There is a public desire and a commercial market for devices and surgical procedures that change the natural color of the iris. According to Stroma Medical (stromamedical.com), for example, the Stroma procedure turns brown irides a shade of blue by using a cold laser device to promote macrophagic removal of anterior iris pigment. No data on the safety or efficacy of this device were available at the time of writing, although a trial is planned outside the European Union and US territories.
AT A GLANCE
• There is a market for devices and surgical procedures that change the natural color of the iris.
• Interested people will travel outside the United States and European Union to receive implants such as the BrightOcular prosthetic iris device, which can cause long-term complications such as corneal decompensation, cataract, recurrent uveitis, anterior chamber hemorrhages, glaucoma, iris atrophy, and ectopia uveae.
• The authors describe their approach to removing these devices safely.
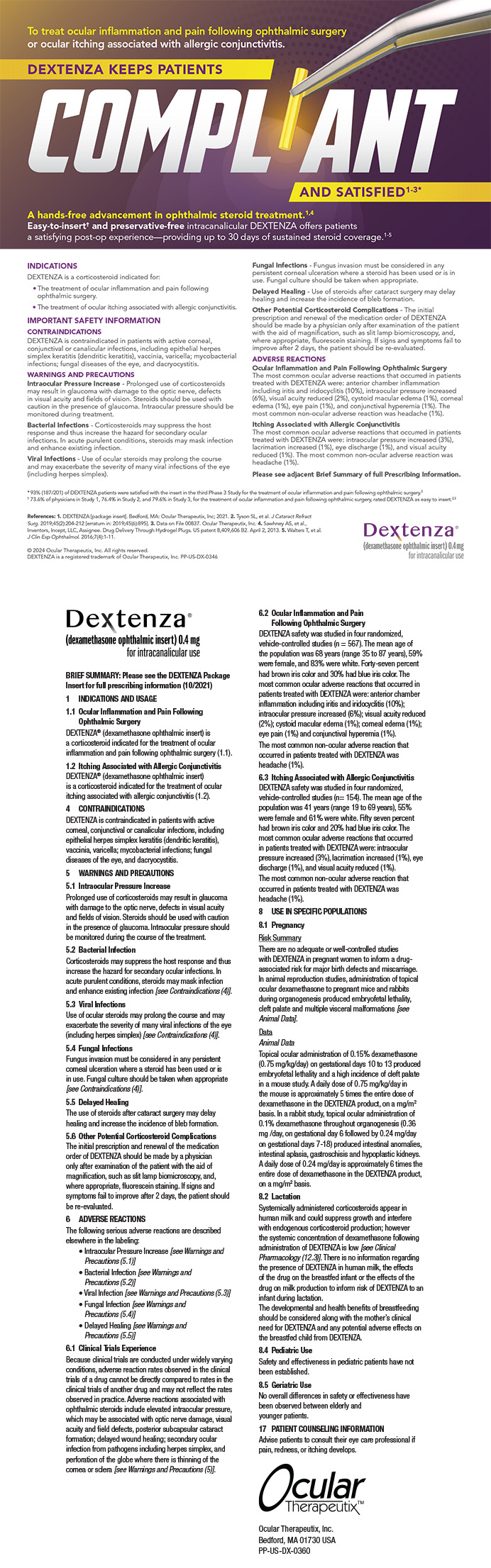
Cosmetic implants such as the BrightOcular prosthetic iris device (Stellar Devices; Figure 1) are currently available and widely marketed to change the iris’ color. These implants are promoted on various Internet channels, including YouTube. Neither this device nor its predecessor, the NewColorIris (Kahn Medical Devices), is licensed for use in the United States or the European Union. Instead, residents of those countries typically travel elsewhere for surgery. There are no available safety data for either product. Neither is there an accurate estimate of the number of devices implanted. Unfortunately, these devices represent a major public safety concern: both have been widely reported in the medical literature as causing significant morbidity, including uveitis, glaucoma, cataract, and corneal decompensation.1-10
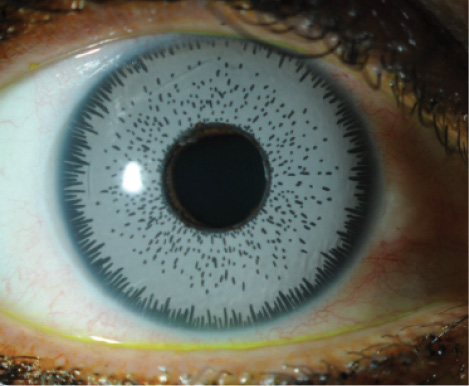
Figure 1. BrightOcular implant in situ.
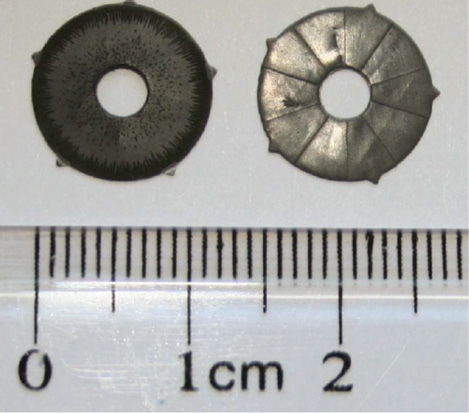
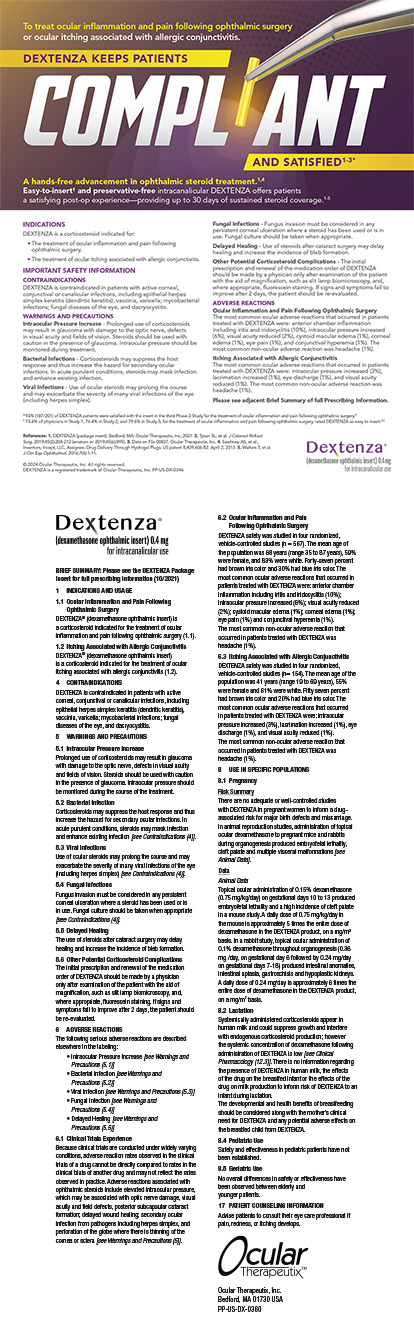
Figure 2. Posterior grooves and spiked protrusions are visible on this explanted BrightOcular cosmetic iris implant.
BACKGROUND
The NewColorIris was patented in 2006 (US patent 7,025,781 2B), and interested people traveled to Panama to receive the device. As of 2010, more than 700 procedures had been performed.10 The implant consisted of a silicone plate with a diameter of 15 mm, a thickness of 0.16 mm, a pupillary aperture of 3.5 mm, and a total of six anchoring hinges. Manufacturing of this product appears to have ceased, but it was replaced almost immediately by the BrightOcular device.
The newer cosmetic iris implant has patented posterior grooves (Figure 2) that the company claims allow better flow of aqueous and minimize iris chafing (US patent 8,197,540). The BrightOcular device has an overall diameter of 11.5 to 13.5 mm, and its thickness varies from 0.3 to 0.5 mm along sectorial posterior grooves. It has five rounded triangular edges that are 0.12 to 0.14 mm thick and 0.8 to 1 mm long. The company’s official website (brightocular.com) and associated surgical videos attest to the device’s safety by mentioning that the patent for the implant and its silicone material is approved. The device is not FDA approved, however, and there are no data in the literature to substantiate its safety.
COMPLICATIONS
Significant complications arising from anterior chamber iris implants have been widely reported. There is a general consensus among ophthalmologists that these devices should not be implanted and that they can cause long-term problems even years after implantation.1 In our experience, the BrightOcular artificial iris can cause corneal decompensation, cataract, recurrent uveitis, anterior chamber hemorrhages, glaucoma, iris atrophy, and ectopia uveae. Many of these complications can occur simultaneously and necessitate the implant’s removal. Reported secondary surgeries required after explantation include Descemet stripping automated endothelial keratoplasty, cataract extraction with IOL placement, trabeculectomy, implantation of a glaucoma drainage device, and penetrating keratoplasty.1
The complications associated with cosmetic iris implants likely arise from the devices’ placement against the iris within the anterior chamber. Iris chafing can lead to localized trauma that causes uveitis-glaucoma-hyphema syndrome, which in turn leads to iris atrophy and ectopia uvaea. Glaucoma may result from the formation of peripheral anterior synechiae and damage to the trabecular angle. Recurrent inflammation together with required corticosteroid therapy leads to cataract formation. As with other anterior chamber devices, slow attrition of corneal endothelial cells occurs through contact of the implant with the corneal periphery.
SURGICAL EXPLANTATION TECHNIQUE
Overview
During implantation, the BrightOcular device is folded and introduced through a limbal incision. Once it enters the anterior chamber, the implant unfolds to its full size. Complications related to these implants necessitate their explantation. It is important for surgeons to remove these devices without further damaging anterior chamber structures or precipitating corneal decompensation, because endothelial cell numbers may be depleted. Adhesions may have formed between the device and the underlying iris, which will make pulling the implant out through a clear corneal incision complicated and risk further iris trauma or root tears. Moreover, the implant may buckle anteriorly and traumatize the corneal endothelium as it is pulled out of the eye.
Based on our experience, we recommend the following steps to safely remove the BrightOcular device:
No. 1. Perform specular microscopy. We begin by performing specular microscopy to measure endothelial cell density in these cases so as to assess the risk of corneal decompensation.
No. 2. Attempt to visualize the iris. Because the iris is often not visible beneath the implant, it is important to avoid inadvertently damaging this tissue during cutting maneuvers. In some cases, preoperative pupillary constriction with 2% pilocarpine or intraoperative acetylcholine (Miochol-E; Bausch + Lomb) can allow early visualization of the iris.
No. 3. Break adhesions. The BrightOcular device has five anchoring protrusions that may adhere to iris tissue. We attempt to break these adhesions by injecting viscoelastic material between the cosmetic and natural iris. Gentle manipulation of the implant can confirm its freedom from adhesions.
No. 4. Segment the device, or create a tab. It is typically difficult to avoid uncontrolled buckling of the implant if it is simply dragged out of eye in toto. A number of different methods of explantation have been described. In our experience, the implant material is easily cut. It can then be trisected or bisected with microscissors and removed piecemeal. Alternatively, we have removed the implant by making two partial-thickness incisions to create a tab opposite the corneal entry, which we then grasp with a microforceps so as to withdraw the implant from the eye. The relieving incisions avoid anterior buckling. To protect the corneal endothelium, we will position an instrument such as an iris repositor anterior to the implant as it is withdrawn if needed.
No. 5. Address synechiae. Peripheral anterior synechiae may have formed in the trabecular angle. It is important to attempt viscodissection at the time of the device’s explantation, as demonstrated by Ike Ahmed, MD.
IRIS RECONSTRUCTION
Secondary surgical procedures may be undertaken at the time of a cosmetic iris implant’s removal, but it may be better to wait until the eye has recovered from the device’s explantation. Reconstruction of the underlying natural iris, if disfigured, can be achieved through suture repair or an appropriate medical cosmetic iris implant such as the CustomFlex (HumanOptics; Figure 3) placed behind the iris and secured in the sulcus space. Unfortunately, devices such as this one are currently available in the United States only via a compassionate use exemption from the FDA and approval of a local institutional review board.

Figure 3. A BrightOcular device prior to explantation (A). After the implant’s removal, the underlying iris is disfigured with ectopia uveae and corectopia. The patient also has a cataract and suffers from severe glare (B). The eye after cataract surgery and implantation of a CustomFlex artificial iris in the sulcus (C).
CONCLUSION
The well-documented complications of cosmetic implants may lead to permanent ocular damage. National ophthalmic bodies should attempt to increase public awareness of the risks of these devices. Physicians such as ourselves have attempted to highlight these risks in the local and national press, on television both in the European Union and the United States, and via social media outlets. We believe that companies such as Stellar Devices should be required to provide objective data on the number of devices implanted and actual complication rates.
1. Hoguet A, Ritterband D, Koplin R, et al. Serious ocular complications of cosmetic iris implants in 14 eyes. J Cataract Refract Surg. 2012;38:387-393.
2. Hull S, Jayaram H, Mearza AA. Complications and management of cosmetic iris implants. Cont Lens Anterior Eye. 2010;33(5):235-238.
3. McCall D, Hamilton A, Grigg J, et al. Severe glaucoma and vision loss due to cosmetic iris implants. Med J Aust. 2015;202:181.
4. Arthur SN, Wright MM, Kramarevsky N, et al. Uveitis-glaucoma-hyphema syndrome and corneal decompensation in association with cosmetic iris implants. Am J Ophthalmol. 2009;148:790-793.
5. Thiagalingam S, Tarongoy P, Hamrah P, et al. Complications of cosmetic iris implants. J Cataract Refract Surg. 2008;34:1222-1224.
6. Anderson JE, Grippo TM, Sbeity Z, et al. Serious complications of cosmetic NewColorIris implantation. Acta Ophthalmol. 2010;88:700-704.
7. Sikder S, Davis SW, Patel VP, et al. Complications and management of NewColorIris implantation in phakic eyes. J Refract Surg. 2011;27:239-240.
8. George MK, Tsai JC, Loewen NA. Bilateral irreversible severe vision loss from cosmetic iris implants. Am J Ophthalmol. 2011;151:872-875.
9. Luk S, Spiteri A, Muthasamy K, et al. Cosmetic iris implantation complicated by secondary angle closure. Cont Lens Anterior Eye. 2015;38(2):142-143.
10. Mansour AM, Ahmed II, Eadie B, et al. Iritis, glaucoma and corneal decompensation associated with BrightOcular cosmetic iris implant [published online ahead of print December 30, 2015]. Br J Ophthalmol.
doi:10.1136/bjophthalmol-2015-307295.
Romesh Angunawela, MD, FRCOphth, FRCS
• consultant eye surgeon, Department of Cornea and Refractive Surgery, Moorfields Eye Hospital, London
• romesh.angunawela@moorfields.nhs.uk; Twitter @Your_2eyes
• financial interest: none acknowledged
Ali Mearza, FRCOphth
• clinical director of ophthalmology and lead consultant eye surgeon, Department of Ophthalmology, Imperial College Healthcare NHS Trust, London
• ali.mearza@imperial.nhs.uk; Twitter @AliMearza
• financial interest: none acknowledged