A 43-year-old man presents for a refractive surgery evaluation. The patient is a health care worker by trade. He enjoys an active lifestyle and plays video games in his free time.
The patient typically wears contact lenses but reports recent problems with ocular dryness and irritation. He experiences mild relief with artificial tears and wears over-the-counter readers to help him see up close.
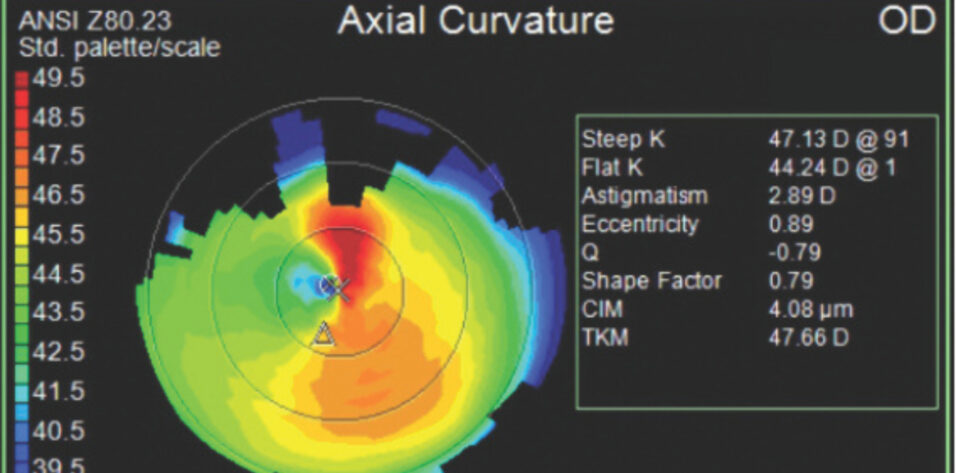
Upon presentation, his manifest refraction is -9.00 -2.00 x 180º = 20/20 OD and -11.00 -1.50 x 175º = 20/30 OS. The cycloplegic refraction is similar. A slit-lamp examination finds significant superior corneal pannus located about 3 to 4 mm vertically from the limbus and toward the visual axis in each eye. Both eyes have grade 1+ to 2+ superficial punctate keratitis. The maximum dilated pupil size is 7 mm in each eye. The results of a dilated fundus examination and all other clinical examination characteristics are normal. Imaging results and measurements are shown in Figures 1 and 2.

Figure 1. Imaging for the right (A, C) and left (B, D) eyes.

Figure 2. Measurements for the right and left eyes.
How would you proceed?
— Case prepared by Arjan Hura, MD

EVA KIM, MD
During a typical consultation for an EVO ICL (STAAR Surgical), I tell patients that ideal candidates for the technology meet two criteria: (1) excellent eye health and (2) ocular anatomy that is compatible with ICL insertion.
I perform a comprehensive dilated eye examination on all my patients. They also undergo diagnostic testing, including fundus photography, OCT of the macula, and retinal nerve fiber layer testing. Certain abnormal findings either require treatment preoperatively or, occasionally, disqualify the patient for an ICL.
I emphasize to patients the importance of ocular anatomy. An anterior segment that is too small or crowded might not allow safe placement of an ICL. An anterior segment that is too large might permit the implant to move or rotate—an unacceptable situation if the patient requires a toric model—and would allow the ICL to sit directly adjacent to the crystalline lens, which is not recommended.
I would tell this patient that initial biometry measurements categorize his anterior segment as small. I would explain that, although this does not exclude him as a candidate, there might not be enough room in his eyes to house an additional lens.
All my ICL consultation patients undergo ultrasound biomicroscopy with augmented intelligence (UBM AI, Sonomed Escalon) coupled with ICL Guru testing (Revai) to determine precise lens sizing. Not only does the testing determine the precise size of the ICL to be placed in the eye, but more importantly, it also determines candidacy for the technology. With the use of UBM AI and ICL Guru software, I was able to implant a spherical ICL safely in a patient with an aqueous depth of 2.3 mm in each eye.

JOSEPH LING, MD
This case highlights both the amazing options available for vision correction and their limitations.
The poor quality of the patient’s topography is likely the result of tear film instability and lid interference. Tomography reveals relatively thin corneas for the degree of refractive correction needed.
The combination of borderline corneal thickness, dry eye, and pannus makes him a poor candidate for laser vision correction. An anterior chamber depth (ACD) of 2.40 mm OD and 2.52 mm OS is too shallow for the safe implantation of an EVO ICL. With those options ruled out, a refractive lens exchange (RLE) is the only surgical alternative left, but the patient’s age and high myopia increase the risk of retinal detachment. A thoughtful conversation about surgical risks—ideally involving a retina specialist—would therefore be essential. If the patient is highly motivated and willing to accept the risks, RLE with presbyopia-mitigating strategies could deliver an excellent outcome. Alternatively, it is worth remembering that retinal detachment risk decreases with age as the vitreous matures. Waiting is a strategy in itself.
It should be noted that the pannus might be the eye’s way of saying “bad fit” or “too much wear” of the contact lenses. A refit with daily disposable contact lenses could restore comfort and improve the patient’s surgical candidacy down the line.
Not every case ends in surgery. Sometimes, the best move is patience.

ROGER ZALDIVAR, MD, MBA
I will assume that the patient is experiencing significant difficulties with his contact lens wear and wants to resolve them after several attempts to improve the health of his ocular surface. The ACD of 2.5 mm is on the low end, which could make deciding whether to implant an EVO ICL challenging.
The iridocorneal angle of 32º provides a good amount of space for positioning the ICL without causing significant risk of angle closure. The iridocorneal angle measurement is a crucial factor in assessing the anterior chamber configuration and can help mitigate the risk of postoperative complications such as increased IOP. I believe that the 32º angle combined with the use of advanced sizing methodologies such as the ICL Guru could make the patient a suitable candidate for an ICL. ICL Guru is an AI-powered tool that uses a comprehensive set of biometric data to determine the optimal lens size and vault. This methodology could help ensure that the ICL is precisely tailored to the patient's eye, thereby reducing the risk of complications and improving the likelihood of a successful outcome.
I would avoid a toric ICL because it demands highly precise sizing. Instead, two 5.5-mm limbal relaxing incisions would be made at the steepest meridian. If the residual angle is tight, it would be increased by rotating the lens vertically.
Clinical studies1,2 and my own experience have shown that, with careful planning and the use of advanced tools, ICLs can be implanted safely in eyes with slightly small ACDs. Regular follow-up visits can help detect and manage any potential issues early, ensuring the best possible outcomes.
I would thoroughly discuss the risks and benefits of surgical intervention with the patient to ensure that he is well-informed and comfortable before proceeding.

WHAT I DID: ARJAN HURA, MD
The patient and I had an extended conversation about his refractive surgery options. I explained that he was not a candidate for laser vision correction because of the large refractive error, high risk of ectasia, and potential worsening of preexisting dry eye disease. He was not interested in RLE because of the risk of postoperative retinal detachment due to his young age, long axial lengths, high myopia, and lack of posterior vitreous detachments.
We discussed EVO ICL surgery as a possible option, and I emphasized that the procedure would be off-label due to the shallow internal ACD in each eye. I explained that whether to proceed with EVO ICL surgery would depend on the results of UBM AI and ICL Guru testing, which were performed (Figure 3). The procedure can sometimes be performed successfully in an off-label manner in patients with shallow ACDs. However, due to the predicted risk of angle closure in this patient, even with the smallest-diameter EVO ICL available, I informed him he was not a candidate for the procedure.

Figure 3. ICL Guru testing shows a high likelihood of angle closure in the right (A) and left (B) eyes.
Despite advances in diagnostic and surgical technology and AI, not every patient is a surgical candidate. Sometimes, the best option for the health, safety, and longevity of a patient’s eyes and vision is to forgo surgery. First, do no harm.
1. Huang T, Zhang H, Li K. Assessment of clinical efficacy and safety of ICL implantation in patients with relatively shallow anterior chamber depth in early and midterm postoperative time. Heliyon. 2024;10(22):e39791.
2. Zaldivar R, Zaldivar R, Cummings AB, et al. Evaluating the predictive accuracy of an AI-based tool for postoperative vault estimation in phakic intraocular lens implantation. Clin Ophthalmol. 2025;19:1945-1956.