CASE PRESENTATION
A healthy 27-year-old woman with a long history of rigid gas permeable contact lens use presents with reduced vision, worse in the left than right eye. The patient is a competitive equestrian. She states that the contact lenses are difficult to wear because of the dust and dirt in the air during competition, and she would like to know if there is anything she can do to become less dependent on contact lenses.
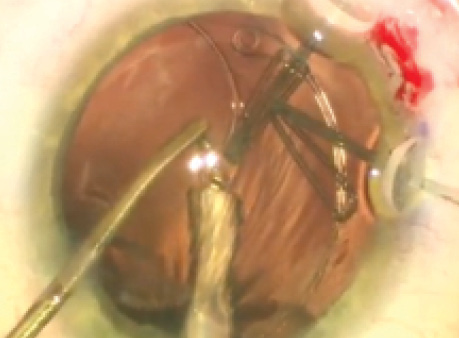
Upon examination, the patient’s visual acuity is 20/40 OD and 20/400 OS with her glasses in place. With a refraction of -10.00 + 3.50 × 090, the visual acuity in the patient’s right eye remains 20/40, but the left eye refracts to 20/70 with -15.50 + 3.00 × 085. The pupils are normal with no afferent pupillary defect, and the external examination is normal. A slit-lamp examination of the anterior segment is normal, with the exception of bilateral subluxation of the crystalline lenses. Examinations of the retina and optic nerve are normal (Figures 1-4).
How would you manage this patient’s cataract(s) and her request to be independent of contact lenses?
—Case prepared by Brandon D. Ayres, MD.

Figure 1. A clinical examination of the patient’s left eye shows superonasal subluxation of the crystalline lens.
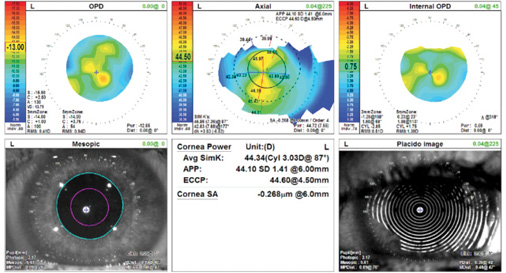
Figure 2. Topography.
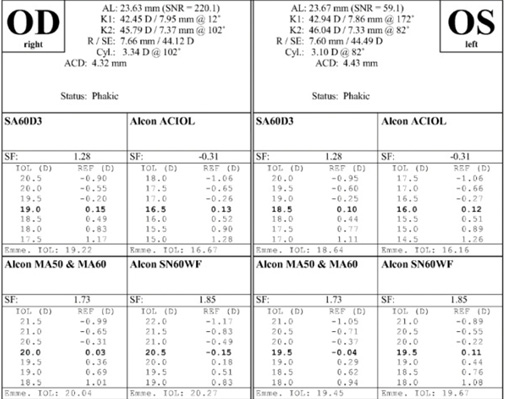
Figure 3. Measurements with the IOLMaster (Carl Zeiss Meditec).
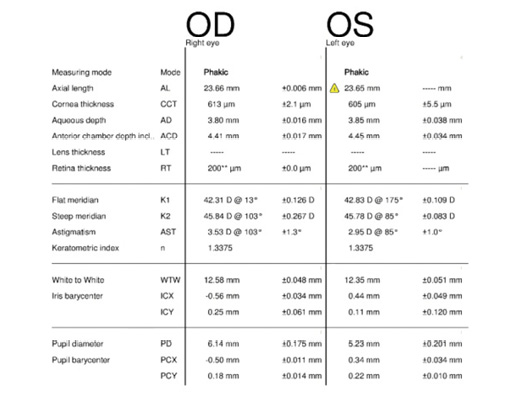
Figure 4. Measurements with the Lenstar (Haag-Streit).

KENNETH A. BECKMAN, MD
In my opinion, the surgeon’s primary responsibility in cases like this one is to safely remove the lens and place an IOL that provides the best possible vision. The patient’s goal of being free of contact lenses is secondary. Ordinarily, my first thought is to identify the etiology of the subluxated lens. Is there an underlying disorder that may carry other health risks such as Marfan syndrome? For the purposes of this discussion, I will assume that this evaluation has already taken place.
Although it is tempting to try to salvage the capsule to permit the placement of an IOL in the bag, capsular tension rings (CTRs) do not last indefinitely in my experience. I do not believe that an IOL could be safely implanted in the bag with a CTR and remain in place for the duration of this young patient’s life without suturing either the IOL or the CTR. There is a high likelihood of vitreous loss, and this patient is a high myope and thus at increased risk of retinal detachment. I would therefore choose to keep matters simple.
I would have a retina surgeon perform a pars plana vitrectomy and lensectomy. In an older patient, I would consider placing an anterior chamber IOL. Because this patient is only 27 years old, I would consider suturing a posterior chamber IOL. Dr. Ayres shared with me an elegant approach to suturing the Akreos IOL (Bausch & Lomb),1 and I think this procedure would be the simplest and least traumatic option for the eye. Certainly, other posterior chamber IOLs can be sutured as well.
The next decision relates to IOL power. Because I would not choose a toric IOL, I know there will be residual astigmatism, which can be treated postoperatively. Although the patient is interested in remaining independent of contact lenses, there are not many options. Because the patient is young and has not yet developed presbyopia, I would discuss the option of monovision versus full distance correction and the need for readers postoperatively.
It would be important to bear in mind that this patient has had a very high refractive error and has never been able to function without contact lenses or thick glasses. Even if her refractive error is not fully corrected with these surgeries, she will notice a dramatic improvement. She may then be able to wear a weak pair of glasses or perhaps a soft contact lens that is more tolerable.
Although I understand that this patient has expectations and goals, it is the duty of the surgeon to make the decision that is in the patient’s best interest. It is tempting to try to cure everything in one swoop, but this is not always possible. There is nothing wrong with telling the patient no.

DAVID A. GOLDMAN, MD
This case is complex due to the bilateral lens subluxation. Fortunately, although the patient has significant astigmatism, it appears to be regular on topography, although there is some dropout on the scan, likely secondary to dryness. After a detailed history, including any patching/amblyopia, I would further evaluate the patient for visual potential and any evidence of amblyopia. This could include pinhole acuity testing, a potential acuity meter, or even an electroretinogram. Assuming no amblyopia, surgery is the only option to improve her visual acuity.
My surgical approach would be to stabilize the capsular bag during capsulorhexis with the Mackool Cataract Support System (FCI Ophthalmics). With four hooks in, the bag should be sufficiently stable for me to perform traditional phacoemulsification. I would implant an enVista lens (MX60; Bausch + Lomb) because of its zero asphericity and the significant possibility that the IOL will not be perfectly centered postoperatively. I would also place a Cionni Ring for Scleral Fixation (Morcher, distributed in the United States by FCI Ophthalmics), and I would fixate the bag-lens complex to the sclera with a Gore-Tex suture (W.L. Gore & Associates; off-label use).
Because the patient has thick corneas, I would target some myopia to make postoperative laser vision correction consume less tissue. LASIK or PRK would be options for this patient, and I would prefer to treat her refractive error rather than her topographical astigmatism. A toric lens could be implanted, but suturing it to perfect centration and axial position would be highly challenging. Furthermore, predicting the effective lens position in patients such as this one can be less accurate than in traditional cataract surgery, and spherical error can also be treated postoperatively with a laser.

KATHRYN M. HATCH, MD
The subluxation of the crystalline lenses increases the complexity of the surgical approach. In a classic case of with-the-rule astigmatism and bilateral cataracts, my typical approach would be the sequential placement of a toric IOL guided by intraoperative aberrometry, with the eyes treated 1 week apart to minimize anisometropia between surgeries. Given the zonular compromise in this case, traditional approaches may not be impossible, but they certainly would be more difficult than usual.
I would address this case in a staged fashion: cataract surgery followed by astigmatism management. Given the size of the zonular dehiscence, I would address the astigmatism on the corneal plane rather than at the lens. I believe that the excimer laser will manage the astigmatism more predictably than attempting to center a toric IOL in a potentially unstable capsular bag. Even a small amount of axial decentration when correcting more than 3.00 D of cylinder could cause large refractive shifts, with a resultant over- or undercorrection of astigmatism.
I would perform laser cataract surgery with capsulotomy construction to minimize strain on the compromised zonules. I would employ techniques to stabilize and center the capsule as necessary, including the use of a CTR and one or two sclera-fixated Ahmed Capsular Tension Segments (Ahmed CTSs; Morcher, distributed in the United States by FCI Ophthalmics), depending on the size of the zonular dehiscence. I would place a one-piece IOL in the capsular bag. Once the first eye healed, I would perform surgery on the other eye with a similar technique.
I would address astigmatism management in both eyes 2 to 3 months after cataract surgery so as to allow resolution of inflammation, any necessary ocular surface management, and a YAG capsulotomy for any posterior capsular opacification. I would then proceed with laser vision correction, either LASIK or PRK.

W. BARRY LEE, MD
Before considering treatment, it would be important to consider the differential diagnosis. Of the various causes, homocystinuria must be ruled out due to its potentially lethal implications from thrombotic events. After the workup, the next decision is whether an anterior or posterior segment approach will be better. I prefer a pars plana lensectomy to remove the lens. The surgery can be performed simultaneously or staged with a retinal surgeon. Performed well, this technique will minimize the risk of retinal complications.
Because the patient is intolerant of contact lenses, she will also likely be intolerant of aphakic contact lenses, making IOL implantation a must. Options include the scleral fixation of an IOL with glue or with 9–0 Prolene (Ethicon) or 8–0 Gore-Tex (off label), because an anterior chamber IOL is contraindicated in a patient this young. I would construct a superonasal near-clear incision for implantation of the IOL and create Hoffman pockets at 1 and 7 o’clock for fixation of the sutures.
The peripheral corneal incision used to initiate the pocket formation would act as a limbal relaxing incision and reduce some of the with-the-rule astigmatism. I typically use a CZ70BD lens (Alcon), which has eyelets for fixation of the IOL to the sclera, and a refractive target of -1.00 to -1.50 D. Once the eye healed, the sutures had been removed from the superonasal incision, and the refraction had stabilized, a PRK procedure could be performed to reduce any residual refractive error from the small amount of myopic astigmatism remaining.

WHAT I DID: BRANDON D. AYRES, MD
After a long discussion with the patient, we decided to attempt cataract removal with suture fixation of the capsular bag and the placement of a toric IOL to help reduce her dependence on spectacle correction.
One of the most critical and challenging steps of surgery is creating a continuous curvilinear capsulorhexis. To simplify this step, I used a laser to make the capsulotomy. I created small arcuate incisions to facilitate alignment of the toric IOL. Thereafter, the patient was prepared for removal of the cataract.
Before entry into the anterior chamber, I marked the estimated location of where the Ahmed CTS would be sutured, and I constructed a 4 × 3-mm scleral pocket with a crescent blade and marked out the borders of the pocket using a gentian violet marker.
The capsulotomy was removed and a small viscodissection performed to facilitate placement of capsular support hooks. Because the patient was young, I was able to remove the lens entirely with a bimanual I/A system. Next, I carefully placed a CTR and removed the capsular support hooks. The toric IOL was then placed and rotated to just a few degrees shy of the intended axis.
I used a microvitreoretinal blade to create two transconjunctival sclerotomies through the scleral pocket and into the sulcus space. I then laced a Gore-Tex CV-8 suture (W.L. Gore & Associates; off-label use) through an Ahmed CTS, recovered the suture ends in the anterior chamber, and externalized them on the conjunctival surface. The Gore-Tex suture was recovered through the pockets and tied, allowing centration of the IOL-capsular bag complex. After fixation, the remainder of the viscoelastic was removed, and the IOL was rotated to the intended axis. I sutured several of the corneal incisions for safety.
The patient did very well postoperatively. Her UCVA improved to 20/30 on postoperative day 1 and to 20/25 by 1 month. A few weeks later, her second eye was treated in a similar fashion, leaving her with a bilateral UCVA of 20/25.
1. Fass ON, Herman WK. Sutured intraocular lens placement in aphakic post-vitrectomy eyes via small-incision surgery. J Cataract Refract Surg. 2009;35(9)1492-1497.
Section Editor Lisa Brothers Arbisser, MD
•emeritus position at Eye Surgeons Associates, the Iowa and Illinois Quad Cities
•adjunct associate professor, John A. Moran Eye Center, University of Utah, Salt Lake City
Section Editor Brandon D. Ayres, MD
•surgeon in the Cornea Service, Wills Eye Hospital, Philadelphia; (484) 434-2700; bayers@willseye.org
•financial disclosure: consultant to and on the speakers bureau for Alcon
Section Editor Audrey R. Talley Rostov, MD
•private practice with Northwest Eye Surgeons, Seattle; SightLife global partner
Kenneth A. Beckman, MD
•director of corneal services, Comprehensive EyeCare of Central Ohio, Westerville, Ohio
•clinical assistant professor of ophthalmology, The Ohio State University, Columbus
•president of CEDARS
•(614) 890-5692; kenbeckman22@aol.com; Twitter @KenBeckmanMD; financial disclosure: consultant to Bausch + Lomb
David A. Goldman, MD
•private practice, Goldman Eye, Palm Beach Gardens, Florida; (561) 630-7120; david@goldmaneye.com
•financial interest: none acknowledged
Kathryn M. Hatch, MD
•member of the faculty in ophthalmology, Harvard Medical School, Massachusetts Eye and Ear Infirmary, Waltham, Massachusetts
•(781) 890-1023; kathryn_hatch@meei.harvard.edu; financial interest: none acknowledged
W. Barry Lee, MD
•partner, Eye Consultants of Atlanta
•co-medical director, Georgia Eye Bank, Atlanta; lee0003@aol.com
•financial interest: none acknowledged