Refractive accuracy in cataract surgery is increasingly important. Patients expect to obtain excellent visual acuity and quality after surgery, and the margin for error is narrowing. Achieving a postoperative result within ±0.50 D of the intended refractive target is typical in most normal eyes, but certain types of eyes present challenges. This article discusses several strategies that can help to maximize outcomes in difficult eyes and offers tips for simplifying IOL selection in these cases that go beyond merely selecting the appropriate lens calculation.
THE BASICS
The most important thing we can do as refractive cataract surgeons is to conduct a meticulous preoperative examination in every eye. Obtaining highly accurate measurements is the key to nailing the postoperative refraction. This starts with accurate diagnostic testing. I use the Argos Biometer With Image Guidance (Alcon) and the IOLMaster 700 (Carl Zeiss Meditec) for every eye, and I compare the results with both devices. If the measurements do not match, I like to use the ORA System With VerifEye (Alcon) as a third device to confirm the most appropriate IOL power intraoperatively. For surgeons with only one device, I suggest repeating measurements to ensure accuracy and making sure the cornea is well lubricated. The imaging software with the two biometers I use captures images quickly, so dryness is less of an issue than with older biometers.
The most difficult eyes in which to obtain accurate measurements and to calculate IOL power include short and long eyes, postrefractive surgery eyes, eyes with poor ocular surface health, and eyes with dense cataracts. For this last group, I prefer to use the Enhanced Retinal View (ERV) mode on the Argos biometer because it can penetrate even the densest cataracts, including grade 4 cataracts, and provide an accurate prediction of the IOL power. When the Argos with ERV is not available, manual A-scan biometry can be used. This method, however, tends to produce more variable measurements.
The Argos has an extremely fast (< 1 second) capture time and scanning speed. This helps us reduce our patient-technician contact time—a consideration that is especially important for current social-distancing efforts. Overall, with the Argos, a typical biometry examination is about 5 minutes, and typical A-scan biometry requires about 15 minutes (data on file with Alcon). The ERV is an optional setting on the Argos, so the technician must enable it before the acquisition of the measurement.
Of course, a good IOL formula is also important. I predominantly use the Barrett Universal formula.
OTHER CONSIDERATIONS
Patient personality is a huge factor to consider when selecting an IOL, especially in difficult eyes. Some patients are more willing than others to tolerate trade-offs in visual quality or subtle side effects if they can achieve excellent vision at a certain range. Others, however, will be unhappy if their vision is anything less than perfect. Of note, I have found that even particular patients do well with a trifocal IOL because it delivers consistent refractive outcomes at near (16 inches), intermediate (24 inches), and far.
About 5 years ago, surgeons started to be better at matching patients with the best IOLs for them. Patient counseling is crucial to this endeavor, but the most consistent lens outcome for me has been with the AcrySof IQ PanOptix trifocal IOL (Alcon).
It is also important to examine the ocular surface before cataract surgery. Eyes with dry eye disease, for example, can present with false astigmatism on the preoperative examination. This increases the risk of selecting the wrong toric IOL power and overtreating the astigmatism.
HITTING THE REFRACTIVE TARGET
Cataract surgeons have gotten better at hitting the refractive target more consistently, even in difficult eyes. The reason for this is threefold.
No. 1. The latest biometry devices provide more reproducible and consistent measurements than previous generation devices. These measurements can also be shared seamlessly between devices through the cloud, eliminating transcription errors and reducing the risk of inaccurate IOL powers. Both the Argos and IOLMaster 700 provide consistent and predictable outcomes in normal eyes.
No. 2. These devices are more powerful and can therefore penetrate even the densest cataracts and obtain accurate measurements in the most challenging and difficult eyes (see Case Study).
Case Study
A 59-year-old man with a grade 4+ nuclear sclerotic and white posterior subcapsular cataract (Figure 1) presented with very poor vision. The patient had a history of myopic LASIK in both eyes and expressed interest in laser cataract surgery.
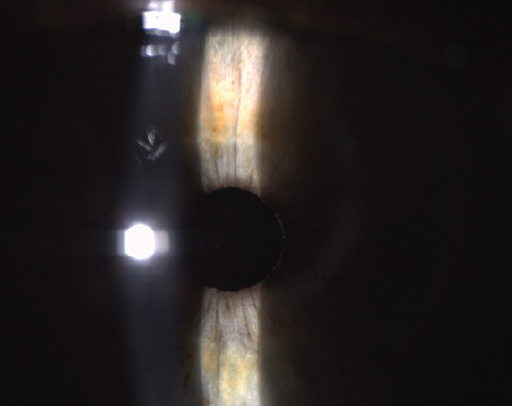
Figure 1. Preoperative image showing a grade 4+ nuclear sclerotic and white posterior subcapsular cataract.
Preoperatively, biometry was performed with the Argos (Alcon) and IOLMaster 700 (Carl Zeiss Meditec). Both devices were able to penetrate the dense cataract, and both adjusted the IOL calculation to compensate for the prior myopic LASIK treatment. The predicted postrefractive outcome was less than or equal to 0.50 D.
I discussed with the patient his options, which included the AcrySof IQ Vivity and AcrySof IQ PanOptix IOLs (both from Alcon). Because he had experienced minimal nighttime vision symptoms before the onset of his cataract and had minimal astigmatism, we decided the best option for him was the bilateral implantation of a PanOptix IOL. On postoperative day 1 (Figure 2), visual acuity was 20/20 OU, J1+ at near, and J1 at intermediate.
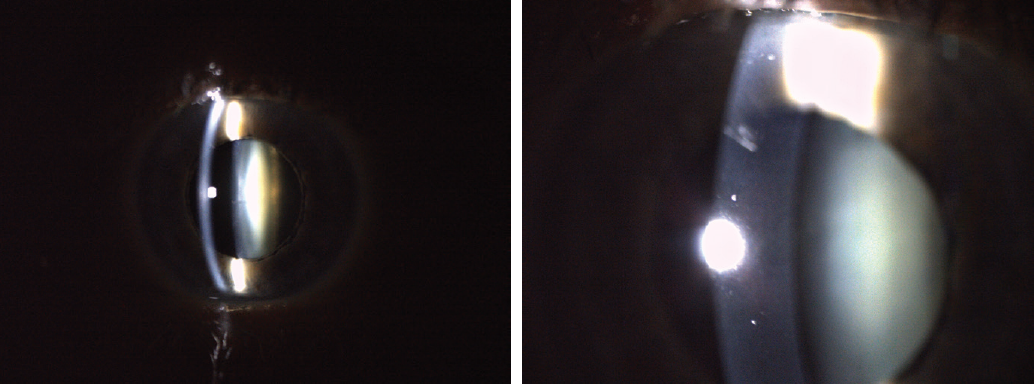
Figure 2. Postoperative day 1 images showing an AcrySof IQ PanOptix IOL in situ with a clear cornea.
No. 3. Devices such as the Argos have a variety of IOL formulas built-in and allow operators to toggle between them in order to decide which formula will provide the most accurate refractive result. This is especially important because I am seeing a lot more patients with a history of myopic LASIK who are now of cataract age. I find myself going to the ASCRS online calculator infrequently (if ever) now that I have the Argos. In the future, I envision that this and other devices will incorporate AI data into IOL calculations.
CONCLUSION
Proper IOL selection in difficult eyes is more than simply using the right IOL formula. Postoperative results within ±0.50 D of the intended refractive target are achievable, even in difficult eyes, when a meticulous preoperative examination, consideration of patient personality, and proper patient counseling are incorporated into the surgical planning process.