
Corneal collagen cross-linking (CXL) is designed primarily to decrease the progression of keratoconus and corneal ectasia. Underlying the efficacy of CXL is the production of covalent cross-links within and between molecules (collagen and glycosaminoglycans) in the corneal stroma, leading to overall strengthening of corneal biomechanics. Many laboratory and clinical studies have demonstrated beneficial visual and optical effects of CXL in treating ectatic corneal disorders, with few reported complications.1 My colleagues and I reported that patients experienced a 1.70 D flattening of maximum keratometry on corneal topography and an improvement of approximately 1 Snellen line in both distance BCVA and UCVA 1 year after CXL.2 In other studies, we found improvements in corneal topography keratoconus indices and in total and corneal higher-order aberrations as well as enhanced subjective visual function in treated patients.3-5
LASIK may lead to a decrease in structural stability of the cornea in some circumstances.6 By making a LASIK flap and removing tissue, the anterior layers of the corneal structure are modified, and hence, corneal rigidity may decrease. According to John Marshall, PhD, LASIK may weaken the cornea by 15% to 25%.7 In the vast majority of cases, this does not lead to adverse clinical effects. However, based on the success of CXL in the setting of ectatic disease management, investigators have become interested in the procedure’s use as an adjunct to LASIK and PRK. The goal of the combined procedure is to strengthen the cornea, both to avoid corneal ectasia and to stabilize long-term refractive outcomes.
LASIK Xtra
There are a number of potential indications for a combined CXL and LASIK procedure (LASIK Xtra; Avedro [not FDA approved]). LASIK Xtra can be viewed as an extra safety element for eyes with thin corneas or requiring high degrees of correction demanding a greater amount of tissue removal (Figure). Eyes with high myopia and hyperopia may have a greater tendency to regress over time after LASIK.8 Thus, strengthening the cornea with concurrent CXL may be beneficial for the long-term stability of the refractive result and ultimate predictability of the procedure. Another group of patients who may also benefit from LASIK Xtra are those in whom the topography, though not frankly abnormal, may be of some concern. There is also the possibility of using CXL in combination with a topography-guided laser treatment in the case of frank keratoconus.
To date, the standard Dresden protocol, as first described by Professor Theo Seiler and colleagues, is used to treat ectatic corneal diseases.1 The central 9 mm of the epithelium is removed. Riboflavin is then administered topically every 2 minutes for a total of 30 minutes to ensure complete saturation of the corneal stroma, which is then exposed to ultraviolet A radiation (365-nm light) for 30 minutes at an irradiance of 3 mW/cm2.
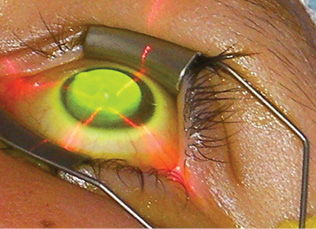
A more recently conceived technique, accelerated crosslinking, uses higher ultraviolet power with a proportionally decreased treatment time for an equivalent total dose. Accelerated CXL has become popular in LASIK Xtra, because it can be easily integrated into the LASIK procedure.
TOPOGRAPHY-GUIDED PRK and CXL
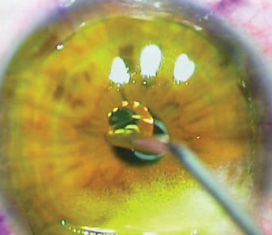
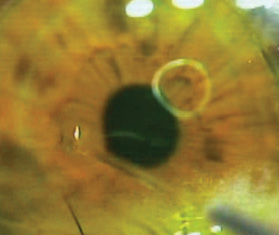
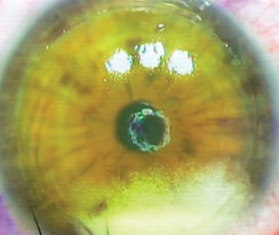
Researchers have focused considerable attention on CXL in conjunction with topography-guided PRK. The idea is to halt or decrease the progression of keratoconus via CXL and reduce the irregularity and asymmetry of the corneal optics with topography-guided PRK. Kanellopoulous and Binder reported improved distance BCVA and UCVA in 27 of 32 eyes after combined CXL and PRK.9 These investigators stated that same-day CXL combined with topography-guided PRK was superior to sequential procedures for visual rehabilitation.
CXL IN HIGH-RISK PATIENTS
CXL may be considered in eyes at high risk of corneal instability or ectasia after LASIK or PRK. These include eyes that have thin corneas, require high correction, or have worrisome but not frankly contraindicative topography. Young patients needing a high correction or who have a high degree of astigmatism and anisometropia may also be at higher risk.14 In such cases, LASIK Xtra may theoretically provide an extra element of safety.
LASIK XTRA increases safety by increasing corneal strength and improves long-term refractive stability after LASIK
The Basic Procedure for LASIK Xtra (Avedro; not FDA approved)
1. Perform the standard LASIK procedure.
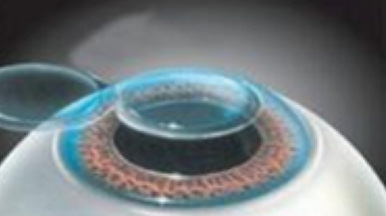

2. Place one drop of 0.25% riboflavin (0.87% saline, dextran) on the stromal bed.
3. Let soak for 60 to 90 seconds.
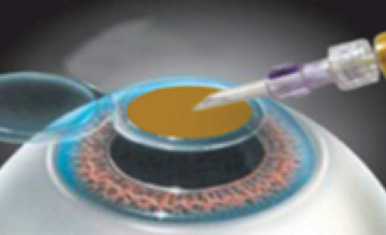
4. Copiously irrigate riboflavin off the stromal bed.
5. Replace the LASIK flap.
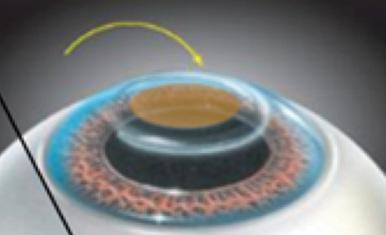
6. Complete ultraviolet exposure (30 mW for 2-3 minutes if using the accelerated CXL protocol).

CXL AND LASIK FOR HIGH REFRACTIVE CORRECTIONS
Patients requiring a high degree of correction, particularly high hyperopes, may experience regression years after LASIK.8 In these cases, combining LASIK and CXL may improve the long-term stability of the refractive result and the ultimate predictability of the procedure. International studies have shown the potential benefit for patients undergoing high myopic and hyperopic corrections. Tan compared 72 highly myopic eyes (> -8.00 D) treated with adjunctive CXL and 62 eyes that underwent LASIK alone. Predictability and visual acuity results were found to be better in the combined treatment group.10
At a Glance
• The combined CXL and LASIK procedure (LASIK Xtra) is designed to increase surgical safety and refractive stability in eyes that have thin corneas or require high degrees of correction.
• Strengthening the cornea with concurrent LASIK and CXL may be particularly beneficial for high hyperopes and myopes by increasing the longterm stability of the refractive result.
• Additional studies are needed to determine if the LASIK nomogram needs to be adjusted when the procedure is combined with CXL and to assess the risk of infection, inflammation, and corneal haze.
Kanellopoulos compared LASIK Xtra (65 eyes) to standard LASIK (75 eyes) for high myopic corrections (mean correction, approximately -6.00 D).11 In the combined treatment group, 91% of eyes achieved a distance UCVA of 20/20 or better, and 95% achieved a distance UCVA of 20/25 or better. In the LASIK only group, 85% of eyes achieved a distance UCVA of 20/20 or better, and 89% achieved a distance UCVA 20/25 or better.
Hyperopic patients may be of greater concern with regard to regression over time after LASIK.12 This may be secondary to epithelial remodeling and hyperplasia over the area of ablation. Alternatively, regression may be related to biomechanical changes induced by the midperipheral tissue removal of the hyperopic ablation. Theoretically, combined LASIK and CXL may therefore be of the most value for this refractive group.
Kanellopoulos studied the results of LASIK Xtra in 34 patients with hyperopia.13 Preoperatively, the mean refraction was approximately +3.15 D and +3.40 D in the LASIK Xtra and LASIK only groups, respectively. Eyes that underwent CXL demonstrated a mean regression from treatment of +0.22 D, whereas eyes that underwent LASIK showed greater regression of +0.72 D, suggesting a benefit of LASIK with adjunctive CXL for this population.
ROUTINE LASIK AND CXL
Corneal ectasia after laser refractive surgery is rare. Preoperative factors can usually be identified to guide proper patient selection and treatment. Even so, ectasia can occur in cases where there are no preoperative warning signs. If combining LASIK and CXL safely reduces risks, some surgeons argue, the combined procedure may be advisable. However, there are theoretical downsides of the combined procedure such as increased procedural time and possibly increased risks of infection, inflammation, or corneal haze. Such consequences appear to be minimized by irrigating the stromal bed with riboflavin solution before repositioning the flap and by limiting procedural time with an accelerated CXL technique. In addition, studies are still required to ascertain whether the LASIK nomogram needs to be adjusted when the procedure is performed in conjunction with CXL. Early international data suggest little difference in refractive outcomes between LASIK and combined LASIK and CXL,15 suggesting that a substantial adjustment to the surgeon’s standard LASIK nomogram may not be necessary.
CONCLUSION
Adjunctive CXL may increase the safety and accuracy of laser refractive surgery. The clinical settings in which to use the combined procedure have yet to be fully defined, but research is ongoing. n
1. Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-a-induced collagen crosslinking for the treatment of keratoconus. Am J Ophthalmol. 2003;135:620-627.
2. Hersh PS, Greenstein SA, Fry KL. Corneal collagen crosslinking for keratoconus and corneal ectasia: one-year results. J Cataract Refract Surg. 2011;37:149-160.
3. Greenstein SA, Fry KL, Hersh PS. Corneal topography indices after corneal collagen crosslinking for keratoconus and corneal ectasia: one year results. J Cataract Refract Surg. 2011:37:1282-1290.
4. Greenstein SA, Fry KL, Hersh, MJ, Hersh PS. Higher-order aberrations after corneal collagen crosslinking for keratoconus and corneal ectasia. J Cataract Refract Surg. 2012;38:292-302.
5. Brooks NO, Greenstein SA, Fry KL, Hersh PS. Patient subjective visual function after corneal collagen crosslinking for keratoconus and corneal ectasia. J Cataract Refract Surg. 2012;38: 615-619.
6. Sinha Roy A, Dupps WJ Jr, Roberts CJ. Comparison of biomechanical effects of small-incision lenticule extraction and laser in situ keratomileusis: finite-element analysis. J Cataract Refract Surg. 2014;40:971-980.
7. Knox Cartwright NE, Tyrer JR, Jaycock PD, Marshall J. Effects of variation in depth and side cut angulations in LASIK and thin-flap LASIK using a femtosecond laser: a biomechanical study. J Refract Surg. 2012;6:419-425.
8. Alió JL, Soria F, Abbouda A, Peña-García P. Laser in situ keratomileusis for -6.00 to -18.00 diopters of myopia and up to -5.00 diopters of astigmatism: 15-year follow-up. J Cataract Refract Surg. 2015:41:33-40.
9. Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: the athens protocol. J Refract Surg. 2011;27:323-331.
10. Randleman JB, Woodward M, Lynn MJ, Stulting RD. Risk assessment for ectasia after corneal refractive surgery. Ophthalmology. 2008;115(1):37-50.
11. Tan J, Lytle GE, Marshall J. Consecutive laser in situ keratomileusis and accelerated corneal crosslinking in highly myopic patients: preliminary results [published online ahead of print December 5, 2014]. Eur J Ophthalmol. doi:10.5301/ejo.5000543.
12. Kanellopoulos AJ, Asimellis G. Epithelial remodeling after femtosecond laser-assisted high myopic LASIK: comparison of stand-alone with LASIK combined with prophylactic high-fluence cross-linking. Cornea. 2014;33:463-469.
13. Qazi MA, Roberts CJ, Mahmoud AM, Pepose JS. Topographic and biomechanical differences between hyperopic and myopic laser in situ keratomileusis. J Cataract Refract Surg. 2005;31:48-60.
14. Kanellopoulos AJ, Khan J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: Initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J Refract. Surg. 2012;28 (11 suppl):S837-840.
15. Tamayo GE. Predictable visual outcomes with accelerated corneal cross-linking concurrent with laser in situ keratomileusis. J Cataract Refract Surg. 2012;38(12):2206.
Peter S. Hersh, MD
• Cornea and Laser Eye Institute-Hersh Vision Group, Teaneck, New Jersey
• professor of clinical ophthalmology and director of cornea and refractive surgery, Rutgers Medical School, Newark, New Jersey
• visiting research collaborator, Princeton University, Princeton, New Jersey
• (201) 692-9434; www.vision-institute.com
• financial disclosure: medical monitor for Avedro


