
It is an exciting time to be a refractive surgeon. Gone are the days that we counseled patients on the differences between two corneal laser-based procedures, LASIK and PRK, to correct their refractive error. And gone are the days of surgeons having to tell some patients that they were not good candidates for refractive surgery due to their thin corneas, suspicious topographies, dry eye disease (DED), or other corneal irregularity.
Today, a variety of additional options are available, including SMILE, epi-Bowman keratectomy, refractive lens exchange, refractive cataract surgery, and phakic IOLs, which have helped us to expand the indications and the population of patients we can treat. Now, almost every patient is a candidate for refractive surgery. And now more than ever before, we can truly select the right procedure for the right patient.
This article focuses on phakic IOLs and emphasizes the clinical guidelines and best practices that can help surgeons to find success with this versatile form of refractive correction.
SUGGESTED CLINICAL GUIDELINES
In the early history of phakic IOLs, the trend was to offer this option to patients who were not good candidates for laser vision correction (LVC). In some practices, this approach is still used; in my opinion, however, it limits the use of a great procedure. Phakic IOLs should not be viewed as an alternative to LVC but rather as a great option in our toolbelt for refractive correction in those patients who are good candidates for the procedure.
Phakic IOLs offer certain advantages over other refractive correction techniques. They do not require corneal tissue removal, as LVC does; they are removable in case of any potential complication or a patient’s future surgical needs; and they have been shown to provide better visual quality in some patients, with fewer aberrations and dysphotopsias.1 Phakic IOLs also avoid potential side effects of LVC including induced DED.
In the United States, two phakic IOL models are available, the Visian ICL (STAAR Surgical) and the Verisyse (Johnson & Johnson Vision). My experience is with the Visian ICL, which is indicated for the treatment of -3.00 to -20.00 D of myopia with up to 4.00 D of astigmatism in phakic patients between the ages of 21 and 45 years. The recent approval of the toric ICL further expands our ability to treat all patients as potential refractive surgery candidates. Eyes must have an anterior chamber depth of at least 3.0 mm, an anterior chamber angle of at least grade 3, and endothelial cell density of at least 2,000 cells/mm2 to be candidates for the procedure.
PERSONAL PREFERENCES
In our practice, I automatically consider the ICL for patients with -6.50 D of myopia or more. And in patients with -4.00 to -6.50 D of myopia, we discuss the phakic IOL alongside other refractive surgery options, ultimately selecting the procedure that is best for the individual patient. Patients in that range could do well with either phakic IOLs or LVC. Below -4.00 D, I tend to suggest LASIK or another corneal laser refractive surgery procedure.
For any patient with suspicious topography, severe DED, or other ocular condition that is a contraindication for LVC, a phakic IOL is considered. We educate such patients that their corneas may continue to change over time, and that for them, the phakic IOL is a safer, more reliable procedure.
ADVICE FOR GETTING STARTED
As with any new procedure, initially there will be a learning curve—but this should not keep you away from implementing phakic IOLs in your practice. A stepwise approach to introducing the technology can help set you up for success.
A good place to begin for those who are just getting started with phakic IOLs or those who are interested in expanding their surgical offerings to include lens-based refractive correction is with patients who have suspicious topographies (eg, thin or irregular corneas) and severe DED. From there, you can add patients with high myopia, and then gradually increase the diopter range to include moderate and even low myopia. Studies have shown that phakic IOLs can be used to correct low myopia as well as they correct high myopia.2,3 And, with the recent FDA approval of the Visian Toric ICL, astigmatism management is also safe and effective. ICL repositioning, if required, is easily achieved.
BEST PRACTICES
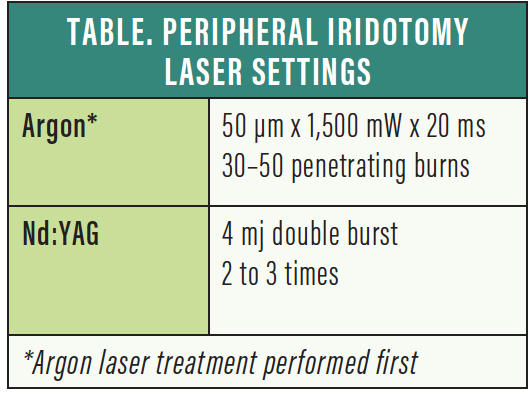
Currently in the United States, a peripheral iridotomy (PI) is required with phakic IOLs to prevent pupillary block and acute glaucoma. A PI is typically created with an Nd:YAG laser before phakic IOL surgery or during the implantation procedure. My preferred method for creating PIs is to use an argon laser in combination with the Nd:YAG laser. The argon laser helps reduce the risk of bleeding, makes it less painful for the patient, and makes the PI much more predictable. With this technique, I can also perform the procedure successfully without the use of an iridotomy lens, which makes it much more comfortable for the patient and for the surgeon. My laser settings can be found in the Table.
Another point I would like to make is that we should not recommend just one procedure or even one type of procedure to our patients. Each refractive surgery procedure has its place in our armamentarium, and each can provide the right patient with excellent long-term outcomes and life-changing value. It is therefore best practice to educate patients on all their options, and then to help guide them toward selecting the one that is best for them. We must consider what is in the best interest of our patients and counsel them accordingly.
For a long time, the cost differential between ICL surgery and LVC was substantial, and this was a barrier to patient adoption of phakic IOLs. We recently incorporated a lens-based in-office surgery suite to our practice, and it has been a complete game-changer. It has reduced our costs significantly, which we then pass on to the patient. This allows our patients to choose the best option for them based on their preference and not on price.
Refractive Surgery in a Keratoconic Eye: Phakic IOLs Were the Best Fit
By Andrea Russo, MD

The demand for refractive surgery increased in my practice after the COVID-19 lockdown. One of the reasons for this rebound effect is our patients’ need to wear masks during the pandemic. The consequent fogging of glasses experienced by many patients has inspired them to seek refractive surgery.
Interestingly, many of these patients had previously undergone a refractive surgery evaluation and were found not to be good candidates for reasons including keratoconus or ectasia risk, thin corneas, high prescriptions, or tear disorders. Many of these patients are candidates for phakic IOLs, and these are the ones now expressing the greatest preoperative enthusiasm and postoperative satisfaction. The only drawback for me with this group of patients is removing their “inoperable” label, therefore contradicting the previous opinion they had received from another ophthalmologist.
I recently counseled a patient with keratoconus who desired refractive correction. After a detailed conversation (see the sections Advantages of Phakic IOLs and Addressing Concerns), we decided that phakic IOL implantation was the best chance this patient had to achieve spectacle independence.
ADVANTAGES OF PHAKIC IOLS
At least here in Italy, most patients are aware only of laser vision correction (LVC) as a refractive surgical option. The idea of a lens inside their eye is therefore frightening at the beginning. In these cases, I spend extra time explaining the procedure and highlighting the advantages of the Visian ICL (STAAR Surgical) over LVC.
In particular, I show an animation of the procedure, available from Rendia. During the video, I describe the positioning of the ICL behind the iris, and I explain that the procedure is fast, usually taking no more than 5 minutes per eye. I note that the recovery time is comparable to, if not faster than, recovery from LASIK.
ADDRESSING CONCERNS
Still, one of the main concerns expressed by patients is the presence of a lens inside the eye. “What if I rub my eyes, or if something hits the eye?” I reassure them that these lenses are not rigid but rather extremely soft, and they can go back to their normal lives with confidence. I add that ICLs are routinely implanted in US Army personnel, a further guarantee of their quality and safety, and I mention the potential reversibility of the procedure.
It is often noted that LVC is less invasive than phakic IOL implantation. Particularly for this group of patients, however, I sometimes consider a reversible and upgradable phakic IOL to be less invasive than a definitive laser treatment—especially for a patient who would be left with minimal residual stromal thickness not allowing future enhancements.
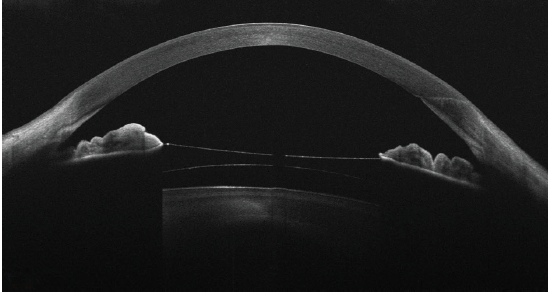
Figure. Representative OCT scan of an eye with keratoconus implanted with an ICL.
Further, I am often asked by young patients, “What if my prescription changes over time?” Our eyes are living organs, and we can never be sure about the stability of an individual’s prescription, especially those with medium to high myopia. This is why I prefer phakic IOLs, which leave all the surgical options on the table for the future if a prescription changes. This flexibility is met with a sigh of relief from my patients.
AN EXCELLENT OUTCOME
In the case of the keratoconus patient mentioned at the outset of this article, CXL was first performed to stabilize the ectasia. After following the patient for 12 months and confirming corneal stability, a toric ICL was implanted. The resultant postoperative visual acuity was 20/20, and the patient was extremely happy with his outcome.
Andrea Russo, MD
- Founder, Brescia Eye Center, Brescia, Italy
- dott.andrea.russo@gmail.com
- Financial disclosure: None
CONCLUSION
Phakic IOLs are growing in market share, and today they represent an excellent option for premium refractive correction. With the clinical guidelines outlined here and a gradual and stepwise approach to implementation, surgeons can enjoy great success with phakic IOL technology. Keeping in mind that the proper way to counsel patients is to inform them of all their surgical options, phakic IOLs can play an integral part in the success of progressive refractive surgery practices.
1. Parkhurst G. A prospective comparison of phakic collamer lenses and wavefront-optimized laser-assisted in situ keratomileusis for correction of myopia. Clin Ophthalmol. 2016;10:1209-1215.
2. Alfonso JF, Baamonde B, Belda-Salmerón L, Montés-Micó R, Fernández-Vega L. Collagen copolymer posterior chamber phakic intraocular lens for hyperopia correction: three-year follow-up. J Cataract Refract Surg. 2013;39(10):1519-1527.
3. Kamiya K, Shimizu K, Igarashi A, et al. Posterior chamber phakic intraocular lens implantation: comparative, multicentre study in 351 eyes with low-to-moderate or high myopia. Br J Ophthalmol. 2018;102(2):177-181.




