A 66-year-old man is referred to you for anisometropia after a scleral buckling procedure for a retinal detachment in his pseudophakic right eye. The manifest refraction is -4.50 +1.00 × 145 OD and -1.50 +0.75 × 160 OS. The examination is remarkable only for an irregular pupil in the right eye, and the patient underwent YAG capsulotomy in both eyes after cataract surgery (Figures 1 and 2).
The patient has tried but been unable to tolerate glasses and contact lenses. He presents to you for resolution of his anisometropia.
—Case prepared by Karl G. Stonecipher, MD
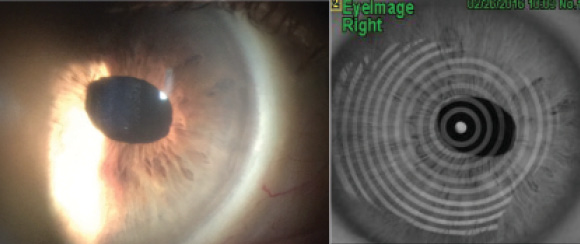
Figure 1. A slit-lamp examination shows a nasally decentered pupil after retinal detachment surgery.
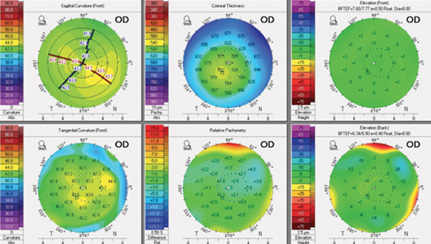
Figure 2. Corneal tomographic image.

WILLIAM B. TRATTLER, MD
A variety of options can be considered for a pseudophakic patient with an open capsule who has developed significant myopia following a scleral buckle. Such individuals may be happy with their current vision and prefer wearing glasses or contact lenses as needed. If not, possibilities include surface ablation, LASIK, or a piggyback IOL. An IOL exchange would be lower on my list because of the open posterior capsule.
In this case, I would recommend laser refractive surgery, either PRK or LASIK, with a target of good distance vision in the right eye. A piggyback IOL carries a similar level of risk as PRK or LASIK, so this intraocular procedure could also be considered. A piggyback IOL would not address the horizontal astigmatism, however, so I would expect PRK or LASIK to provide better UCVA postoperatively.
Of note, the pupil is only mildly decentered, so the patient should do very well with PRK, LASIK, or a piggyback IOL, without requiring surgical revision of the pupil.

DAVID R. HARDTEN, MD
It is not uncommon for patients to experience anisometropia after a retinal detachment repair. If this patient is happy with the monocular BSCVA in his right eye (ie, the irregular pupil is not causing symptoms on its own), then I would proceed with laser vision correction in that eye. In patients who are 60 years of age and older, the epithelium is often loose, so I would perform PRK in this case. Wavefront-guided ablation probably is not possible because of the IOL, retinal irregularity, and irregular pupil, and in patients with somewhat decreased BCVA, it is not critical; standard treatment would likely be satisfactory. In patients with significant anisometropia who have high myopic or hyperopic refractive errors, a piggyback IOL is another option, but at this level of myopia, my preference would be PRK.

ARTHUR B. CUMMINGS, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin)
I would address the anisometropia by means of PRK or other surface ablation with mitomycin C in order not to disturb the retinal detachment surgery or scleral buckle. I would perform a topography-guided procedure in which the ablation was automatically centered on the corneal apex. Another option would be a wavefront-optimized or aberration-free profile with the ablation centered either on the corneal apex or 75% between the pupillary center and corneal apex (aiming closer to the apex). This patient has had surgery but not refractive surgery, so I would imagine that he could undergo a primary refractive procedure with Contoura Vision (Alcon) in the United States. Given his age, I would first verify that the tear film was healthy and stable, especially if I were going to employ topography in the generation of the ablation profile.

JERRY TAN, MBBS(S’pore), FRCS(Edin), FRCOphth, FAMS
One important consideration is that excimer lasers ablate tissue with reference to the pupillary center. In this case, the pupil is oval and decentered nasally. Before considering treatment, I would place the patient under the laser to see if the eye tracking were accurate and reliable. If not, the treatment could be badly decentered. Interestingly, the pupil appears almost round in Figure 2 versus obviously oval in Figure 1. The pupillary outline must be accurately defined if a topography-guided treatment is used.
The manifest astigmatic refraction is consistent with topography in terms of both axis and power. My preference would be a topography-guided treatment that was centered on the corneal vertex (by default). I would use the largest optical zone so as to cover the scotopic pupil. Fortunately, based on the history provided, this patient does not have a multifocal IOL, which would cause additional problems such as coma from the decentered pupil. If he has a nonaspheric IOL, there is an excellent chance that he will achieve very good vision after topography-guided LASIK.
A noncorneal alternative would be a piggyback toric IOL like the Sulcoflex toric lens (Rayner Intraocular Lenses), which is designed to be placed in the sulcus. There are inherent risks to intraocular surgery, however, in a patient who has had retinal detachment surgery. There is also a risk of malrotation of a toric sulcus lens for this piggyback IOL.1
If the eye tracker could follow the pupil well, the refraction were stable, and the cornea had fully healed, I would perform topography- or corneal wavefront-guided LASIK surgery using the largest optical zone safely possible at least 6 months after his last operation. Using a femtosecond laser, I would create a thin flap that avoided any corneal incisions.
1. McGrath LA, Lee GA. Transscleral fixation of a supplementary toric intraocular lens to prevent rotation in a pseudophakic patient. J Cataract Refract Surg. 2013;39(1):134-138.
Section Editor Alan N. Carlson, MD
• professor of ophthalmology and chief, corneal and refractive surgery, Duke University Eye Center, Durham, North Carolina
Section Editor Stephen Coleman, MD
• director of Coleman Vision, Albuquerque, New Mexico
Section Editor Karl G. Stonecipher, MD
• clinical associate professor of ophthalmology, University of North Carolina, Chapel Hill
• director of refractive surgery, TLC in Greensboro, North Carolina
• (336) 274-2244; stonenc@aol.com
Section Editor William F. Wiley, MD
• private practice at Cleveland Eye Clinic, Cleveland, Ohio
Arthur B. Cummings, MB ChB, FCS(SA), MMed(Ophth), FRCS(Edin)
• consultant ophthalmologist, Wellington Eye Clinic and Beacon Hospital, Dublin, Ireland
• abc@wellingtoneyeclinic.com; Twitter @cummingsab
• financial disclosure: consultant to Alcon and WaveLight
David R. Hardten, MD
• director of clinical research and cofounder, Minnesota Eye Consultants, Minneapolis
• (763) 746-7211; drhardten@mneye.com
Jerry Tan, MBBS (S’pore), FRCS (Edin), FRCOphth, FAMS
• consultant ophthalmologist, Jerry Tan Eye Surgery, Singapore
• +65 6738 8122; jtaneyes@singnet.com.sg; jerrytaneyesurgery.com
• financial disclosure: consultant to Schwind eye-tech solutions
William B. Trattler, MD
• director of cornea, Center of Excellence in Eye Care, Miami
• (305) 598-2020; wtrattler@earthlink.net; Twitter @wtrattler


