By Dan Z. Reinstein, MD, MA(Cantab), FRCSC, DABO, FRCOphth, FEBO
This year marks the 10th anniversary of the first lenticule extraction procedure performed using the VisuMax femtosecond laser (Carl Zeiss Meditec) and 7 years since the introduction of small-incision lenticule extraction (SMILE). This article summarizes some recent advances in technique.
OUTCOMES
In January 2016, the first long-term study was published, reporting outcomes 5 years after surgery. It showed no significant change to the 6-month outcomes and no loss of 2 lines of corrected distance visual acuity (CDVA).1 The long-term results of SMILE are thus similar to those of LASIK, as would be expected, given that both procedures involve the removal of stromal tissue and the 1-year outcomes are comparable.2
The results of these early SMILE populations should be considered in context. These were among the first eyes ever treated, so they reflect the procedure in its original form. Specifically, since then, the following improvements have been made:
• The laser energy and spot-spacing settings have been optimized.
• The 250-kHz laser has been upgraded to 500 kHz.
• Surgical technique and instruments have improved with time and experience.
• User nomograms for SMILE have been applied and adopted by many surgeons.
These enhancements are reflected in the increasing number of articles reporting excellent outcomes after SMILE during the past year,2-7sup>n> including large populations of 772 and 1,396 eyes.3
TREATMENT RANGE
Myopia
One question often asked about SMILE is whether it can be used for low myopia, which would mean a very thin and unmanageable lenticule. Most surgeons are successfully performing SMILE for low myopia by increasing the lenticule’s thickness to a manageable level through expansion of the optical zone, which also has the benefits associated with large optical zones. Sri Ganesh, MBBS, MS, DNB, described the use of a lenticule at least 20 to 30 µm thick, which further improves visual recovery, but patients are also doing well with the current FDA trial’s protocol of 15 µm (data on file with Carl Zeiss Meditec). My colleagues and I have published SMILE results for low myopia comparable to those of LASIK,8 and Ang et al9 have shown no difference in outcomes between myopia below and above -5.00 D.
Using SMILE to treat high myopia has potential advantages, owing to the conservation of the anterior stroma. In a recent study comparing the treatment of moderate and high myopia, Kim et al5 showed equivalent refractive accuracy between groups.
Hyperopia
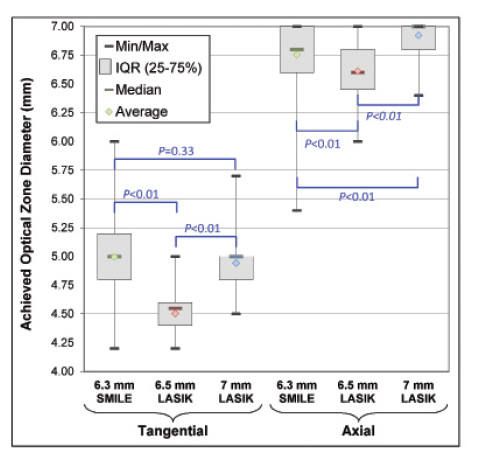
Figure. Box plots of the achieved optical zone diameter based on both tangential and axial curvature difference maps for SMILE with a 6.3- to 6.7-mm programmed optical zone compared with matched LASIK controls with both a 6.5- and a 7-mm programmed optical zone.
The first phase of the second trial of femtosecond lenticule extraction for hyperopia has been completed and was published by Sekundo et al.10 We demonstrated an improvement over the first trial11 by redesigning the profile, expanding the optical zone, and adding a large transition zone. I am currently running the first study of SMILE for hyperopia in conjunction with my colleague Kishore Pradhan, MD, at the Tilganga Institute of Ophthalmology in Kathmandu, Nepal. We presented the early results at The Association of Research in Vision and Ophthalmology’s annual meeting this year.12
In brief, using a 6.3-mm optical zone and a 2-mm transition zone in 58 eyes, we found that, 3 months after surgery, (1) the achieved optical zone on topography was actually larger than that for LASIK using the MEL 80 (Carl Zeiss Meditec) with a 6.5-mm optical zone and equivalent to a 7-mm optical zone and (2) centration was not different from that with LASIK (Figure). The difference in achieved topographic optical zone might be due to the elimination in SMILE of two types of error: fluence projection (because the majority of the ablation is performed peripherally, these errors are increased for hyperopic LASIK compared with myopic LASIK) and truncation (ie, part of the excimer laser ablation might be applied outside the diameter of the flap, leading to truncation).
Watch it Now
Joaquín Fernández, MD, provides a step-by-step explanation of small-incision lenticule extraction.
In a subanalysis of 31 sighted eyes (CDVA 20/40 or better), we found that refractive accuracy and safety at 3 months were similar to those of matched LASIK controls (efficacy was not compared because of the difference in CDVA between groups). These results are encouraging, and we plan to start hyperopic SMILE treatments in London soon.
RETREATMENT OPTIONS AFTER SMILE
How to perform a retreatment after SMILE is often the first question that I am asked. I prefer thin-flap LASIK. My protocol for the primary SMILE procedure is to use a cap thickness of at least 135 µm, which leaves the stronger anterior stroma and corneal nerve plexus untouched. The epithelium will have thickened centrally after a myopic correction to partially compensate for the tissue that has been removed, but the epithelium will not be thicker than approximately 80 µm.13 As a result, there will be a gap between 80 and 135 µm in which to make a flap. Because the standard deviation in the flap’s thickness with the VisuMax is 4.4 µm,14 if I aim for a 100-µm flap, then it will be more than four standard deviations away from both the epithelium and the existing SMILE interface (even if the SMILE interface is more superficial than intended). In reality, this approach is even safer, because I measure both the epithelial thickness and the SMILE cap’s thickness with optical coherence tomography and very high-frequency digital ultrasound, so I can plan how thick to make the flap based on direct measurements.
Earlier this year in a case report, David Donate, MD, described an interesting new method that allows a retreatment to be performed as SMILE.15 The second SMILE procedure is set to the depth of the original, but the laser ablation is stopped midway through after creating the lower lenticule interface and lenticule sidecut. In this way, the existing cap interface acts as the upper interface of the lenticule, and the surgeon can use the existing small-incision tunnel to dissect and extract this second lenticule. If the results continue to be as promising as in this case report, then this method may well become the standard for retreatments after SMILE.
OTHER APPLICATIONS FOR SMILE
Some surgeons are combining SMILE with corneal collagen cross-linking for cases of forme fruste keratoconus, with results on 15 eyes reported by Graue-Hernandez et al.16 This is an interesting way of improving on the Athens protocol, and the published results are promising. The jury is still out, however, on the long-term safety of removing tissue from keratoconic eyes. SMILE has also been reported after deep anterior lamellar keratoplasty.17
Another area of research involves implanting lenticules to treat hyperopia or keratoconus. Although intriguing, initial studies have shown a large undercorrection of the effect when trying to treat hyperopia.18For keratoconus, the idea is that implanting a lenticule can increase the stromal thickness in the region of the cone and thus help to regularize the cornea.
Soosan Jacob, MS, FRCS, DNB, has developed the presbyopic allogenic refractive lenticule (PEARL) inlay. This procedure involves creating a corneal inlay by cutting a button from a SMILE lenticule using a trephine. This clever idea certainly would be an improvement over any synthetic inlay in terms of biocompatibility. The procedure intentionally creates a central island in order to have a central steep zone for near vision in the same way as the Raindrop Near Vision Inlay (ReVision Optics). This is also the goal of many multifocal corneal approaches as well as Intracor (Technolas Perfect Vision). I would therefore expect results with the PEARL inlay to be similar to those of synthetic inlays and these other procedures, because the PEARL inlay is using the same mechanism and because central islands are associated with a reduction in quality of vision and a reduction in safety. I anticipate that some patients will be extremely happy, because they will get distance and near vision and be able to adapt to the multifocality. As with any multifocal approach, however, I expect that a percentage (and not a small one) of patients may be unhappy with their quality of vision. Other factors to consider are the extra time and cost involved in transplanting human corneal tissue, which in Europe involves a huge amount of regulatory and administrative effort.
THE FUTURE
Outcomes continue to improve as the community of SMILE surgeons expands and shares knowledge. The treatment range is now established from low to high myopia, and studies are planned to extend it above -12.50 D. Efforts are also underway to include the treatment of hyperopia and mixed astigmatism as well as to add asphericity to the myopic lenticule profile. In addition, surgeons are developing more applications for the procedure.
For these reasons, SMILE has become an integral part of my practice, although I view the procedure as complementary to LASIK. There are still patients whom I deem more suitable for LASIK, and others may need therapeutic treatment options offered by an excimer laser.
1. Blum M, Taubig K, Gruhn C, et al. Five-year results of small incision lenticule extraction (ReLEx SMILE) [published online ahead of print January 8, 2016]. Br J Ophthalmol. doi:10.1136/bjophthalmol-2015-306822.
2. Pradhan KR, Reinstein DZ, Carp GI, et al. Quality control outcomes analysis of small-incision lenticule extraction for myopia by a novice surgeon at the first refractive surgery unit in Nepal during the first 2 years of operation. J Cataract Refract Surg. 2016;42(2):267-274.
3. Chansue E, Tanehsakdi M, Swasdibutra S, McAlinden C. Efficacy, predictability and safety of small incision lenticule extraction (SMILE). Eye Vis (Lond). 2015;2:14.
4. Hansen RS, Lyhne N, Grauslund J, Vestergaard AH. Small-incision lenticule extraction (SMILE): outcomes of 722 eyes treated for myopia and myopic astigmatism. Graefes Arch Clin Exp Ophthalmol. 2016;254:399-405.
5. Kim JR, Kim BK, Mun SJ, et al. One-year outcomes of small-incision lenticule extraction (SMILE): mild to moderate myopia vs. high myopia. BMC Ophthalmol. 2015;15:59.
6. Albou-Ganem C, Lavaud A, Amar R. SMILE: refractive lenticule extraction for myopic correction [in French]. J Fr Ophtalmol. 2015;38:229-237.
7. Kunert KS, Melle J, Sekundo W, et al. One-year results of small incision lenticule extraction (SMILE) in myopia [in Geerman]. Klin Monbl Augenheilkd. 2015;232:67-71.
8. Reinstein DZ, Carp GI, Archer TJ, Gobbe M. Outcomes of small incision lenticule extraction (SMILE) in low myopia. J Refract Surg. 2014;30:812-818.
9. Ang M, Mehta JS, Chan C, et al. Refractive lenticule extraction: transition and comparison of 3 surgical techniques. J Cataract Refract Surg. 2014;40:1415-1424.
10. Sekundo W, Reinstein DZ, Blum M. Improved lenticule shape for hyperopic femtosecond lenticule extraction (ReLEx(®) FLEx): a pilot study. Lasers Med Sci. 2016;31:659-664.
11. Blum M, Kunert KS, Vossmerbaumer U, Sekundo W. Femtosecond lenticule extraction (ReLEx) for correction of hyperopia – first results. Graefes Arch Clin Exp Ophthalmol. 2013;251:349-355.
12. Reinstein DZ, Pradhan KR, Dhungana P, et al. SMILE for hyperopia: visual and refractive outcomes, optical zone centration, diameter, and aberration induction. Poster presented at: ARVO 2016; May 4, 2016; Seattle, WA.
13. Reinstein DZ, Archer TJ, Gobbe M. Change in epithelial thickness profile 24 hours and longitudinally for 1 year after myopic LASIK: three-dimensional display with Artemis very high-frequency digital ultrasound. J Refract Surg. 2012;28:195-201.
14. Reinstein DZ, Archer TJ, Gobbe M. Accuracy and reproducibility of cap thickness in small incision lenticule extraction. J Refract Surg. 2013;29:810-815.
15. Donate D, Thaeron R. Preliminary evidence of successful enhancement after a primary SMILE procedure with the sub-cap-lenticule-extraction technique. J Refract Surg. 2015;31:708-710.
16. Graue-Hernandez EO, Pagano GL, Garcia-De la Rosa G, et al. Combined small-incision lenticule extraction and intrastromal corneal collagen crosslinking to treat mild keratoconus: long-term follow-up. J Cataract Refract Surg. 2015;41:2524-2532.
17. Mastropasqua L, Calienno R, Lanzini M, Nubile M. Small incision lenticule extraction after deep anterior lamellar keratoplasty. J Refract Surg. 2015;31:634-637.
18. Pradhan KR, Reinstein DZ, Carp GI, et al. Femtosecond laser-assisted keyhole endokeratophakia: correction of hyperopia by implantation of an allogeneic lenticule obtained by SMILE from a myopic donor. J Refract Surg. 2013;29:777-782.
19. Ganesh S, Brar S, Rao PA. Cryopreservation of extracted corneal lenticules after small incision lenticule extraction for potential use in human subjects. Cornea. 2014;33:1355-1362.

By Stephen G. Slade, MD
The use of small-incision lenticule extraction (SMILE) continues to grow around the world. Outside the United States, where SMILE is approved in virtually all markets, close to 500,000 procedures have been performed,. Interestingly, the procedural volume for SMILE has even proven to be more stable than that for LASIK in countries where refractive surgery volumes are down because of adverse press.
AT A GLANCE
• Small-incision lenticule extraction (SMILE) was introduced 7 years ago, and almost 500,000 procedures have been performed. SMILE is available in most markets worldwide, and the premarket approval application for use of the VisuMax laser for the procedure has been submitted to the FDA.
• Surgeons are studying SMILE for hyperopia as well as other applications of the procedure.
• Whether or not SMILE will replace LASIK remains to be seen. Dr. Reinstein views the procedures as complementary.
In the United States, Carl Zeiss Meditec has submitted to the FDA the final module of the company’s premarket approval application for the VisuMax femtosecond laser lenticule removal procedure for the correction of myopia.
US CLINICAL TRIAL
The clinical trial was conducted across five US study sites, with 336 eyes treated (unilaterally) and monitored for 12 months. The objective of the study was to evaluate the safety and effectiveness of the procedure for the reduction or elimination of -1.00 to -10.00 D of myopia with up to 0.50 D of refractive cylinder; cylinder was not treated as a part of this clinical trial.
By 6 months, 99.7% of eyes had achieved a UCVA of at least 20/40 by 6 months, with 88% of eyes achieving a UCVA of 20/20 or better at 6 and 12 months. In terms of the predictability of the achieved versus the intended manifest refraction spherical equivalent, it was within ±1.00 D of the attempted correction in more than 98% of eyes at all study visits. The proportion of eyes within ±0.50 D of the attempted correction was 93% at 6 months and 94% at 12 months. I am particularly impressed with the consistency of the scatterplots of predictability (Figure). There is no divergence in the upper ranges of myopia like one would see with LASIK or PRK. The numbers track more like those for an IOL, because SMILE is not “dose dependent”: the same amount of surgery and healing is involved for a -3.00 D treatment as for a -10.00 D correction.
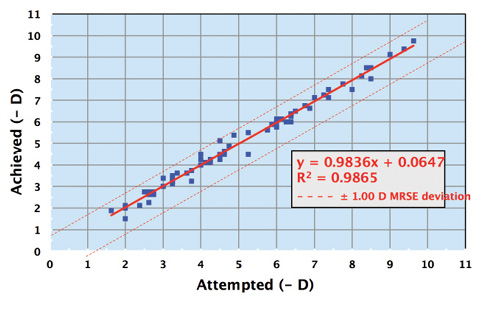
Figure. Manifest refraction spherical equivalent predictability at 3 months (attempted vs achieved, N = 69 eyes).
Safety was also well demonstrated in this trial. No study eye had a BSCVA of less than 20/40 beyond week 1 or experienced more than a 2.00 D increase in astigmatism at any visit, and there were no serious adverse events over the course of the study. At 12 months, 98% of eyes demonstrated no loss of BSCVA, and 26% actually showed gains in BSCVA.
The company has gained approval for and is concurrently studying the SMILE procedure for the treatment of myopia with astigmatism.
THE INVARIABLE COMPARISON
The invariable comparison is between SMILE and LASIK. In the largest published look (a review of 56 publications), Moshirfar and colleagues found the following: “Small-incision lenticule extraction has shown efficacy, predictability, and safety that are proportionate to those of laser in situ keratomileusis (LASIK), with the additional benefit that it eliminates flap creation and the attendant risks. The potential advantages of the procedure related to improved biomechanical stability, postoperative inflammation, and dry eye symptoms have not been fully established. Small-incision lenticule extraction-treated eyes have shown a reduced degree of postoperative corneal denervation and higher-order aberrations and an accelerated rate of corneal nerve convalescence relative to LASIK.”1
Will SMILE replace LASIK? I personally hope refractive surgeons have as many tools available as possible. Many attempts to rebrand LASIK and PRK and to sidestep their baggage have failed, including LASEK, cLASIK (Chiron LASIK), iLASIK (Abbott Medical Optics), and advanced surface ablation. These rebranded procedures are not fundamentally different from LASIK, however, whereas SMILE is. Even if SMILE is only “as good as” LASIK, will the former succeed with patients who have fear or confusion about PRK and LASIK? SMILE could be a welcome fresh start.
1. Moshirfar M, McCaughey MV, Reinstein DZ, et al. Small-incision lenticule extraction. J Cataract Refract Surg. 2015;41(3):652-665.
Dan Z. Reinstein, MD, MA(Cantab), FRCSC, DABO, FRCOphth, FEBO
• medical director, London Vision Clinic, London
• adjunct professor of ophthalmology, Department of Ophthalmology, Columbia University Medical Center, New York
• professeur associé, Centre Hospitalier National d’Ophtalmologie, Paris
• visiting professor, Biomedical Science Research Institute, Ulster University, United Kingdom
• drz@londonvisionclinic.com
• financial disclosure: consultant to Carl Zeiss Meditec; financial interest in ArcScan
Stephen G. Slade, MD
• practices at Slade and Baker Vision in Houston
• (713) 626-5544; sgs@visiontexas.com
• financial disclosure: medical monitor for Carl Zeiss Meditec’s SMILE studies