Understanding and navigating the increasing complexity of refractive surgery options will ultimately strengthen the refractive surgery market. Modern refractive surgery was born in the late 1980s and 1990s with radial keratotomy. Although this procedure started the revolution of patients seeking independence from glasses and contact lenses to improve their lifestyle, refractive surgery was a relatively rare choice for many people requiring vision correction. Early technology had limitations in terms of its safety, effectiveness, and breadth of patient candidacy, and it became clear early on that there would be a constant desire for improvements to meet patients’ ever-rising expectations.
AT A GLANCE
- Laser corneal refractive surgery has proven successful across a wide range of patients, but it is not ideally suited to patients who need high levels of correction.
- Phakic IOLs are beneficial to some patients, because they can bypass the cornea’s potentially unpredictable healing response. With phakic IOLs, the healing response is independent from the amount of correction desired, allowing for precision and accuracy across the full range of correction.
- Small-incision lenticule extraction has some of the advantages of both phakic IOLs and laser vision correction. Its accuracy does not depend on the desired amount of correction, and it may be less prone to biomechanical and surface concerns than traditional laser vision correction.
Advances have opened new doors by broadening the pool of eligible candidates seeking spectacle independence. There are many options available today to achieve patients’ short- and long-term visual goals, which increases the complexity for providers.
LASER VISION CORRECTION
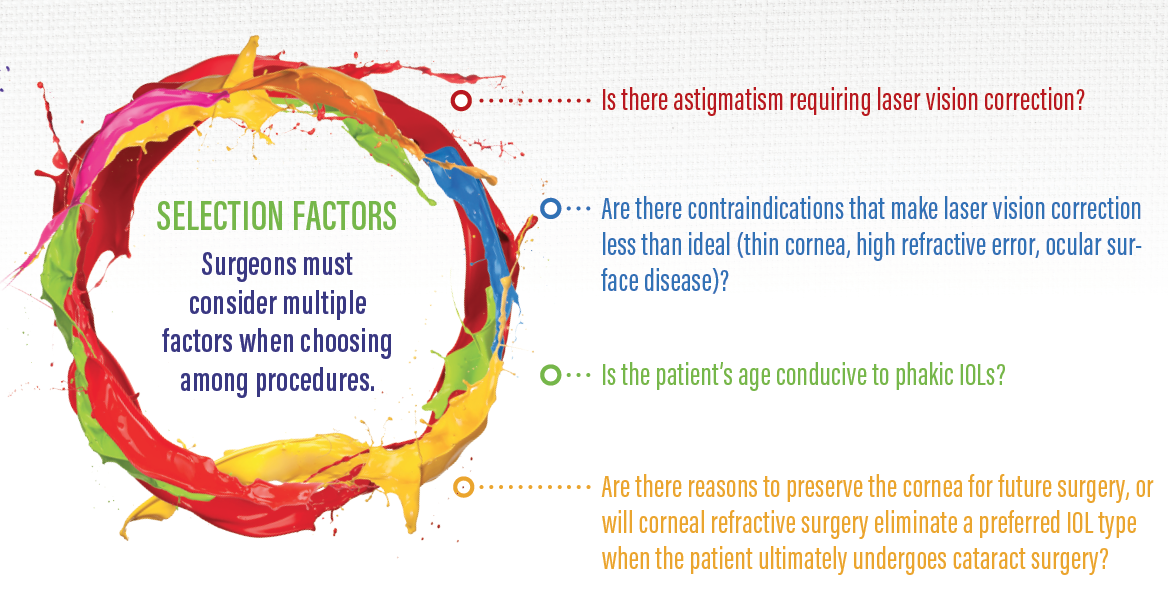
Laser corneal refractive surgery has proven successful across a wide range of patients, but it is not ideally suited to everyone. Laser vision correction (LVC) is quite accurate at low to moderate levels of refractive error. Thankfully, the majority of patients with refractive error are within the low to moderate levels of myopia based on refractive error epidemiology.1,2 LVC is less accurate at high levels of refractive error, however, and the enhancement rates begin to climb.3 Furthermore, higher levels of LVC raise concerns about biocompatibility: a limited amount of tissue can be removed, depending on the starting corneal thickness and desired correction.
Additional concerns are dry eye and ocular surface disease. Because corneal LVC can interfere with corneal innervation, patients at risk of underlying surface pathology may not be suitable candidates for these procedures. Additionally, corneal LVC can have implications for future cataract surgery options; certain IOLs may not be suitable for these eyes.
PHAKIC IOL
The phakic IOL has distinct advantages for a segment of the patient base interested in refractive surgery. Patients with higer degrees of refractive error, corneal surface concerns, and biocompatility concerns can benefit from phakic IOL vision correction. One unique advantage of this technology is that it bypasses the cornea’s potentially unpredictable healing response. The healing response to phakic IOLs is independent from the amount of correction desired, because the correction is applied to the IOL that is inserted and is not a factor of reshaping the cornea. This allows for precision and accuracy across the full range of correction.
Although the phakic IOL requires intraocular surgery that carries inherent risks, in some ways, it is less invasive than corneal refractive surgery, which permanently alters the shape of the eye. Phakic IOLs are removable and replaceable. In theory, once a phakic IOL is removed, the eye’s refractive state returns to its preoperative state.
The relative advantages of phakic IOLs become less clear when applied to low levels of vision correction. LVC is accurate in these cases, because there is less healing response required, and subsequently, nomograms are more accurate. Unless there are surface or biocompatibility concerns, the avoidance of intraocular risks may make corneal LVC the preferred choice for addressing low refraction errors.
Technological limitations are another factor, particularly in the United States, where the newest phakic IOLs are not yet available. Currently, toric models are not available, thus limiting the potential patient base. Many patients have both myopia and astigmatism, so an implantable collamer lens (ICL) may only correct a portion of their refractive error.
In the United States, the current model of the ICL (Visian ICL; STAAR Surgical) requires a peripheral iridotomy (PI) to prevent pupillary block. The PI adds time and expense, and it introduces the potential side effect of glare symptoms originating from the PI. In Europe, the Visian ICL with CentraFlow Technology (STAAR Surgical) has a central port that allows fluids to pass through, eliminating the need for a PI.
James Katz, MD, speaks with Gregory D. Parkhurst, MD, regarding a recent study comparing phakic IOLs with wavefront-guided LASIK for myopia treatment.
SUMMARY
The recent US availability of small-incision lenticule extraction (SMILE) has increased the options for LVC. This procedure may make the decision between LVC and a phakic IOL more complex. SMILE has some of the advantages of phakic IOLs and traditional LVC. Like phakic IOLs, SMILE’s accuracy does not depend on the desired amount of correction, and it may be less prone to biomechanical and surface concerns when compared with traditional LVC.
Although there is increased complexity regarding the choices for vision correction, safety, efficacy, and breadth of candidacy continue to evolve with technological advances. Success across a wider range of patients and refractive error will further strengthen the market, as spectacle independence becomes more the norm than the exception.
1. Vitale S, Ellwein L, Cotch MF, Ferris FL 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126(8):1111-1119.
2. Williams KM, Verhoeven VJ, Cumberland, P, et al. Prevalence of refractive error in Europe: the European Eye Epidemiology (E(3)) Consortium. Eur J Epidemiol. 2015;30(4):305-315.
3. Alió JL, Soria F, Abbouda A, Peña-García P. Laser in situ keratomileusis for -6.00 to -18.00 diopters of myopia and up to -5.00 diopters of astigmatism: 15-year follow-up. J Cataract Refract Surg. 2015;41(1):33-40.