis after cataract surgery. J Cataract Refract Surg. 2008;34(7):114-1120.
24. Witkin AJ, Chang DF, Jumper JM, et al. Vancomycin-associated hemorrhagic occlusive retinal vasculitis. Ophthalmology. 2017;124(5):583-595.
25. Chang DF, Haripriya A, Ravindran RD. Reply. Ophthalmology. 2017;124(10):e78-e79.
26. Ambrósio R Jr, Lopes BT, Faria-Correia F, et al. Integration of Scheimpflug-based corneal tomography and biomechanical assessments for enhancing ectasia detection. J Refract Surg. 2017;33(7):434-443.
27. Lass J; Cornea Preservation Time Study Group. Cornea Preservation Time Study (CPTS): advancing knowledge on effect of storage time on graft success and endothelial cell loss following DSEK. Paper presented at: Cornea and Eye Banking Forum; November 10, 2017; New Orleans, LA.
28. Cummings A, Durrie D, Gordon M, et al. Prospective evaluation of outcomes in patients undergoing treatment for myopia using the WaveLight Refractive Suite. J Refract Surg. 2017;33(5):322-328.
29. Rowen S. A twin centre, double-masked, randomized, placebo-controlled, repeated administration, crossover study to establish safety, tolerability and efficacy of CSF-1 for the improvement of near vision in presbyopic subjects. Poster presented at: XXXV Congress of the ESCRS; October 7-11, 2017; Lisbon, Portugal.
30. Hummel CD, Diakonis VF, Desai NR, et al. Cyclorotation during femtosecond laser-assisted cataract surgery measured using iris registration. J Cataract Refract Surg. 2017;43(7):952-955.
31. Narang P, Agarwal A. Single-pass four-throw technique for pupilloplasty. Eur J Ophthalmol. 2017;27(4):506-508.
32. Kim DB. The next big thing in scleral haptic fixation. Cataract & Refractive Surgery Today. October 2017;17(10):27-36. http://bit.ly/2he1fLv. Accessed October 26, 2017.
33. Henderson BA, Yi DH, Constantine JB, Geneva II. New preventative approach for negative dysphotopsia. J Cataract Refract Surg. 2016;42(10):1449-1455.
34. Geneva II, Henderson BA. The complexities of negative dysphotopsia. Asia Pac J Ophthalmol (Phila). 2017;6(4):364-371.
35. Chee SP, Chan NS. Capsule milking: modification of capsulorhexis technique for intumescent cataract. J Cataract Refract Surg. 2017;43(5):585-589.
36. Daly R. Optical power calculation tools on ASCRS site expands to five. EyeWorld. https://www.eyeworld.org/optical-power-calculation-tools-ascrs-site-expands-five. March 2017. Accessed October 25, 2017.




