
Angle alpha is the difference between the center of the limbus and the visual axis. Compared to angle kappa (the difference between the center of the pupil and the visual axis), angle alpha is less well known, but I find it to be very useful for screening premium IOL candidates.
AT A GLANCE
• Good centration of premium IOLs is critical to successful outcomes. If a diffractive multifocal IOL is decentered relative to the visual axis, the patient may look through the diffractive rings rather than through the central optical zone as intended, which can cause deterioration of postoperative visual function due to an induction of higher-order aberrations.
• Many strategies have been proposed for clinically estimating the visual axis and optimizing centration of an IOL.
• The author has made measuring angle alpha a routine part of his preoperative workup for refractive cataract patients. Excluding patients with a high angle alpha, using scanned capsule centration, and implanting a more forgiving multifocal IOL have produced excellent refractive results.
Surgeons know that good centration of premium IOLs is critical. If a diffractive multifocal IOL is decentered relative to the visual axis, the patient may look through the diffractive rings rather than through the central optical zone as intended, which can induce higher-order aberrations and thus decrease postoperative visual function.1 Poor alignment of a toric lens with the visual axis may induce astigmatism, reduce the magnitude of the correction, or otherwise affect quality of vision.
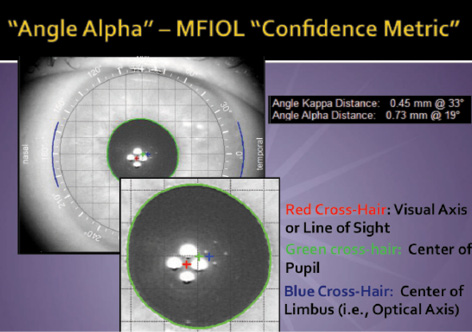
Figure 1. The iTrace measures the distance between the visual axis, as estimated by the center of the first Purkinje reflex (red cross hair), and the center of the pupil (green cross hair), which is useful for LASIK. The angle alpha is the distance from the visual axis to the center of the limbus (blue cross hair), which is useful for IOL implantation.
Many strategies have been proposed for clinically estimating the visual axis and optimizing centration of an IOL. In the presence of a high angle kappa, for example, it is often recommended to deliberately decenter or “nudge” the IOL nasally in order to keep it on the visual axis. It may be impossible, however, to keep an IOL centered on the visual axis if that axis is not closely in line with the anatomical center of the capsule. With current haptic technology, the lens has a tendency to center in the middle of the capsular bag, which is most closely correlated with the center of the limbus. I therefore want to know in advance if the patient’s visual axis and limbal center are poorly aligned, not so that I can shift the implant, but so that I can avoid selecting a multifocal IOL.
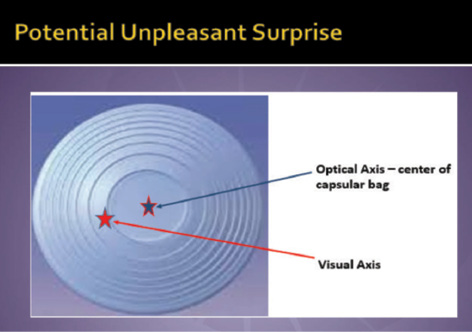
Figure 2. When there is a large (> 0.5 mm) angle alpha, the optical axis/center of the capsular bag may not match the patient’s visual axis, leading to a potentially unpleasant refractive surprise if a multifocal IOL is implanted.
MEASURING ANGLE ALPHA
I have made measuring angle alpha with the iTrace Workstation (Tracey Technologies) a routine part of my preoperative workup for refractive cataract patients (Figure 1). The ray tracing device color-codes the amount of angle alpha. An angle less than or equal to 0.3 mm is green, 0.3 to 0.5 mm is yellow, and greater than 0.5 mm is red. A green angle alpha gives me the greatest confidence that the patient will be looking through the center of the central optic zone, as intended. I will consider implanting some multifocal IOLs when angle alpha is in the yellow zone.
I implant the Tecnis Multifocal +2.75 (ZKB00; Abbott Medical Optics) in about 90% of my multifocal IOL cases. This is in part because, as the FDA data show, the lens offers better intermediate vision and less risk of night vision problems than earlier-generation multifocal IOLs without much sacrifice in functional near vision. The implant is also more forgiving of angle alpha because the central optical zone is larger than that of the ZMB00 (1.3 vs 1 mm). At least in theory, that means that an eye implanted with a ZKB00 lens could have an angle alpha of up to 0.65 mm (half the diameter of that IOL’s central optic zone).
Because I do not want the patient’s visual axis to be right on the edge of the diffractive rings, however, I personally draw the line at the upper limit of the iTrace’s yellow zone for a ZKB00, and I will stay in the green zone for a ZMB00 or an eye with ocular surface problems that might degrade image quality. When angle alpha is in the red zone, I will not implant a multifocal IOL at all (Figure 2).
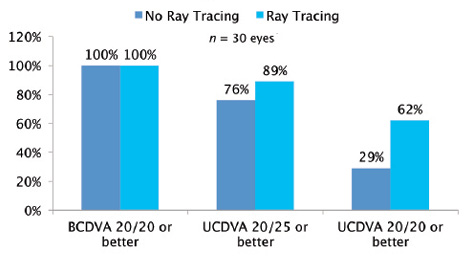
Figure 3. The author’s postoperative distance results with the ZKB00 with and without ray tracing to rule out high angle alpha.
I only use angle kappa for cataract surgery planning in cases where the patient is hyperopic and has both a high angle alpha and a high angle kappa. If the angle alpha is greater than 0.5 mm using the iTrace, I typically avoid premium and aspheric IOLs and instead implant an aberration-free monofocal IOL (eg, SofPort LI6AO [Bausch + Lomb]) for binocular distance vision or monovision. I use the angle kappa—not the angle alpha—measurements for planning hyperopic laser vision correction to ensure that the center of the ablation is aligned with the visual axis rather than the center of the pupil.
If the patient has a low angle alpha, I like to maximize the IOL’s alignment on the visual axis by using the scanned capsule centration mode on the Catalys Precision Laser System (Abbott Medical Optics). William Wiley, MD, has shown that scanned capsule centration achieves better results than pupillary centration.2
CONCLUSION
In my experience, excluding a high angle alpha, using scanned capsule centration, and implanting the ZKB00 multifocal IOL have produced excellent refractive results (Figure 3). With this method, the IOL always looks very nicely aligned on the visual axis and pupil when I am examining the patients at the slit lamp postoperatively. Taking these steps to better predict lens alignment with the visual axis has helped me achieve better visual quality and high rates of satisfaction for my premium IOL patients.
1. Park CY, Oh SY, Chuck RS. Measurement of angle kappa and centration in refractive surgery. Curr Opin Ophthalmol. 2012;23(4):269-275.
2. Wiley WF, Bafna S, Jones JJ. Optical coherence topography-guided capsule bag-centered femtosecond laser capsule. Paper presented at: 2013 ASCRS/ASOA Symposium & Congress; April 9-14, 2013; San Francisco, CA.
Asim R. Piracha, MD
• medical director of John-Kenyon Eye Center in Louisville, Kentucky
• associate professor at the University of Louisville’s Department of Ophthalmology and Visual Sciences
• (502) 895-2910; apiracha@johnkenyon.com
• financial disclosure: has received speaking fees from Abbott Medical Optics


