
Posterior capsular opacification (PCO) is one of the most common complications of otherwise uneventful cataract surgery. PCO occurs after cataract surgery when lens epithelial cells from the area of the capsular fornix proliferate and migrate across the posterior capsule. The contraction of these cells can cause fine wrinkles or folds and fibrotic opacities in the posterior capsule. When significant PCO obscures the visual axis and interferes with patients’ vision, an Nd:YAG laser capsulotomy is performed to create an opening in the posterior capsule, thereby improving visual acuity and quality of vision.
Approximately one-third of patients who undergo cataract surgery and receive a posterior chamber IOL develop significant PCO that requires a laser capsulotomy in the years following cataract surgery. Knowing when to YAG and when not to is helpful to reduce the risk of complications (discussed later) and to increase patients’ chances of improved vision.
COMPLICATIONS
Complications after Nd:YAG laser capsulotomy are rare. Retinal detachment can develop in the months following the capsulotomy, with the reported incidence ranging from less than 1% to slightly more than 3%. Cystoid macular edema (CME) can also occur after laser capsulotomy.
Although Nd:YAG laser capsulotomies are successful in the majority of patients and the rate of complications is low, it is important to keep in mind the potential risk of complications when performing the procedure. Care must be taken to focus the laser precisely in order to avoid damaging the IOL optic. Extensive pitting of the IOL optic can lead to visual symptoms.
Various lenses are available to help precisely focus the laser beam on the posterior capsule. A posterior offset of 100 to 200 µm also often helps to prevent damage to the posterior surface of the IOL, and the minimum laser power necessary to create an opening in the posterior capsule should always be used.
WHEN TO YAG
Indications. The most common reason for performing an Nd:YAG laser capsulotomy is when significant fibrosis, wrinkling, or opacification of the posterior capsule occurs. When PCO causes decreased vision, glare, or difficulties with visual function, a laser capsulotomy is indicated. The procedure is also indicated when PCO compromises the clinician’s view of the fundus in a patient with retinal disease.
Laser capsulotomy also may be considered for patients who develop capsular block syndrome and capsular bag distention syndrome in the period immediately after cataract surgery. Capsular block syndrome results from a partial occlusion of the anterior capsulorhexis opening by the IOL, which can cause a buildup of material posterior to the lens optic. Capsular distention syndrome can occur when a retained OVD occupies the space between the posterior surface of the IOL optic and the posterior lens capsule.
Patients with these syndromes often report blurred or cloudy vision. Forward movement of the IOL optic can also induce myopia. An Nd:YAG laser capsulotomy creates an opening in the posterior lens capsule that allows material trapped behind the optic to flow into the anterior vitreous, thus decompressing the area behind the IOL and alleviating capsular bag distention syndrome and capsular block syndrome.
Timing. Patients who develop capsular distention syndrome or capsular block syndrome may require treatment immediately after cataract surgery.
In contrast, some patients have a persistent posterior subcapsular cataract or fibrosis along the posterior capsule that cannot be removed during cataract surgery. In this and other situations where a capsulotomy is not immediately necessary, it is often recommended to postpone the procedure until the blood-aqueous barrier is reestablished. This delay decreases the risk of inflammation after laser capsulotomy. It is unclear exactly when the blood-aqueous barrier re-forms after surgery, but it is reasonable to wait approximately 6 to 8 weeks following cataract surgery before performing a routine laser capsulotomy.
WHEN NOT TO YAG
Inflammation and CME. A laser capsulotomy should not be performed in the presence of active or ongoing intraocular inflammation. It is also prudent to wait for possible resolution of CME before performing a laser capsulotomy.
IOL exchange. One of the most common reasons for not performing a laser capsulotomy is if there is a reasonable possibility of having to exchange an IOL. This problem arises most frequently in patients who receive multifocal IOLs and experience dysphotopsias postoperatively. Some surgeons advocate for an early laser capsulotomy in this situation to try to resolve patients’ symptoms. It is crucial, however, to differentiate visual symptoms caused by true PCO from symptoms that may be related to the IOL itself. Patients who are experiencing dysphotopsias, especially significant positive dysphotopsias, often require an IOL exchange. Those experiencing significant negative dysphotopsias may achieve neural adaptation over time.
If a piggyback IOL procedure is being considered, if the original IOL has become displaced, if IOL manipulation is being contemplated, or if an IOL exchange is a possibility, it is important to hold off performing a laser capsulotomy. An open posterior capsule makes these procedures much more difficult to perform.
Endophthalmitis. The most common cause of chronic endophthalmitis following cataract surgery is a low-grade infection located within the capsular bag secondary to Propionibacterium acnes. This condition is uncommon and is sometimes misdiagnosed as PCO. It is important to evaluate patients carefully at the slit lamp to look for signs of P acnes within the capsular bag. In these cases, a fluffy white infiltrate is often observed between the capsular bag and the posterior lens capsule (Figure). A laser capsulotomy should be avoided because opening the posterior capsule can allow dissemination of the bacteria into the vitreous, which may lead to endophthalmitis instead of keeping the infection localized to the capsular bag.
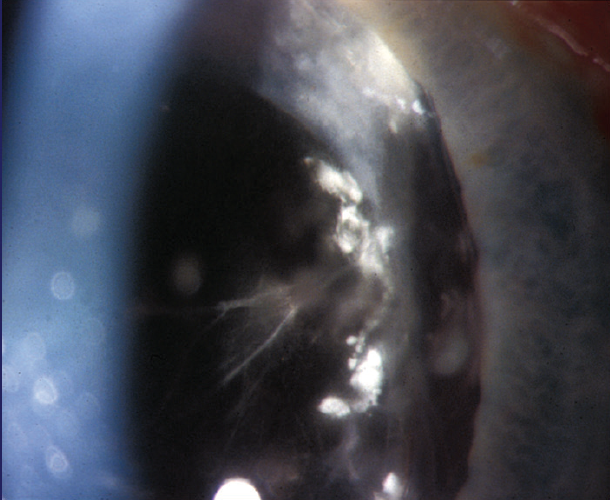
Figure. P acnes is visible between the capsular bag and the posterior lens capsule.




