CASE PRESENTATION
A 65-year-old woman presents with a complaint of worsening vision in her left eye over the past 8 months. Recently, her husband began walking at her left to prevent her from running into anything on that side. The patient has a history of cataract surgery on the right eye only.
On presentation, her UCVA is 20/25-2 OD and hand motions OS, with no improvement on refraction. A slit-lamp examination shows an IOL in situ and grade 1+ posterior capsular opacification in the right eye and a dense brunescent lens in the left eye (Figure). The cup-to-disc ratio and the results of an examination are normal in the right eye. No view can be obtained in the left eye.
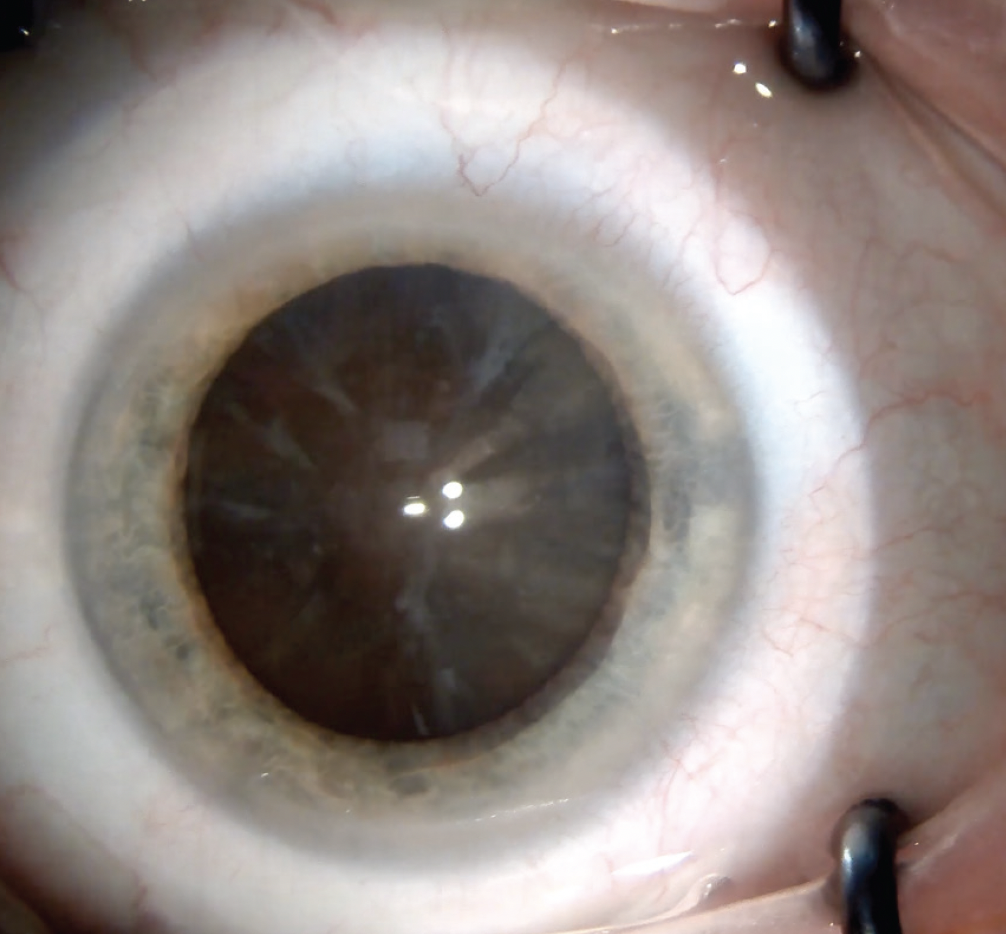
Figure. Dense brunescent cataract.
Topography measures 1.25 D of regular corneal astigmatism at 161º in the left eye. Biometry with the IOLMaster 700 (Carl Zeiss Meditec) is unable to obtain measurements in the left eye.
What questions would you ask the patient? What additional tests would you perform in the lane if she asks about the left eye’s visual potential? What studies would you obtain preoperatively? What would your surgical approach and lens choice be?
— Case prepared by Cristos Ifantides, MD, MBA

UDAY DEVGAN, MD, FACS, FRCS
Cataract surgery for the second eye is usually requested by the patient because they learned from the procedure on the first eye that their vision can be easily and painlessly restored. This case is unusual because the patient’s UCVA is 20/25 OD yet she allowed the visual acuity in her left eye to deteriorate to hand motions. The dense brunescent cataract in the left eye and her husband’s walking on her blind side to compensate are odd.
Does the patient have sensory exotropia in her nearly blind left eye? What were the biometry measurements for the left eye when the right eye underwent cataract surgery? Did both eyes ever have approximately the same refraction, or does the patient have a history of anisometropia? Is there a relative afferent pupillary defect (RAPD)? Does the left eye have a history of trauma?
Ultrasound would be performed to check for sensory exotropia, assess the posterior segment, and measure the axial length. Corneal pachymetry measurements and an endothelial cell count would be obtained because a high amount of phaco energy will be required to remove the dense cataract.
If the preoperative consultation and testing identify no red flags, phaco cataract surgery with a monofocal toric IOL would be performed on the left eye. A plano refractive target would be reasonable. If corneal endothelial weakness is identified, however, then manual small-incision cataract surgery (MSICS) would be performed instead.

BRENTON FINKLEA, MD
My first question for this patient would be, “Why was cataract surgery performed on only one eye?” Although changes in health insurance, limited access to care, and other socioeconomic factors may be elements in situations like this one, unilateral cataracts may also be overlooked in individuals who have a history of poor vision due to amblyopia, trauma, or retinal and optic nerve pathologies. Knowing the eye’s history would help me anticipate surgical challenges.
The clinical examination would include assessing the eye for an RAPD before dilation and a Purkinje tree test to evaluate visual potential. Potential acuity meters and laser interferometry tests may be ineffective in determining the visual potential of eyes with extremely dense cataracts. Immersion A-scan and B-scan ultrasound would be imperative to measure the axial length and evaluate the structure of the posterior segment.
Although modern phaco platforms can handle most cataracts, MSICS would be my preference as a safer option, particularly if zonular weakness or endothelial dysfunction is a concern. I would operate from a temporal approach and attempt to create a frown incision on the astigmatic steep axis near 160º. A scleral tunnel should induce +0.75 to +1.50 D of corneal steepening 90º away from the incision site depending on the surgical technique. With proper surgical planning, the patient should have minimal residual astigmatism after surgery.
A one-piece PMMA IOL would be implanted. A Light Adjustable Lens (RxSight) is not ideally suited to MSICS because shifts in astigmatism can occur up to 6 months or later following surgery.

P. DEE STEPHENSON, MD, FACS
The patient cannot pinpoint the exact onset of the decline in vision in her left eye. She reports no pain, discomfort, flashes, floaters, or symptoms suggestive of color distortion. The presentation discloses no known history of amblyopia, muscle imbalance, trauma, or prior ocular surgery involving the left eye, and there is no stated family history of age-related macular degeneration, glaucoma, or other hereditary retinal conditions.
Records from the earlier cataract procedure would be reviewed, with particular attention paid to the refraction, fundus findings, and A-scan measurements. This information is critical to ruling out anisometropia and other binocular considerations that could affect postoperative management. Because the dense cataract obscures a view of the posterior segment, a full evaluation would be conducted to confirm the absence of retinal and optic nerve diseases.
Pupillary testing would be performed to determine if an RAPD is present, which would suggest a compromised optic nerve or significant retinal dysfunction. Due to the mature cataract, the fundus is not adequately visible on direct ophthalmoscopy. After pupillary dilation, an attempted indirect ophthalmoscopic exam revealed only limited details. B-scan ultrasonography would therefore be performed to help rule out conditions such as retinal detachment, vitreous hemorrhage, and intraocular masses that might be masked by the dense lens opacity. A potential acuity meter could be used to better estimate the eye’s visual potential. Together, these approaches would help predict how much visual function might be recovered postoperatively, particularly helpful information because the fundus cannot be visualized. If uncertainty persists regarding retinal function, an electroretinogram would be obtained to assess photoreceptor response.
Because optical biometry is not feasible, ultrasound biometry (A-scan) would be performed to measure the axial length and facilitate IOL power selection. Given the amount of corneal astigmatism, a toric IOL merits consideration, but the final decision would depend on the biometric data and, ideally, intraoperative aberrometry. Specular microscopy would be performed to assess endothelial cell density, an important factor in long, complex cataract procedures. Glare testing might help quantify the impact of the cataract on visual function and assist with patient counseling.
I would lean toward standard phacoemulsification in this situation. Given the density of the lens, trypan blue dye would be instilled to enhance visualization of the anterior capsule during the capsulorhexis. Laser cataract surgery, however, could be an option. Currently available femtosecond laser platforms allow rapid docking and treatment and can be used to create a precise capsulotomy and custom lens fragmentation patterns, potentially reducing the amount of phaco energy required and making lens removal smoother.

WHAT I DID: CRISTOS IFANTIDES, MD, MBA
The density of the cataract made it difficult to determine the visual potential of the eye. I typically ask patients like this one whether they ever had a better or good eye and a worse or bad eye when they were growing up. This information gives me a better understanding of the degree of amblyopia that might have been present. I also test for entoptic phenomenon and ask patients whether they see a similar tree branch shape in both eyes when I shine a transillumination light through their closed eyelid and move the globe around gently. This acts like a quick and dirty electroretinogram that gives me a coarse estimate of retinal potential. I use the analogy of a house with a dirty window to explain my inability to predict visual potential with certainty. “If someone inside the house can’t see out of it,” I say, “then someone standing outside of the house can’t see inside, either, and I can’t tell you how the inside of the house is looking until after we remove the cataract.” I often use both A- and B-scan ultrasonography to ensure that cataract surgery is worth undertaking and IOL measurements can be obtained.
Given the hard cataract, I performed MSICS. Because the astigmatism was against the rule, I made the cataract incision temporally to flatten the steep plane. Although one-piece PMMA lenses are excellent in situations like this one, I typically must place a special order for them. I therefore implanted a three-piece IOL (SofPort lens, model LI61SE, Bausch + Lomb) from stock that my practice has on consignment in case a surgical plan changes. Postoperatively, the patient’s UCVA was 20/30+2 OS.




