Advances in cataract and refractive cataract surgery—including surgical techniques and IOL technologies—have expanded the options for improving patients’ vision. Part of being an excellent, comprehensive, and, most importantly, prepared cataract surgeon is anticipating possible complications during and after surgery, avoiding these complications, and knowing how to handle them properly should they occur.
Dislocation, inadequate rotation or misplacement, and decentration of an IOL are important considerations in the pre-, peri-, and postoperative periods, especially in high-risk patients. Careful preoperative scrutiny of the patient’s anatomy allows the surgeon to make an educated decision on whether the patient is a good candidate for certain premium IOL technologies and whether there is an increased risk of IOL dislocation (eg, history of trauma, zonulopathy, pseudoexfoliation). This article provides advice on managing three common complications that may arise with cataract surgery.
DISLOCATED IOL
An IOL may become dislocated at any time during the postoperative period (Figure). One key to the management of this complication is taking a careful patient history. Was zonular loss observed, or did the posterior capsule tear during surgery? Is dislocation due to trauma that occurred years after cataract surgery? The second key is the postoperative examination. Where is the IOL located (eg, inside or outside of the capsular bag, in the vitreous cavity)? What type of IOL is it? Management differs for one- and three-piece IOLs.
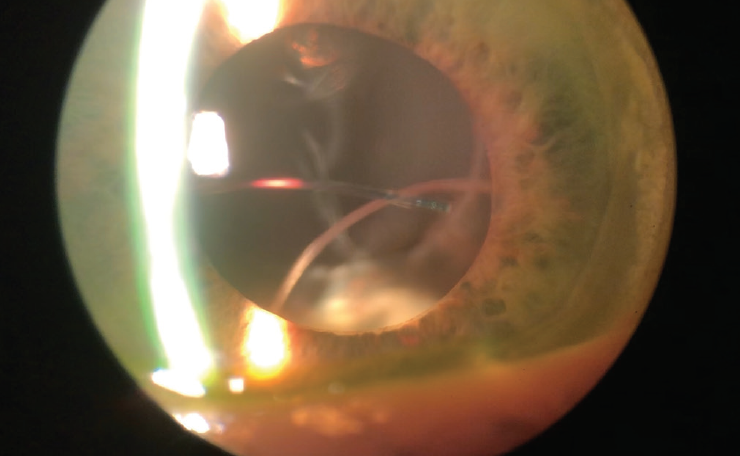
Figure. A severely subluxated three-piece IOL in an eye with diffuse zonular loss. An outside surgeon attempted to place a three-piece IOL in the sulcus with little zonular support.
If the dislocation is severe (ie, the IOL is mostly in the vitreous cavity), it is imperative to consult and work with a retina surgeon to ensure the safe explantation and/or fixation of the IOL. Some skillful retina surgeons are able to bring a three-piece IOL forward from the vitreous cavity and perform scleral fixation without having to explant and exchange the lens.1,2 The availability of this option, however, depends on other factors.
Factor No. 1. If there is retinal damage, it may be safest to explant the IOL and treat the retinal issues before inserting a new IOL.
Factor No. 2. If the IOL dislocated many years after implantation, scleral fixation may not be possible because of the fragility or instability of the IOL haptics.
Factor No. 3. If the anterior capsule is intact and at least part of the IOL is retrievable from within the posterior chamber, it may be possible to reverse optic capture a three-piece IOL and/or to bring it out of the capsular bag and reposit it in the ciliary sulcus.1 This may or may not require an anterior or posterior vitrectomy at the time the IOL is repositioned. Exquisite care must be taken not to damage remaining capsular and zonular support.
Factor No. 4. If a one-piece IOL has dislocated and the anterior capsule is not intact, the best option is to explant it and plan for a secondary IOL (scleral-fixated, iris-sutured, or even an anterior chamber IOL) at a later date.
A lengthy preoperative discussion with the patient is warranted. It should provide details on surgical risk, including the surgeon’s possible inability to successfully implant and secure an IOL due to dislocation. It is important to emphasize that additional surgery and visual refinement may be required at a later date.
MISALIGNED TORIC IOL
Despite technological advances, a slight risk of postsurgical rotation of a toric IOL remains. This should be discussed with patients preoperatively. Some patients, such as those with high myopia and keratoconus, may be at increased risk of IOL malrotation because of their ocular anatomy. Additionally, a residual amount of an OVD in the capsular bag at the time of surgery may destabilize the IOL and lead to unplanned rotation.
Precise alignment of a toric IOL is important. The correction of astigmatism decreases by 3.3% with every 1º of error in alignment. Each 10º of misalignment therefore produces a 33% loss of toric correction.3,4
If misalignment of a toric IOL is noted early in the postoperative period, the optimal time to reposition the IOL surgically is approximately 1 to 2 weeks postoperatively.3,4 That said, most toric IOLs can be rotated without significant risk within the first 3 to 6 months postoperatively.3,4
Before returning to the OR, important considerations include the extent of misalignment and if a secondary support device such as a capsular tension ring may be helpful in maintaining correct alignment.1,3,4 Informed consent should address the possibility of inadvertent damage to the capsular bag and the possible need (albeit rare) for IOL explanation at the time of repositioning. Keratometry readings, refraction, and IOL position relative to the planned axis should also be reviewed. I suggest using www.astigmatismfix.com, a helpful resource created by John P. Berdahl, MD, and David R. Hardten, MD, FACS, to calculate the degree of rotation required at the time of secondary surgery.3,4 In concert with this, intraoperative aberrometry may prove helpful to determine the degree of misalignment during surgery and confirm proper alignment at the end of the case.
DECENTERED DIFFRACTIVE IOL
Diffractive (bifocal, trifocal, and extended depth of focus) IOLs can address the lifestyle concerns of presbyopia. Because of their design, however, decentration can lead to unwanted visual aberrations and side effects and suboptimal visual acuity.5,6 The assessment of a patient with a decentered diffractive IOL should address two questions.
Question No. 1: Where is the IOL centered on examination? Slight decentration of an IOL with respect to the pupil is common because the pupillary center is nasal to the optical center of the eye.6 If an IOL is noted to be slightly decentered during the first postoperative week and vision is compromised, it is possible to push the lens nasally to the center of the pupil intraoperatively, but this requires a trip back to the OR.5,6
Question No. 2: Is the IOL–capsular bag complex dislocated? If the entire capsular bag–IOL complex is decentered, perhaps because of pseudoexfoliation or trauma, informed consent must address the possible need for IOL explantation and exchange depending on zonular support.5-7 In the unfortunate case of IOL–capsular bag dislocation, surgical management is necessary to permit realignment and centration of the IOL. Oftentimes, minimal zonular laxity noted at the time of surgery can be successfully addressed with the insertion of a capsular tension ring.7 If the degree of zonulopathy is great, however, a scleral-fixated capsular tension segment may be used to center the capsular bag and IOL.7-9 In the right hands, this procedure can produce successful results, but there is still a chance that the diffractive IOL will remain slightly off-center and visual aberrations such as glare and halos may result.
In the case of severe capsular bag dislocation that cannot be adequately addressed and recentered surgically, it may be necessary to explant the entire capsular bag–IOL complex (usually in combination with vitrectomy) and to place a secondary IOL at a later date. In the United States, only one-piece diffractive IOL technologies are available, so the patient must be informed that an IOL exchange would involve the implantation of a monofocal IOL, which may necessitate the use of glasses for intermediate and near activities.
CONCLUSION
Addressing the why and how of an IOL complication assists with the formulation of a treatment strategy for each individual eye and patient.
1. Gross JG, Kokame GT, Weinberg DV; Dislocated In-The-Bag Intraocular Lens Study Group. In-the-bag intraocular lens dislocation. Am J Ophthalmol. 2004;137(4):630-635.
2. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-1142.
3. Holland E, Lane S, Horn JD, Ernest P, Arleo R, Miller KM. The AcrySof Toric intraocular lens in subjects with cataracts and corneal astigmatism: a randomized, subject-masked, parallel-group, 1-year study. Ophthalmology. 2010;117(11):2104-2111.
4. Kramer BA, Hardten DR, Berdahl JP. Rotation characteristics of three toric monofocal intraocular lenses. Clin Ophthalmol. 2020;14:4379-4384.
5. Salerno LC, Tiveron MC Jr, Alió JL. Multifocal intraocular lenses: types, outcomes, complications and how to solve them. Taiwan J Ophthalmol. 2017;7(4):179-184.
6. Soda M, Yaguchi S. Effect of decentration on the optical performance in multifocal intraocular lenses. Ophthalmologica. 2012;227(4):197-204.
7. Guo L, Wang C, Yang X. A novel technique for the surgical management of intraocular lens-capsular bag-capsular tension ring complex dislocation. Exp Ther Med. 2019;17(4):2785-2788.
8. Chan CC, Crandall AS, Ahmed IIK. Ab externo scleral suture loop fixation for posterior chamber intraocular lens decentration: clinical results. J Cataract Refract Surg. 2006;32(1):121-128.
9. Kirk TQ, Condon GP. Simplified ab externo scleral fixation for late in-the-bag intraocular lens dislocation. J Cataract Refract Surg. 2012;38(10):1711-1715.