

Posterior polar cataracts always present a challenge to the cataract surgeon due to their propensity to be associated with posterior capsular weakness and posterior capsular rupture (PCR). As techniques, technologies, and surgeons’ understanding of this problem have evolved, PCR rates have dropped from as high as 26% to 36% in the 1990s to between 7% and 8% more recently.1-9
AT A GLANCE
• Femtodelineation creates multiple nuclear layers that act as shock absorbers during surgery.
• The customizable, sharp, predictable layers of cushioning protect the posterior capsule until the end of lens removal.
• he femtodelineation technique can also be useful in posterior polar cataracts with an associated dense nucleus, because there is no need for a mechanical division technique that could stress the capsular-zonular complex.
Since the advent of laser cataract surgery, the use of femtosecond laser technology is increasingly being reported in various challenging situations. In particular, we find this technology to be invaluable in dealing with posterior polar cataracts. Currently, the laser is widely used to create corneal incisions and lens capsulotomies and to perform nuclear division. We recently described the application of a cylindrical lens division pattern in posterior polar cataracts, a procedure we call “femtodelineation” (see Femtodelineation: a New Surgical Technique).10 This technique can enhance safety and reduce PCR rates in surgery for posterior polar cataracts.
The basic principles of emulsification in posterior polar cataract hold true for this technique
• preventing forward bulge of the capsular-zonular
diaphragm
• mechanically cushioning and protecting the weak
posterior capsule
• avoiding sudden, rapid buildup of hydraulic pressure inside the capsular bag
ADVANTAGES IN POSTERIOR POLAR CATARACTS

Figure. Small air bubbles generated by firing of the femtosecond laser, which may not drastically increase intracapsular pressure.
We performed a prospective, observational study in 45 consecutive eyes of 45 patients undergoing cataract surgery for posterior polar cataracts. Using the femtodelineation technique, our PCR rate was 4.4%; that is, two of the 45 eyes had a PCR. Of these, one involved accidental aspiration of the posterior capsule into the aspiration probe during irrigation and aspiration, and in the other, the PCR was noted at the end of nuclear removal. In a previous study, we described the inside-out delineation technique for posterior polar cataract removal,9 and in that report, we had a PCR rate of approximately 9%. Thus, we find the femtodelineation technique offers a lower PCR rate and enhanced safety during surgery in these eyes.
In effect, femtodelineation creates multiple nuclear layers or zones that act as shock absorbers during surgery. These shock absorbers prevent the transmission of mechanical forces and fluidic turbulence to the weakest part of the posterior capsule until the end of surgery. Further, since no hydro-based procedures are involved, the risk for buildup of hydraulic pressure within the bag is eliminated.
One of the biggest advantages of using the laser to create nuclear delineation is that it produces extremely well-demarcated and predictable walls of division. These sharp vertical walls separating the layers from each other make removal easy, requiring minimal mechanical maneuvering with the second instrument.
When the last layer of epinucleus is finally removed, gently stripping it off the fornices around 180º creates a plane of separation between the lens material and the posterior capsule. Because a cleavage is created between the epinucleus and the posterior capsule, passage of fluid into this space will not lead to buildup of hydraulic pressure. Therefore, even if there is a preexisting or intraoperative PCR, there is no or minimal enlargement of this rupture. If there is a PCR, the final goal of being able to implant an IOL in the capsular bag can be achieved by converting this small rupture into a continuous posterior capsulorhexis.
Further, unlike with manual techniques, with femtodelineation, the size, number, and depth of the delineated cylinders can be customized by the surgeon depending on the size of the pupil, the size of the capsulorhexis, or surgeon’s preference.
The femtosecond laser platform is integrated with a live anterior segment OCT that not only shows the status of the posterior capsule but also allows the surgeon to keep a safety margin from the posterior capsule. This ensures that there is no inadvertent damage to the posterior capsule due to collateral effects of the photodisruption created by the laser.
FEMTODELINATION: A NEW SURGICAL TECHNIQUE
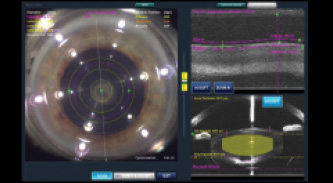
Figure 1. The laser is programmed to create three concentric cylinders in the lens. On the bottom right, anterior segment optical coherence tomography shows the thickness of the lens and the posterior capsule. Based on this information, the surgeon can choose the desired safety margin level so that no collateral damage occurs to the fragile capsule.

Figure 2. At the end of femtodelineation, there are four distinct zones in the lens: three cylinders protected by a thick, uniform cushion of epinucleus.
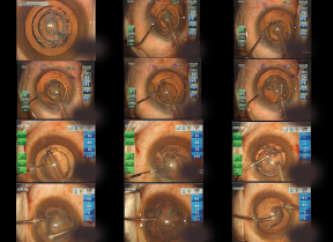
Figure 3. Each layer is emulsified and aspirated. The sharp, demarcated walls allow easy removal with little mechanical manipulation. At the end, a thick, uniform epinuclear layer remains, which is easy to detach.
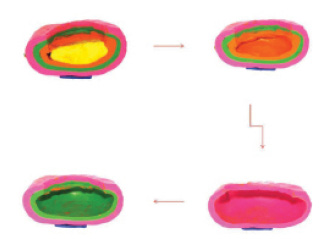
Figure 4. Illustration shows how, as each nuclear layer is removed sequentially, the epinuclear cushion remains, guarding the potentially dehiscent or weak posterior capsule.
We have found that femtodelineation is also useful in posterior polar cataracts with an associated dense nucleus. As the nucleus is already predivided by the laser, it is easily debulked without the need for any mechanical division techniques, which could otherwise cause stress on the capsular-zonular complex.
An added benefit with laser cataract surgery is the ability to achieve a well-centered capsulorhexis of a desired size. This helps to ensure better effective lens position; it can also be useful in the event that ciliary sulcus IOL implantation must be performed.
POTENTIAL CONCERNS
There is a concern regarding elevation of intralenticular pressure due to the bubbles generated during laser application. However, we have found that, with the use of low energy settings and greater laser and spot separation, the bubbles generated are small (Figure). These compliant bubbles may not have the capability to produce a dramatic rise in intralenticular pressure.
Capsular block syndrome, resulting in rupture of the posterior capsule, has been reported in the past with laser cataract surgery. However, as understanding of the technology has improved, surgeons are now more cautious when performing hydrodissection, and recently there have been no more reports of this syndrome.
SUMMARY
Laser technology is especially useful in posterior polar cataracts, as it helps to avoid hydro-based procedures and yet provides customizable, sharp, predictable layers of cushioning that protect the posterior capsule until the end of lens removal.
1. Osher RH, Yu BC, Koch DD. Posterior polar cataracts: a predisposition to intraoperative posterior capsular rupture.
J Cataract Refract Surg. 1990;16:157-162.
2. Vasavada A, Singh R. Phacoemulsification in eyes with posterior polar cataract. J Cataract Refract Surg. 1999;25:238-245.
3. Fine IH. Cortical cleaving hydrodissection. J Cataract Refract Surg. 1992;18:508-512.
4. Masket S. Consultation section. J Cataract Refract Surg. 1997;23:819-824.
5. Allen D, Wood C. Minimizing risk to the capsule during surgery for posterior polar cataract. J Cataract Refract Surg. 2002;28:742-744.
6. Fine IH, Packer M, Hoffman RS. Management of posterior polar cataract. J Cataract Refract Surg. 2003;29:16-19.
7. Lee MW, Lee YC. Phacoemulsification of posterior polar cataracts- a surgical challenge. Br J Ophthalmol. 2003;87:1426-1427.
8. Hayashi K, Hayashi H, Nakao F, et al. Outcomes of surgery for posterior polar cataract. J Cataract Refract Surg. 2003;29:45-49.
9. Vasavada AR, Raj SM. Inside-out delineation. J Cataract Refract Surg. 2004;30:1167-1169.
10. Vasavada AR, Vasavada V, Vasavada S, et al. Femtodelineation to enhance safety in posterior polar cataracts. J Cataract Refract Surg. 2015;41:702-707.
Abhay R. Vasavada, MS, FRCS
• director, Raghudeep Eye Clinic, Iladevi Cataract & IOL Research Centre, Gujarat, India
• member, CRST Europe Global Advisory Board
• icirc@abhayvasavada.com
• financial disclosure: research support from Alcon
Vaishali Vasavada, MS
• consultant ophthalmologist, Raghudeep Eye Clinic, Iladevi Cataract & IOL Research Centre, Gujarat, India
• vaishali@raghudeepeyeclinic.com
• financial disclosure: research support from Alcon


