
Keratoconus is a progressive thinning of the cornea that results in irregular astigmatism. Recent calculations show a prevalence that is five to 10 times higher than was reported in the literature a decade ago,1 and it has become apparent that the actual number is even higher. This increased recognition of the presence of keratoconus is likely due to the advent of new topographic technologies, routine screening of topography and tomography prior to cataract surgery, and increased awareness of the subtle signs of forme fruste keratoconus.
As patients with cataracts continue to have higher visual demands, we will see more patients with keratoconic eyes who desire the best refractive outcomes.2 Achieving excellent outcomes in these patients is more difficult for a variety of reasons, one of which is the challenges of IOL power calculations. In this article, I discuss some of the pearls and pitfalls in lens power calculations in keratoconic eyes undergoing cataract surgery.
CHALLENGES IN IOL CALCULATION
Eyes with keratoconus often end up hyperopic after cataract surgery. This can be frustrating for patients because most of them were previously myopic. One causative factor is irregular keratometry (K). With a variety of types and grades of keratoconus, it is unclear which K readings are best to use in IOL power calculations. Patients with keratoconus sometimes have long axial lengths, which can further contribute to hyperopic error.
Additionally, the anterior chambers in these eyes are often not proportional to the effective lens position. Assumptions made in IOL calculations for normal eyes are not true for these eyes. Watson et al showed that hyperopic error was low in eyes with mild (K < 48.00 D) and moderate (K = 48.00–55.00 D) keratoconus after cataract surgery, but that errors were more unpredictable in severe keratoconus.3
This past year, my colleagues and I compared the Barrett, Olsen, and Holladay 1 formulas in a cohort of eyes with keratoconus.4 All formulas showed a hyperopic refractive predictive error, but the Barrett formula had the lowest absolute mean and median refractive predictive errors. Further, there was a linear relationship using simulated K (simK) with the Holladay 1 formula up to about 47.00 D, and anything steeper resulted in a larger range of results.4
Based on our findings, we now aim for a refractive target of -0.75 D in eyes with mild to moderate keratoconus and -1.25 D for corneas steeper than 47.00 D, with the understanding that these patients may have myopic or hyperopic surprises (Figure 1).
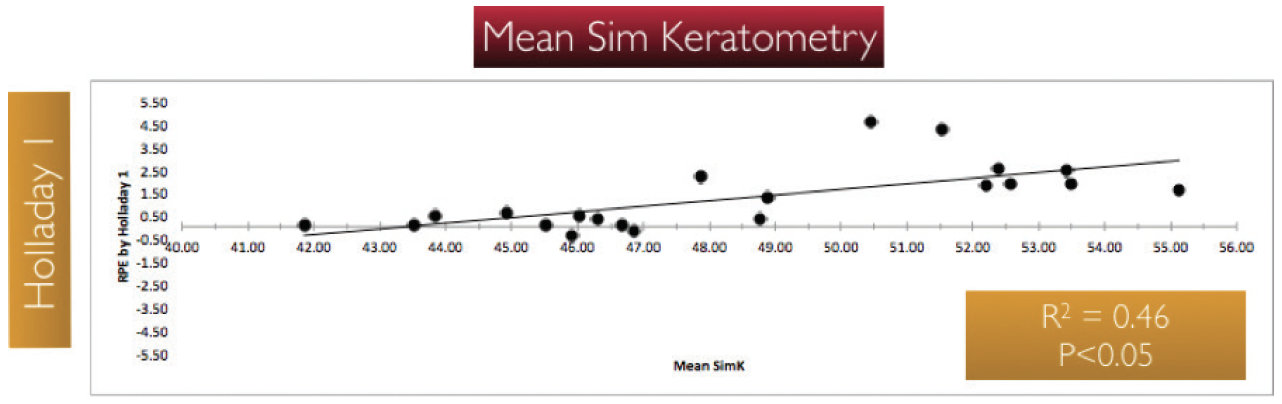
Figure 1. Relationship of refractive predictive error using the Holladay 1 formula related to mean simK on Galilei (Ziemer) topography. As the average simK increases, the error becomes more hyperopic. Once the keratometry is greater than 47.00 D, the values become less correlated.
CONTACT LENSES
Obtaining accurate K readings may be difficult in keratoconic patients who wear contact lenses, whether toric soft lenses, hybrid lenses, or rigid gas permeable lenses. These patients do not like to be out of their contact lenses for very long, but they often need to undergo multiple measurements because contact lens warpage can take a long time to ameliorate. Often, when I tell patients that, ideally, they should stop wearing their hard contact lenses for 1 month for every year they have worn them, they are reluctant to even undergo surgery.
I let these patients know that, if they plan to continue to wear hard contact lenses after surgery, then we can ease up on this rule. I have them remove one lens at a time for 2 weeks, take the measurements in that eye, then repeat them 1 week later. If the two measurements match, then I move on to surgery, knowing that the patient’s cornea will change even more afterward.
For those who wear scleral lenses, I am not so concerned, although I do ask these patients to stop wearing the lenses for at least 5 days before surgery. Because scleral lenses do not rub on the cornea, they do not cause the same amount of corneal warpage, and we often see normalization of the cornea within 24 hours. Additionally, these patients often go back into their scleral lenses, which provide comfort and correction after surgery.
It is important to note that if a patient may go back into contact lenses after surgery, the surgeon should aim for a more myopic target, as it is much easier to fit a myopic lens to correct astigmatism.
TORIC IOLS
The traditional thinking has been to avoid using toric IOLs in keratoconic eyes because they could increase the eyes’ already irregular astigmatism. However, the availability of CXL and topography-guided PRK may allow more patients to receive toric IOLs at the time of cataract surgery.
If the patient’s cornea is not changing, due either to progression or regression from recent CXL, and if the central 3 mm on his or her topography shows regular astigmatism, one can consider use of a toric lens.5 The surgeon should explain to the patient that this is an astigmatism-debulking procedure, rather than one that will correct all errors. The patient may still need glasses or contact lenses for the best vision, but outcomes can be very good. It is important to watch for progression of keratoconus after surgery. The risk of progression is thought to be lessened by use of a small limbal or scleral tunnel incision.
For patients who are happy in hard contact lenses or scleral lenses, be cautious in placing a toric IOL. It is important to counsel these patients that their vision with a toric IOL is never going to be as good as it is with their hard contact lenses. Further, it is hard to get good topographies in these patients, as they tend to be long-term lens wearers, and the ability to reverse contact lens warpage is uncertain. However, if the patient states that he or she is interested in being less dependent on contact lenses and is willing to come in for multiple measurements without the lenses, I may consider a toric lens. If, on the other hand, patients say they want better vision, I advise them that they may need to upgrade to a scleral or a reverse-geometry lens.
REFRACTIVE SURPRISES
Our ace in the hole with unexpected refractive results after cataract surgery is the ability to perform a corneal refractive surgery touchup. Patients with keratoconus, unfortunately, cannot undergo corneal ablation without increasing the risk of further ectasia; therefore, a refractive surprise in a patient with keratoconus may result in the need for IOL exchange.
In one study of keratoconic eyes undergoing refractive lens exchange to correct myopia associated with keratoconus, 26% of keratoconic eyes had to have immediate IOL exchange, and 6% of eyes required a postoperative IOL exchange due to refractive surprise.6 The author recommended use of an intraoperative handheld autorefractor to improve refractive outcomes in these types of eyes.
SPHERICAL ABERRATION
Even when the correct IOL power is determined, the surgeon should be aware of the positive or negative sphericity of the IOL chosen. The keratoconic cornea is unique in its sphericity. Most corneas have increased positive spherical aberration over time, but the cone in the keratoconic cornea creates a negative spherical aberration, much like a cornea after hyperopic LASIK. Because most IOLs have a slight negative spherical aberration, one should consider choosing a true aspheric lens such as the »enVista IOL or the »SofPort AO Aspheric Lens (both Bausch + Lomb) or a positive spherical lens such as the »Sensar (Johnson & Johnson Vision).
CONCLUSION
We will continue to see more keratoconic patients in our cataract evaluations. The expectations of these patients can be just as high as those of other refractive cataract surgery patients. To obtain the best outcomes for these patients, surgeons must perform proper patient counseling, make careful preoperative measurements, adjust the refractive target based on calculations made with multiple formulas, and have a plan in place to address refractive surprises.
1. Godefrooij DA, de Wit GA, Uiterwaal CS, et al. Age-specific incidence and prevalence of keratoconus: a nationwide registration study. Am J Ophthalmol. 2017;175:169-172.
2. Thebpatiphat N, Hammersmith KM, Rapuano CJ, et al. Cataract surgery in keratoconus. Eye Contact Lens. 2007;33:244-246.
3. Watson MP, Anand S, Bhogal M, et al. Cataract surgery outcome in eye with keratoconus. Br J Ophthalmol. 2014;98:361-364.
4. Khandelwal SS, Montes de Oca I, Weikert MP, Wang L, Koch DD. Predictive accuracy of intraocular lens calculation formulas in eyes with keratoconus. Paper presented at: American Society of Cataract and Refractive Surgery Annual Meeting; May 5-9, 2017; Los Angeles.
5. Hashemi H, Heidarian S, Seyedian MA, et al. Evaluation of the results of using toric IOL in the cataract surgery of keratoconus patients. Eye Contact Lens. 2015;41:354-358.
6. Leccisotti A. Refractive lens exchange in keratoconus. J Cataract Refract Surg. 2006;32:742-746.




