Stellaris Vision Enhancement System
By Y. Ralph Chu, MD
Two models of Bausch + Lomb’s phaco machine are available: the Stellaris Vision Enhancement System and the Stellaris PC Vision Enhancement System, which includes retinal surgery capabilities. My experience is with the former.
FLUIDICS
What most attracted me to this machine was the fluidics—the incredibly stable chambers that the unit provides. In my experience, the system’s StableChamber Fluidics controls and pressurizes the anterior chamber to maintain excellent stability, even under high levels of vacuum, which enhances safety. For example, a stable anterior chamber decreases fluctuation of the capsular bag and movement of the iris in eyes with a small pupil, and it thus lowers the risk of my inadvertently bringing the iris into the phaco tip.
The Stellaris is a vacuum-based system, which I find particularly helpful in combination with laser cataract surgery, which can leave fine cortical strands clinging to the capsule. Unlike with a peristaltic machine, “holdability” through occlusion of the phaco tip happens quickly with a vacuum-based system, which makes cortical cleanup efficient.
In some cases, after the laser presoftens the nucleus, no phaco energy is needed to remove the fragments. I have customized the Bluetooth dual-linear foot pedal with my preferred postlaser cataract removal setting (Figures 1 and 2). It allows me to control the amount of vacuum in the up-and-down position and the amount of ultrasound energy using the side-to-side yaw. If the nucleus is slightly dense, I can just slide my foot a little bit to the side to initiate ultrasound in a linear fashion. I really like how customizable the Stellaris is.

Figure 1. The screen display of the Stellaris Vision Enhancement System.

Figure 2. The Bluetooth dual-linear foot pedal.
ENERGY DELIVERY
Improved energy delivery is a feature of advanced phaco platforms. On the Stellaris, Attune Advanced Software includes Programmable Waveform Modulation, which gradually ramps up the energy delivered. In basic terms, the software prevents the repulsion of small pieces of the nucleus from the tip so that I can effectively grasp the fragments. This efficiency decreases the amount of phaco energy used, which I believe leaves a quieter eye that recovers more quickly postoperatively.
USER INTERFACE
The interface is very user friendly. My technicians and I were able to customize vacuum levels and preprogram the foot pedal for different modes. Since then, the day-to-day interface and use of the foot pedal have been simple and quick.
HANDPIECE
The six-crystal Attune Handpiece works at a frequency of 28.5 kHz. I have been impressed by the efficiency of power delivery. I find that the handpiece creates fewer cavitation bubbles than my previous model, so the anterior chamber remains clear. Different tips are available. I typically use a 2.4-mm incision, but when implanting the Crystalens (Bausch + Lomb), I increase the size to about 2.75 mm. I appreciate the versatility that the Stellaris provides by allowing me to change to a smaller phaco sleeve or needle when I wish.
PEARLS
The key to getting the most out of the Stellaris has been taking the time to customize it to suit how I like to perform surgery. Some ophthalmologists favor “stop and chop” surgery with in-the-bag phacoemulsification. Specific settings make this unit work for that kind of technique. I myself prefer to rotate the nucleus and tilt it out of the capsular bag. This supracapsular technique requires fairly high vacuum for efficient nuclear removal. Sometimes, however, I cannot get a nucleus out of the bag. I then need a low-flow mode that works in the bag. I have been impressed by how effectively the Stellaris can move between techniques. Again, I customized the foot pedal so that I can use it to control ultrasound and vacuum.
PITFALLS
Transitioning to the Stellaris will be very natural for surgeons used to vacuum-based systems. To cataract surgeons used to a peristaltic system, I recommend starting with low vacuum settings. Phacoemulsification occurs more quickly with a vacuum-based versus a peristaltic system. I also recommend taking advantage of the support offered by Bausch + Lomb when becoming familiar with the machine.

WhiteStar Signature Pro
By Francis S. Mah, MD
I recently used the new WhiteStar Signature Pro phaco system (Abbott Medical Optics). For me, the fluidics and chamber stability are what make this machine truly impressive.
FLUIDICS
Occlusion-sensing technology anticipates and proactively adjusts to IOP changes to help maintain a stable chamber, even at high vacuum and flow settings (Figure). Surgeons will find that the new system’s fluidics are much more responsive due to a fivefold increase in the vacuum sampling rate, from every 20 milliseconds down to every 4 milliseconds. This technology will potentially reduce complications and surgical time.
One of my first cases nicely illustrates the impact of occlusion-sensing technology on chamber maintenance. The patient was taking tamsulosin (Flomax; Boehringer Ingelheim Pharmaceuticals), and the eye had a dense cataract and a 5-mm pupil. Using the WhiteStar Signature Pro, I performed standard phacoemulsification, with no femtosecond laser. In cases like this one, I have often encountered a lot of chamber “bounce” with a floppy iris and have needed to use a Malyugin Ring (MicroSurgical Technology). In this case, however, the chamber was rock solid throughout surgery, which proceeded smoothly without pupil-stretching devices.
Like its predecessor, the WhiteStar Signature Pro has both peristaltic and venturi vacuum pumps, and it allows surgeons to switch back and forth between the two. This means I can take advantage of the strengths of each pump style instead of having to adapt my technique to compensate for the disadvantages. The intraoperative control of a peristaltic vacuum for sculpting and nuclear disassembly, for example, is safe and impressive, but then I can take advantage of the power, speed, and followability of venturi vacuum for cortical and viscoelastic removal.
TRANSVERSE ULTRASOUND
I find that the Ellips FX handpiece, which moves in a continuous elliptical pattern, reduces the amount of phaco time and energy required to penetrate dense nuclei. The comfortable handpiece easily cut through the dense nucleus in the case described earlier, which is beneficial in terms of surgical outcomes and the speed of visual recovery.
Generally speaking, it is difficult to differentiate visual acuity by machine after a month, but potentially superior results on postoperative day 1 or week 1 will give patients an additional “wow” factor. Recent studies have shown that the combination of longitudinal/transversal ultrasound significantly reduces phaco time, balanced salt solution volume, corneal edema, and endothelial cell loss after surgery compared to torsional ultrasound.1
OTHER FEATURES
The interface is easy to use. My technicians appreciated being able to prime and tune the device, handpiece, and tubing with the push of a single button. I find the system to be cost-effective, with nice ergonomics and a small footprint compared to those of other phaco systems. I also like the new wireless foot pedal, which is significantly more responsive than on earlier models of the machine.
The WhiteStar Signature Pro connects wirelessly to a new mobile analytics tool, the Cataract Analysis and Settings Application. The latter allows me to review performance and procedural metrics from the WhiteStar Signature Pro in graph form on a tablet. This has the potential to help me better use my own data to improve outcomes. For example, by tracking how long sculpting takes me, I may be able to fine-tune my technique or adjust the device settings to be more efficient. In a group setting, it will be possible to identify which surgeons are achieving the best outcomes and to learn from their techniques and settings.
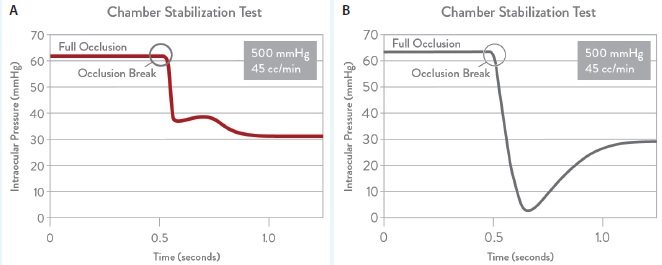
Figure. Chamber stabilization environment technology (with [A] vs without [B]) helps surgeons to anticipate occlusion and prevent surges.
CONCLUSION
Modern phaco machines are highly advanced devices that perform well for routine cases. Subtle differences among platforms, however, can make surgery easier, safer, and more efficient—especially in complex cases—and potentially reduce the need for additional surgical tools. In my opinion, the WhiteStar Signature Pro will make an average surgeon good and a good surgeon even better.
1. Assil KK, Harris L, Cecka J. Transverse vs torsional ultrasound: prospective randomized contralaterally controlled study comparing two phacoemulsification-system handpieces. Clin Ophthalmol. 2015;9:1405-1411.

The Compact Intuitiv System
By Farrell “Toby” Tyson II, MD
The rising popularity of laser cataract surgery has led to the engineering of new designs of phaco machines and innovative features intended to accommodate various clinical needs. Surgeons want to serve their patients with the most advanced technology and safety features, but innovation comes at a cost. The Compact Intuitiv System (Abbott Medical Optics) was built to complement laser cataract procedures and deliver a next-generation phaco unit that keeps costs in check (Figure 1).
Without sacrificing sophistication, this portable, smaller-profile device includes all of the function needed to reliably and safely perform phacoemulsification. OR efficiencies aimed at reducing procedural costs will prove particularly important, as baby boomers reach cataract age. The cost of surgery is often prohibitive. Frequently, the patients with the worst cases do not have the insurance and/or financial resources to access laser technology. A full-featured phaco machine capable of dealing with dense cataracts is therefore simply a necessity in an environment of rising costs and declining reimbursement.

Figure 1. The Compact Intuitiv System.

Figure 2. The Ellips FX handpiece.
FLUIDICS
The Compact Intuitiv System introduces automatic occlusion sensing—real-time chamber stabilization technology that uses computer algorithms combined with small-bore, flexible tubing and a flow-based pump to maintain IOP and reduce postocclusion surge (Abbott Medical Optics, unpublished data, 2014). The system proactively adjusts vacuum settings in milliseconds upon sensing an occlusion, and the flow-based peristaltic pump decreases surge while improving fluidics control. This intraoperative intraocular control allows the surgeon to adjust vacuum, fluid flow, and rise time. Better chamber maintenance permits the use of higher fluidics and breaks up the cataract more efficiently while using less energy. In my experience, this platform distributes phaco energy very well. Using less energy and having the pumps sense what is happening in the chamber allows me to be more aggressive and faster when removing the nuclear particles created during laser cataract surgery.
CREATING EFFICIENCIES
The right tools streamline procedures and improve control. The system’s user-friendly accessories and enhancements include a specially designed handpiece, an easy foot pedal control, a wireless remote control, and a portable chassis. Practices can streamline OR setup and reduce costs by reusing tubing or using auto-loading tube packs with one-step prime/tube.
I find that the Ellips FX handpiece consistently and quickly cuts a precise elliptical pattern on both hard and soft lenses (Figure 2). The tip’s elliptical movement combines the benefits of transversal and longitudinal movement for followability and minimized clogging. In my experience, this feature creates valuable efficiencies by decreasing phaco time, balanced salt solution volume, phaco power, and heat generated at the incision point.1,2
When factored together, the result is quicker case times and reduced corneal edema. My patients have clear corneas on day 1, which gives them the confidence to move forward with surgery on the second eye. They experience the “wow” factor—an expected outcome brought about because of the premium IOL market. When my patients have a clear cornea on day 1, I exceed their expectations.
CONCLUSION
The Compact Intuitiv System is a full-featured phaco machine that delivers the latest generation of technology without compromising quality. I can rely on this machine to meet all of my phaco needs while simultaneously creating efficiencies in the OR and generating excellent outcomes.
1. Assil KK, Harris L, Cecka J. Transverse vs torsional ultrasound: prospective randomized contralaterally controlled study comparing two phacoemulsification-system handpieces. Clin Ophthalmol. 2015;9:1405-1411.
2. Floyd M, Valentine J, Coombs J, Olson RJ. Effect of incisional friction and ophthalmic viscosurgical devices on the heat generation of ultrasound during cataract surgery. J Cataract Refract Surg. 2006;32(7):1222-1226.

The Centurion Vision System
By Lawrence Woodard, MD
As a clinical investigator for the Centurion Vision System (Alcon), I have been using this machine since the summer of 2013. At that time, I had been using Alcon’s Infiniti Vision System for 10 years and was very pleased with its capabilities. I was not sure the new machine would improve my ability to remove cataracts safely and efficiently. Now, I can unequivocally state that I am performing cataract surgery in a much more controlled anterior chamber environment than ever before.1 This article describes my experience with adjusting fluidic parameters to minimize ultrasound time, cumulative dissipated energy (CDE), and fluid usage.2
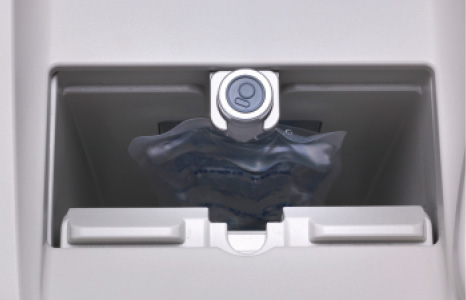
Figure 1. Active Fluidics technology uses plates that compress the BSS bag to dynamically control fluid delivery into the eye, improving anterior chamber stability.
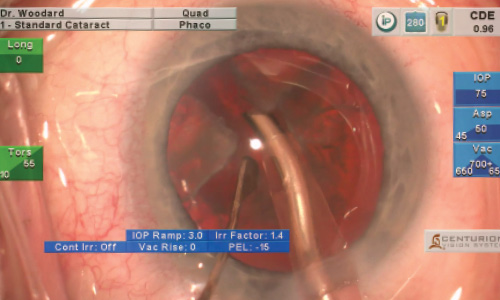
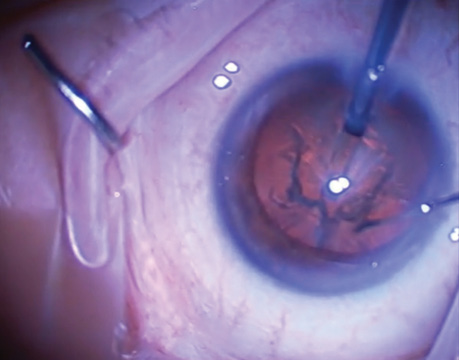
Figure 2. The author uses a 45º Intrepid Balanced Tip to remove nuclear fragments with high vacuum settings after dividing the grade 2 nucleus. Minimal ultrasound energy is used.
FLUIDICS
Traditionally, phaco machines have used gravity to passively deliver balanced salt solution (BSS; Alcon) into the anterior chamber based upon the fixed height of the BSS bottle. The limitation of this design is that the pressure delivered to the eye changes based on the aspiration flow rate, which is influenced by variables such as tip occlusion, fluid egress at the incisions, compliance of the tubing, and vacuum settings. As a result, the volume of fluid in the anterior chamber fluctuates significantly throughout the procedure (especially at high vacuum levels), which increases movement of the posterior capsule. The Centurion’s Active Fluidics technology addresses these issues with two compression plates. They rapidly compress or decompress the BSS bag, in a closed chamber, based on the dynamic fluidic changes occurring during surgery (Figure 1). The Fluidics Management System has a vacuum sensor placed along the aspiration line and a pressure sensor along the irrigation line that continuously monitor pressure loss during the procedure.2 The system then compensates for lost pressure by quickly increasing or decreasing compression of the BSS bag to actively adjust the amount of fluid delivered to the eye. Keeping the volume of fluid in the anterior chamber more consistent better maintains the preset target IOP, thereby minimizing fluctuations in anterior chamber depth and movement of the posterior capsule. Allowing the surgeon to decrease the vacuum and aspiration flow rate limits in foot position 3 also better controls postocclusion surge and minimizes anterior chamber shallowing once occlusion breaks.
The Centurion also incorporates two new surgeon-adjustable parameters that help to control the intraocular environment. The “irrigation factor” setting maintains a more stable anterior chamber by allowing the surgeon to adjust for fluid egress at the incision based on his or her choice of phaco tip, sleeve, and incision morphology. The “IOP ramp” setting allows the surgeon to adjust how rapidly fluid is delivered in the eye upon entry of the tip. This helps to prevent sudden deepening of the anterior chamber upon entry, which may cause reverse pupillary block and significant discomfort for the patient.
The Intrepid Balanced Tip incorporates a computer-generated double bend, which increases excursion at the distal end while minimizing movement proximally at the incision. Lower CDE is attained, because nuclear fragments are maintained at the tip better due to less repulsion.
MY EXPERIENCE
During my first few cases, the Centurion produced a more stable anterior chamber than any machine I had previously used. I favor high vacuum levels when removing nuclear fragments; my goal is to maximize aspiration while minimizing ultrasound energy and fluid usage. My normal settings on the Infiniti for quadrant removal were vacuum of 550 mm Hg, an aspiration flow rate of 45 mL/min, and a bottle height of 110 cm. If I increased the vacuum further, the anterior chamber became too volatile and unstable. With the Centurion, I was able to gradually increase my vacuum limit, because the anterior chamber was so stable. I now have the vacuum limit set at 700 mm Hg, and the anterior chamber is more stable than it was with a vacuum level of 550 mm Hg on the Infiniti (Figure 2). In order to safely maintain these settings, it is imperative to size corneal incisions to minimize fluid egress.
The benefit of increased vacuum is that my CDE has decreased significantly compared with previous machines, yet I use less fluid during the case. Clinically, corneas are clearer on postoperative day 1 due to less endothelial cell trauma during surgery. My settings will not suit everyone, but other surgeons will likely be able to use a higher vacuum level with the Centurion than they have with other machines. A recent study found that CDE, fluid usage, and ultrasound time were all significantly lower when higher vacuum levels were used with the Centurion compared with moderate vacuum levels.3
CONCLUSION
I believe that the Centurion’s Active Fluidics technology and Intrepid Balanced Tip are monumental steps forward in cataract surgery. These advances allow me to remove the cataract more efficiently by creating a more controlled intraocular environment while simultaneously minimizing ultrasound and fluid usage.
1. Solomon KD, Lorente R, Cionni RJ, Fanney D. Prospective, randomized clinical study using a new phaco system with intraocular system target pressure control. Paper presented at: ASCRS/ASOA Congress & Symposium; April 28, 2014; Boston, MA.
2. Centurion Vision System and AutoSert IOL Injector Handpiece Directions for Use. Alcon Laboratories, Inc.; Fort Worth, TX.
3. Allen D. Effectiveness of high vacuum versus lower vacuum with new phacoemulsification console with active fluidics. Paper presented at: ASCRS/ASOA Congress & Symposium; April 28, 2014; Boston, MA.
Y. Ralph Chu, MD
• founder and medical director, Chu Vision Institute, Bloomington, Minnesota
• (952) 835-0965; yrchu@chuvision.com
• financial disclosure: consultant to Bausch + Lomb/Valeant
Francis S. Mah, MD
• director of cornea and external diseases and codirector of refractive surgery at the Scripps Clinic Torrey Pines in La Jolla, California
• (858) 554-7996; mah.francis@scrippshealth.org
• financial disclosure: consultant to Abbott Medical Optics, Alcon, and Bausch + Lomb
Farrell “Toby” Tyson II, MD
• practices at Cape Coral Eye Center in Cape Coral, Florida
• (239) 542-2020; tysonfc@hotmail.com
• financial disclosure: consultant to and speaker and researcher for Abbott Medical Optics
Lawrence Woodard, MD
• medical director of Omni Eye Services and Atlanta Eye Surgery Center in Atlanta
• (404) 351-1990; lwoodard@omnieyeatlanta.com
• financial disclosure: consultant to, clinical investigator for, and speaker for Alcon