
Ophthalmology is facing some difficult challenges in the coming years in the form of a swelling patient population but a declining potential for reimbursement. Fees for commonly performed procedures and diagnostics are being drastically reduced, and at the same time, overarching changes in the structure of how Medicare operates are de-emphasizing the role of procedures in managing patients. A greater interest in preventive medicine is not necessarily a bad thing, but it does require an adjustment to the kinds of services ophthalmologists offer in order to maintain economic viability.
One strategy that has been advanced is to increase efficiency to increase patient volume, with the notion that higher throughput will make up for any shortcomings in revenue. Another strategy, and one that is not mutually exclusive, would be to attract new types of patients to the practice through novel offerings, particularly if the offerings are elective, fee-based services. This has been one of the motivating factors in incorporating aesthetic procedures into ophthalmology, a field that already deals with a number of individuals interested in quality-of-life upgrades in the form of LASIK, cataract surgery, blepharoplasty, and reconstructive surgery.
Although aesthetics are important service offerings in their own right, some of these complementary services can serve the interest of ocular health. The interplay between cutaneous rosacea, ocular manifestations, and dry eye disease (DED) offers one example where treatment for the skin condition may be medically prudent for reducing the impact of the ocular consequences.
A Natural Crossover
Ophthalmologists are trained experts in treating problems pertaining to the skin surrounding the eyes, as there are several dermatologic conditions that either have ocular symptoms or the potential to invade the eye, including eczema, atopic dermatitis, and lid lesions. Being able to differentiate potentially devastating skin diseases around the eye (including basal and squamous carcinoma, melanoma, and sebaceous carcinoma) from noncancerous lesions (squamous papilloma, seborrheic keratosis, epidermal inclusion cysts, or chalazia) is a necessary part of performing a comprehensive eye examination. Thus, it is not too much of a stretch to imagine making a leap from dealing with ophthalmic patients to aesthetic and cosmetic procedures. After all, Botox (onabotulinumtoxinA; Allergan) and Latisse (bimatoprost ophthalmic solution; Allergan) were pioneered by ophthalmologists before moving to the aesthetics dermatology market.
The overlap of treatment modalities goes in the other direction as well. In my practice, I use several laser platforms for the treatment of ocular skin conditions that are also widely used by dermatologists. One such device, the Lumenis M22 intense pulsed light (IPL) multimodal platform, is a versatile treatment modality that is applicable to many dermatologic and ophthalmic conditions. The FDA has approved the treatment of more than 30 skin indications using the Lumenis M22 IPL with Optimal Pulse Technology (OPT). The M22 platform is equipped with a variety of predefined presets (fluence, pulse duration, and other parameters) designed for optimal treatment of different skin conditions; however, the settings are also customizable, serving to broaden the applicability of this device. The user can adjust these settings and use various wavelength filters to target different chromophores, depths, and skin types.
IPL For Rosacea
One of the applications for IPL therapy is facial rosacea, which is an entity that ophthalmologists should be aware of for its potential to have an impact on the skin around the eyes. Rosacea’s presentation on the skin often precedes or is concurrent with ocular manifestations. In 20% of cases, ocular rosacea precedes facial rosacea.1 Ocular rosacea can be a precursor to or a trigger of meibomian gland dysfunction (MGD) and resultant DED, with the most probable mechanism being the spread of inflammation to the eyelids.
It is well established that IPL has a beneficial mechanism of action with regard to rosacea, suggesting the treatment’s utility in other inflammatory conditions. In rosacea, abnormal blood vessels (telangiectasia) release pro-inflammatory agents and matrix metalloproteinases, thus contributing to a chronic state of inflammation that threatens the eyelids and ocular surface. IPL energy is selectively absorbed in the hemoglobin of these abnormal vessels, leading to their destruction and to the reduction of this inflammatory source.
In the absence of treatment, cutaneous rosacea can trigger MGD. As many as 80% of patients with rosacea manifest some degree of MGD.2 Cutaneous rosacea may also be associated with blepharitis (eyelid inflammation) and rosacea keratitis (corneal involvement), each of which is as an independent risk factor for the onset of MGD and DED. There are several pathways whereby rosacea itself can trigger MGD. For example, as epithelial turnover increases in rosacea,3 dead epithelial cells form debris that can accumulate near the eyelids and clog the meibomian glands’ orifices, thus disrupting the normal flow of meibum. Equally as likely, cytokines and chemokines released by newly formed aberrant blood vessels initiate an inflammatory cascade that invades the meibomian glands via the rich vasculature of the eyelids.4 Persistent inflammation of the meibomian glands eventually result in atrophy and drop-out of the glands.
Rosacea may also have indirect pathways to MGD. Skin edema, often accompanying rosacea, boosts the proliferation of Demodex mites. Demodex skin parasites are infested with Bacillus olerinus bacteria. When the bacterial load in and around the eyes rises, expression of Toll-like receptor 2 increases, thus enhancing production of anti-microbial peptides that result in inflammation and additional vascular changes.5 Additionally, wastes and byproducts of the proliferating bacterial microenvironment may clog the meibomian glands and have a negative impact on the viscosity of meibum.
Medical Benefit From an Aesthetic Treatment
Rosacea presents a fascinating case where treatment of a supposed aesthetic condition can have implications for facilitating better ocular health. Work by Rolando Toyos, MD, showed that patients who have had IPL treatments for various skin conditions, including rosacea, reported significant improvement in their ocular symptoms and signs, in some cases including resolution of concomitant MGD.6 There is a growing body of literature to suggest that IPL is a potentially effective treatment for MGD.6-9
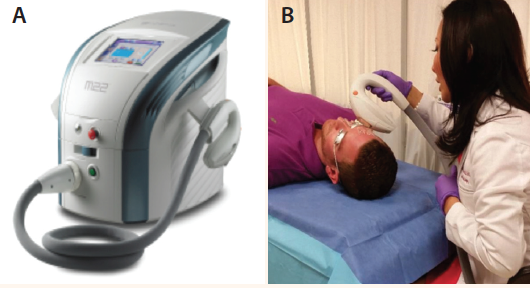
Figure 1. The Lumenis M22 IPL with OPT system (A) and a patient being treated for rosacea with the system (B).

Figure 2. Before and after photographs of a patient with moderate rosacea who was treated with the Lumenis M22 IPL with OPT system (four sessions, 1 month apart).
We are conducting an ongoing trial in our clinic looking at the potential for IPL to treat MGD (see Intense Pulsed Light Therapy for MGD-Related Dry Eye). So far, we have obtained impressive results, which confirm the versatility of the M22 platform. It should be noted that although IPL is a highly effective treatment for cutaneous and ocular rosacea (Figures 1 and 2), and although patients with ocular rosacea who receive IPL often report improvement of dry eye symptoms, the presence of rosacea was not necessary for enrollment in our study. This is important, because it means that IPL’s use is not limited to a subset of patients with both conditions; rather, it appears to be applicable to patients with both or either ocular rosacea and MGD/evaporative DED.
As eye care providers look to an uncertain future with regard to reimbursement, diversifying one’s offerings is a strategy worth considering. Ophthalmologists are already familiar with many of the skin conditions that affect the areas around the eye, and they already deal with patients who are accepting of cosmetic procedures. I mentioned earlier that attracting new patients to the practice was one strategy for building more clientele. Many of the patients who would be accepting of aesthetic procedures, however, are already in the average ophthalmic practice seeking refractive surgery and asking about premium IOLs for their cataract surgery. More urgently, DED and MGD are both prominent conditions that are growing in relevance to the eye care field. They are important in their own right because of the visual symptoms they can cause, and they are doubly important in the context of surgical patients, as untreated MGD is a risk factor for inaccurate keratometry and biometry, and, therefore, for incorrect IOL power selection. n
1. Lambreghts KA, Melore GG. Diseases of the Eyelids. In: Bartlett JD, Jaanus SD, eds. Clinical Ocular Pharmacology, 5th ed, St. Louis, Missouri: Butterworth-Heinemann (Elsevier), 2008;388.
2. Viso E, Rodríguez-Ares MT, Abelenda D, et al. Prevalence of asymptomatic and symptomatic meibomian gland dysfunction in the general population of Spain. Invest Ophthalmol Vis Sci. 2012;53(6):2601-2606.
3. Henriquez AS, Korb DR. Meibomian glands and contact lens wear. Br J Ophthalmol. 1981;65 (2):108-111.
4. Gerber PA, Buhren BA, Steinhoff M, et al. Rosacea: the cytokine and chemokine network. J Investig Dermatol Symp Proc. 2011;15(1):40-47.
5. Yamasaki K, Gallo RL. Rosacea as a disease of cathelicidins and skin innate immunity. J Investig Dermatol Symp Proc. 2011;15(1):12-15.
6. Toyos R, McGill W, Briscoe D. Intense pulsed light treatment for dry eye disease due to meibomian gland dysfunction: a 3-year retrospective study. Photomed Laser Surg. 2015;33(1):41-46.
7. Vegunta S, Patel D, Shen JF. Combination therapy of intense pulsed light therapy and meibomian gland expression (IPL/MGX) can improve dry eye symptoms and meibomian gland function in patients with refractory dry eye: a retrospective analysis. Cornea. 2016;35(3):318-322.
8. Craig JP, Chen YH, Turnbull PR. Prospective trial of intense pulsed light for the treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2015;56(3):1965-1970.
9. Vora GK, Gupta PK. Intense pulsed light therapy for the treatment of evaporative dry eye disease. Curr Opin Ophthalmol. 2015;26(4):314-318.
Sheila C. Barbarino, MD
• cosmetic plastic surgeon at Dell Laser Consultants, Austin, Texas
• (310) 402-2255; sheila.barbarino@gmail.com; drsheilabarbarino.com
• financial disclosure: consultant to Lumenis


