
Since opening my practice in Las Vegas in 2013, I have offered patients a full spectrum of surgical options, including premium IOLs and femtosecond laser procedures. The number of laser cataract surgeries I performed had been increasing, because patients are attracted to the concept. I have to admit, however, that my own recommendation of the procedure was not particularly strong.
AT A GLANCE
• The author’s ambivalence toward laser cataract surgery changed when she began to see a big difference in how well OCT imaging helped her prepare for surgery and in the outcomes she could achieve with the laser system.
• The laser system helps identify tilt, which has meant a more consistent capsulorhexis and better lens fragmentation.
• The laser has improved the author’s results with the Crystalens. Her patients who receive the lens after laser surgery seem to fare better than those who get the implant after standard cataract surgery.
This all changed when I started using a new laser system in September 2014. I noticed a big difference in how well the imaging capabilities of the Catalys Precision Laser System (Abbott Medical Optics) helped me to prepare for surgery. I also saw a real improvement in the outcomes I could achieve through better centration of presbyopia-correcting IOLs and my correction of astigmatism. The Catalys is one of three laser platforms that I have used.
My laser cataract conversion rate has risen from 9% in the first 3 quarters of 2014 to 32% in the first 3 quarters of 2015, due in large part to the shift in my own convictions (Figure 1). I am so busy performing the laser cases that I hired an associate to perform some of my standard cases. Because I am more comfortable offering premium IOLs and incisional astigmatism correction, my volume of those pro- cedures has also increased.
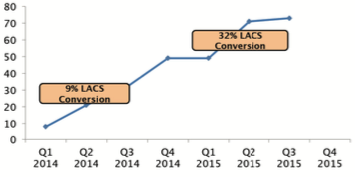
Figure 1. Change in the author’s average monthly laser cataract (LACS) volume and conversion rate over a 2-year period.
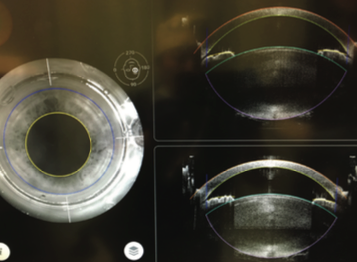
Figure 2. In addition to nuclear density, it is helpful to know in advance if the lens volume is unusually large, as in this case.
BETTER PREPARED
It quickly became apparent to me that high-quality opti- cal coherence tomography (OCT) imaging, particularly when I am given multiple views, provides critical insights for surgery. Surgeons who have performed cataract surgery for a long time may be inclined to dismiss OCT imaging as unneeded information. Once I started to use it, however, I began to appreciate the advance warning of shallow cham- bers, peripheral corneal thinning, or unusually large lenses (Figure 2). Pathology that might be too subtle to detect dur- ing an examination can often be identified at the laser prior to entering the eye.
As a cataract surgeon, I look at the crystalline lens primar- ily from the top down, visualizing it from the anterior sur- face. Yes, I know it has depth as I sculpt or chop the lens, but I did not have a full appreciation of the 3-D structure until I started seeing it routinely in cross-section at the laser. Three-dimensional OCT imaging has changed the way I think of a lens, and it always better prepares me for the OR.
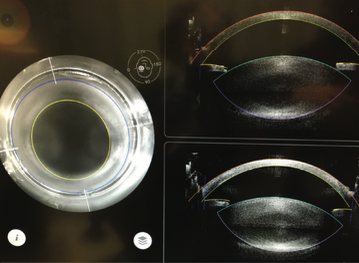
Figure 3. With both axial and sagittal views of the lens, tilt is easily seen and accounted for, providing consistent free capsulotomies and excellent fragmentation.
I also find that having both an axial and a sagittal view of the lens helps me to identify tilt (Figure 3). Accounting for tilt during the laser treatment has meant a more consistent capsulorhexis and better lens fragmentation. Presoftening and/or segmenting the lens with the laser has made the ultrasound portion of the procedure more efficient, with less energy used in the eye, which I find especially valuable with dense nuclei.
IMPROVED OUTCOMES IN PRESBYOPIA
I see a significant amount of retinal pathology in my patient population, making many of them poor candidates for multifocal IOLs. In the past, I was not satisfied with the results of my manual limbal relaxing incisions, so my premium cases consisted mostly of toric IOLs and some accommodating lenses.
Refractive predictability depends on effective lens posi- tion. To me, one of the most exciting features of the Catalys is the “scanned capsule” function, which gets me one giant step closer to reproducible effective lens posi- tion. Based on the OCT measurement of the natural lens, the computer calculates the anatomical center of the lens and centers the capsulotomy based on that point. This is simply something I cannot do without imaging, since the pupillary center does not necessarily line up with the ana- tomical center.
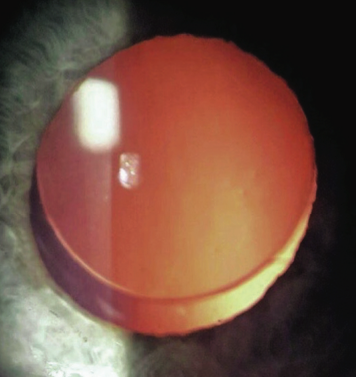
Figure 4. The center of the lens/capsule is not always aligned with the center of the pupil. A scanned capsule capsulotomy can better position the lens on the patient’s visual axis.
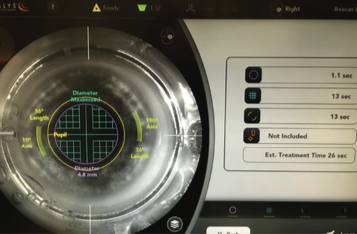
Figure 5. Laser capsulotomy speed is very fast. In this case, the cataract incisions would have interfered with paired laser arcuate incisions, so the author elected to create them manually. She also manually creates incisions in eyes with a history of radial keratotomy.
This computerized scanned capsule centering function has been crucial to my success with the Crystalens (Bausch + Lomb), because its hinged haptics demand good centra- tion for adequate lens function. I have now seen many cases where the scanned capsule capsulotomy differs signif- icantly from where the pupil-centered capsulotomy would have been placed (Figure 4), and I suspect that this could be one reason for patients’ better near function with this lens. I counsel patients that they will need reading glasses for small print, but I often see better reading results in patients who have received a Crystalens after laser cataract surgery versus a standard procedure.
Currently, my laser settings are optimized to reduce the capsulotomy speed down to approximately 1 second (Figure 5), which is faster than any other femtosecond laser platform that I have used. I find that this speed gives me reliable reproducibility and facilitates the treatment of intumescent white cataracts.
The precision of laser arcuate incisions makes more of my patients candidates for multifocal IOLs, even if they have visually significant astigmatism. Some surgeons may believe their manual relaxing incisions are as good as the laser’s, but I can say unequivocally that the laser makes more consistent and reproducible arcuate incisions than I can perform manually.
EDUCATING PATIENTS
Patients in my practice have two decisions to make before cataract surgery: how they want the surgery done (standard or laser) and what kind of lens they want. Should they have visually significant astigmatism, they may choose the laser method with or without a presbyopia-correcting IOL.
There are multiple moments in the practice when this education happens. I believe that it is important for patients to hear about risks and benefits in different ways, because people have different learning styles. My practice uses video, print information, verbal explanations, and eye models so that patients can make well-informed decisions about their eye surgery.
CONCLUSION
I am confident that manufacturers will continue to improve laser platforms. I believe that it is worth surgeons’ time to explore the advantages of laser cataract surgery. I have found it to be extremely rewarding for both my patients and me. It was only when I became convinced of the technology’s advantages that my enthusiasm really resonated with my staff and patients.
Eva Liang, MD
• medical director of Center for Sight in Las Vegas
• (702) 724-2056; eva.liang@c4slv.com
• financial disclosure: consultant to Abbott Medical Optics and Bausch + Lomb


