Michael Collins, MD

Few ophthalmic topics have been discussed and debated as enthusiastically recently as the role of the femtosecond laser in cataract surgery. When the idea of purchasing a laser was first broached at my surgery center’s board meeting 2 years ago, my response was a firm no—an answer that undoubtedly caught my colleagues off-guard.
I have a reputation as an early adopter of new technology, but it is difficult to dispute the effectiveness of traditional cataract surgery. Additionally, without any solid studies proving the technology’s efficacy, it was hard to know if the laser was worth the cost. Then, I thought back to the original use of the femtosecond laser in LASIK surgery. Although the early devices did not accomplish something I was unable to do myself with a blade, they did add precision and accuracy. More significantly, at least to me, femtosecond lasers became the standard of care in refractive surgery. How many fellowship-trained refractive surgeons still create LASIK flaps with a blade? These ruminations began to counter my initial reaction and ultimately led to the purchase of my practice’s laser platform for cataract surgery.
At a Glance
• Dr. Collins attributes the quieter eyes on postoperative day 1 to his spending less time in the eye and using less phaco energy after the laser procedure.
• Whether decreased phaco power benefits the average cataract surgery patient has not been adequately addressed, asserts Dr. Loden.
• According to Dr. Safran, a slightly longer phaco time and greater amount of ultrasound energy are not worth the risks and problems of laser cataract surgery.
ANECDOTAL EVIDENCE
Two years later, there is still no definitive research substantiating the claim that laser cataract surgery is truly better. That said, my administrator recently let me know that I have performed more than 1,500 cases, and I would argue that our hands-on, real-life experience carries some weight.
I recently asked the OR staff at my surgery center for their honest opinion of laser cataract surgery. I queried the technicians I bring with me from my practice, the technicians and nurses who only work at the surgery center, and the certified registered nurse anesthetists who rotate through all the surgery centers in the area. They all initially hated the laser, because it slowed things down and gave them more work to do. Every single one of them responded that laser cataract surgery was better than the standard approach and that they would opt for the laser if they themselves needed cataract surgery.
The optometrists who conduct the 1-day postoperative evaluations of patients on whom I operate tell me that they see about half as much corneal edema and anterior chamber cell and flare in the laser cases. I attribute this difference to my decreased time in the eye and to less phaco time and energy. When I crunched the numbers, I found that I am spending about half as much time inside the eye overall and that I am using a fraction of the phaco time and energy during a laser versus a standard case (Figures 1 and 2). I believe that this increased efficiency not only produces happier patients on postoperative day 1 but that it also increases safety. As one of my ophthalmology professors told me during my residency, “Be efficient inside the eye, but don’t worry about being fast. Do everything correctly in the least amount of time while inside the eye. The less time you are in the eye, the less chance there is that something will go wrong.”
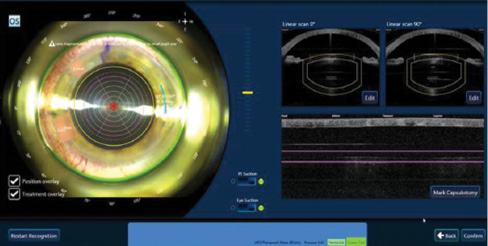
Figure 1. The fragmentation pattern of three radial cuts and five ring cuts using a femtosecond laser significantly decreases phaco time and energy.
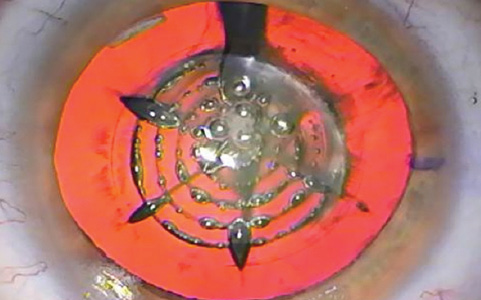
Figure 2. The laser cuts before phacoemulsification.
WHAT I AM AND AM NOT SAYING
I am not saying that laser cataract surgery is an overall time saver for an individual surgeon. I essentially have to do two procedures in two different rooms. The laser portion only takes a couple of minutes with the recently upgraded software. If I am completing 40 cases a day and 20 to 30 of those use the laser, however, those 2 to 3 minutes per case add up. The questions I continue to ask myself are, however, if the laser is working properly (any such device may infrequently have issues),
• Would I want it used on my own eyes?
• Would I use it on my family members?
• Is it worth the time, expense, and effort?
My answer to all of these questions is a firm yes.
Ophthalmologists want to make cataract surgery better and safer for patients. That is what I am trying to do with the laser. For this technology to become mainstream, it will require solid studies with long-term results showing increased safety and better outcomes. After performing laser cataract surgery for a couple of years, however, I do feel that it is better, and improvements continue.
James C. Loden, MD

Laser cataract surgery is here to stay, but the debate over its merits and benefits will likely continue for years. Since the first laser was introduced, the technology has advanced significantly in terms of fragmentation patterns and the creation of a smooth rent-free capsulotomy, clear corneal incisions, and corneal relaxing incisions. I am reminded of the LASIK industry in the late 1990s and early 2000s, when enhancements were rolled out yearly. One argument for laser cataract surgery is the potential decrease in phaco energy needed to remove the cataract and the theoretical benefits.
REALITY VERSUS THEORY
Many peer-reviewed studies, articles, and presentations describe decreased phaco time with laser cataract surgery. It is worth acknowledging the difficulty of eliminating surgeon bias in a study designed to compare phaco time in conventional versus laser cataract surgery. With a horizontal chopping technique, a large-bore phaco needle, and vacuum of 475 mm Hg, it would be possible to remove up to 50% of nuclei during traditional cataract surgery with nearly zero phaco time. This approach, however, might not be in the patient’s best interest. It would be even easier to use vacuum, flow, and the chopper to remove a prefragmented lens. The investigating surgeon would then easily show less phaco time in a study simply by slowing down the procedure and cramming lens material into the phaco tip with the chopper.
Stephen Lane, MD, and I moderated a session on laser cataract surgery at the 2015 annual symposium of the American Society of Cataract and Refractive Surgery, and several papers showed less phaco power. Dr. Lane and I pointed out from the podium that the real endgame with laser cataract surgery is not necessarily using little to no phaco power but performing phacoemulsification to remove the cataract as safely and rapidly as possible. The goal is a clear cornea on postoperative day 1.
In my opinion, what has not been adequately addressed but is of the upmost importance is whether decreased phaco power benefits the average cataract surgery patient. So, phaco power was 15% after the laser procedure versus a theoretical 27% with standard cataract surgery. Is this of any clinical value to the patient? With the endothelial protection offered by modern ophthalmic viscosurgical devices and the speed of the case, I think not. In eyes with dense cataracts where the phaco power is 67 after the laser procedure versus 113 with standard cataract surgery, however, I think the answer is a resounding yes.
OTHER AREAS OF CONTENTION
Research comparing phacoemulsification in standard versus laser cataract surgery has shown little to no advantage with the latter.1 Other areas of contention include the safety and the refractive benefits of a laser capsulotomy compared with a manual capsulorhexis, the accuracy of laser versus manual relaxing incisions, and the benefits of three-plane laser clear corneal incisions versus single-plane manual incisions. Surgeons must objectively assess the data supporting both sides of the arguments and prioritize what they believe is right for their patients over what is right for their practices.
1. Barry P. FLACS ESCRS Study. Paper presented at: XXXIII Congress of the ESCRS; September 7, 2015; Barcelona, Spain.
Steven G. Safran, MD

Ophthalmologists have been using ultrasound to remove cataracts for decades. Cataract surgery using phacoemulsification is arguably the safest, most successful, widely performed operation in all of medicine. A femtosecond laser may reduce the ultrasound energy some ophthalmologists need to perform cataract surgery, but is laser cataract surgery safer, faster, better, and more efficient? If not, why add the complexity and cost of such a device?
THE CAPSULOTOMY
Laser cataract surgery was introduced with the promise that a perfectly round capsulotomy in every case would provide refractive outcomes rivaling those achieved with LASIK. Evidence now suggests, however, that the size and shape of the capsulotomy have little influence on lens position, tilt, or astigmatism.1 At best, the procedure “treads water” with regard to improving refractive outcomes.
SAFETY
Research has yet to show that laser cataract surgery is as safe as well-performed standard cataract surgery. Scanning electron microscopy shows that the edge of the laser capsulotomy is not smooth and continuous like that of a manual tear but rather jagged and shaped like a zipper with a micro-can opener type of configuration, which may lead to decreased structural integrity. The result may be a significantly higher rate of anterior capsular radial tears.2
In a study of 4,000 patients that compared laser and standard cataract surgery, the refractive outcomes were similar, but the rate of complications was higher across the board in the laser group: 8.4 times higher in terms of anterior capsular tears, 2.4 times higher for posterior capsular tears, a 12-fold greater risk of corneal haze, and a fivefold greater need for iris hooks or the Malyugin Ring (MicroSurgical Technology) due to miosis in the laser versus manual group.3 The FLACS ESCRS Study also found a higher incidence of complications with laser versus standard cataract surgery. Investigators for that study concluded, “Femto patients have worse post-operative visual acuity. Femto patients have more post-operative complications and more patients with a post-op visual acuity worse than pre-op.”4
Yes, some studies have demonstrated a reduction in the ultrasound energy required when a laser is used to fragment the nucleus,5 but of course, laser energy is then added to the equation. Research now shows that laser lens fragmentation significantly increases the temperature of the anterior chamber,6 causes a significant acidic pH shift in the aqueous due to the formation of carbonic acid during cavitation,7 and releases prostaglandins8 and other inflammatory mediators,9 leading to greater apoptosis and an increase in inflammatory markers.10 The eye is exposed to this mess until it is vacuumed out during phacoemulsification. I view the phaco handpiece as a solution to the problems created by the laser. More importantly, I believe that a slightly longer phaco time or marginally greater ultrasound energy is a small price to pay to avoid these issues altogether. The side effects of laser cataract surgery that I have described may explain some of the complications reported in the ESCRS FLACS Study4 and research by Abell and colleagues.2,3
Standard cataract surgery takes significantly less time than laser cataract surgery,11 and it carries a lower risk of complications.3,4 The former remains the gold standard.
1. Findl O. Influence of rhexis size and shape on postoperative IOL tilt, decentration and anterior chamber depth. Paper presented at: The XXXI Congress of the ESCRS; October 7, 2013; Amsterdam, Netherlands.
2. Abell RG, Davies PE, Phelan D, et al. Anterior capsulotomy integrity after femtosecond laser-assisted cataract surgery. Ophthalmology. 2014;121(1):17-24.
3. Abell RG, Darian-Smith E, Kan JB, et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery: outcomes and safety in more than 4000 cases at a single center. J Cataract Refract Surg. 2015;41(1):47-52.
4. Barry P. FLACS ESCRS Study. Paper presented at: XXXIII Congress of the ESCRS; September 7, 2015; Barcelona, Spain.
5. Conrad-Hengerer I, Hengerer FH, Schultz T, Dick HB. Effect of femtosecond laser fragmentation on effective phacoemulsification time in cataract surgery. J Refract Surg. 2012;28(12):879-883.
6. Mencucci R, Matteoli S, Corvi A, et al. Investigating the ocular temperature rise during femtosecond laser lens fragmentation: an in vitro study. Graefes Arch Clin Exp Ophthalmol. 2015;253(12):2203-2210.
7. Rossi M, Di Censo M, Oum M. Changes in aqueous humor pH after femtosecond laser-assisted cataract surgery. J Refract Surg. 2015;31(7):462-465.
8. Schultz T, Joachim SC, Kuehn M, Dick HB. Changes in prostaglandin levels in patients undergoing femtosecond laser-assisted cataract surgery. J Refract Surg. 2013;29(11):742-747.
9. Chen H, Lin H, Zheng D, et al. Expression of cytokines, chmokines and growth factors in patients undergoing cataract surgery with femtosecond laser pretreatment. PLoS One. 2015;10(9):e0137227.
10. Toto L, Calienno R, Curcio C, et al. Induced inflammation and apoptosis in femtosecond laser-assisted capsulotomies and manual capsulorhexes: an immunohistochemical study. J Refract Surg. 2015;31(5):290-294.
11. Lubahn JG, Donaldson KE, Culbertwon WW, Yoo SH. Operating times of experienced cataract surgeons beginning femtosecond laser-assisted cataract surgery. J Cataract Refract Surg. 2014;40(11):1773-1776.
Michael Collins, MD
• medical director and founder, Collins Vision, with offices in Fort Myers and Naples, Florida
• (239) 936-4706; mjc@collinsvision.com
James C. Loden, MD
• president, Loden Vision Centers, Nashville, Tennessee
• (615) 859-3937; lodenmd@lodenvision.com
Steven G. Safran, MD
• private practice in Lawrenceville, New Jersey
• (609) 896-3931; safran12@comcast.net
• financial interest: none acknowledged


